RHEUMATOID ARTHRITIS:
IS A CHRONIC SYSTEMIC INFLAMMATORY ARTHRITIS .
CHARACTERIZED BY REMISSION AND EXACERBATION ,
WITH EXTRA ARTICULAR MANIFESTATIONS,
OCCURRING THROUGHOUT THE WORLD IN ALL
ETHNIC GROUPS . FEMALE : MALE RATIO IS 3:1. CAN
EFFECT ANY AGE BUT THE PEAK INCIDENCE OCCUR
WITHIN 4
TH
AND 5
TH
DECADES OF LIFE.
ETIOLOGY :
GENETICS AND ENVIRONMENTAL FACTORS
IMPLICATED CLEARLY IN THE ETIOLOGY AND
PATHOGENESIS OF RA.
GENETIC FACTORS
:
- CONCORDANCE IN MONOZYGOTIC TWINS IS 12-15% IN
COMPARE WITH 3% IN DIAZYGOTIC TWINS.
- INCREASED FREQUENCY IN 1
ST
–DEGREE RELATIVE OF
PATIENTS.
- IN UP TO 50% OF GENETIC SUSCEPTIBILITY IS DUE GENES IN
HLA REGION.
HLA DR4 IN(50-70%) IN CAUCASIAN PATIENTS COMPARE TO
20-25% IN NORMAL POPULATION.
HLA DR4 ALSO ASSOCIATED WITH PROGRESSIVE AND SEVERE
DISEASE.

NON GENETIC RISK FACTORS:
-INFLUENCE OF SEX HORMONES TWO TO THREE TIMES
ARE LIKELY TO OCCUR IN FEMALES THAN MALES.
- TOBACCO SMOKING IS STRONG RISK FACTOR FOR
ETIOLOGY AND SEVERITY AND REDUCE
RESPONSIVNESS TO DMARDS AND BIOLOGICAL
TREATMENT .
- SUSCEPTIBILITY INCREASE IN POST PARTUM AND
BREAST FEEDING PERIOD.
- ALTHOUGH IT IS THOUGHT THAT RA IS TRIGGERED BY
INFECTIOUS AGENT IN A GENETICALLY SUSCEPTIBLE
HOST , A SPECIFIC PATHOGEN HAS NOT BEEN
IDENTIFIED.

Pathology
:
* swelling and congestion of synovial membrane
•
Cellular infiltration of synovium
•
CD4 Tcells and Th17 cells play important role in
pathogenesis.
* Effusion of synovial fluid
Hypertrophy of synovial membrane
Lymphoid follicles formed in synovial tissue .B cell
to produce cytokines and autoantibodies RF and
ACPA
Synovial macrophages produce pro inflammatory
cytokines( TNF, IL-1,IL-6 and IL15) these
stimulating fibroblast to cause swelling and more
soft tissue and cartilage damage

ACTIVATION OF OSTEOCLAST AND CHONDROCYTE
AND MORE BONE AND CARTILAGE DESTRUCTION. .
-LYMPH NODE ARE OFTEN HYPERRPERPLASTIC WITH
PRODUCTION OF RF AND ACPA BY PLASMA CELLS.
.
- INFLAMMATORY GRANULOMATOUS TISSUE (PANUS)
EXTEND UNDER AND OVER ARTICULAR CARTILAGE
LEADING TO CARTILAGE AND BONE EROSION.
- LATER FIBROUS OR EVEN BONY ANKYLOSIS MAY
OCCUR.
-- MUSCLES ATROPHY
.
CLINICAL FEATURES:
-AFTER A PERIOD OF PRODROMAL SYMPTOMS
- PAIN AND JOINT SWELLING OF SMALL JOINTS OF
HANDS ,WRIST AND FEET (USUALLY SPARING THE
DIP JOINTS) USUALLY IN SYMMETRICAL FASHION
WITH MORNING STIFFNESS MORE THAN ONE HOUR.
THE INFLAMED JOINTS ARE TENDER ON PRESSURE
WITH PAINFUL RESTRICTION OF MOVEMENTS.
LARGE JOINTS INVOLVEMENT AND EXTRA
ARTICULAR MANIFESTATIONS MAY OCCUR.

ONSET:
-INSIDIOUS
-ACUTE
-MIMIC POLYMALAGIA RHEUMATICA
-PALINDROMIC RHEUMATISM

I
IF THE DISEASE IS NOT HALTED EARLY BY DISEASE
MODIFYING ANTI RHEUMATIC DRUGS (DMARD)
RESULTING IN BONE EROSIONS , ARTICULAR
DESTRUCTION , LIGAMENT AND TENDON LAXITY OR
CONTRACTURES CAUSING CHARACTERISTIC
DEFORMITY.
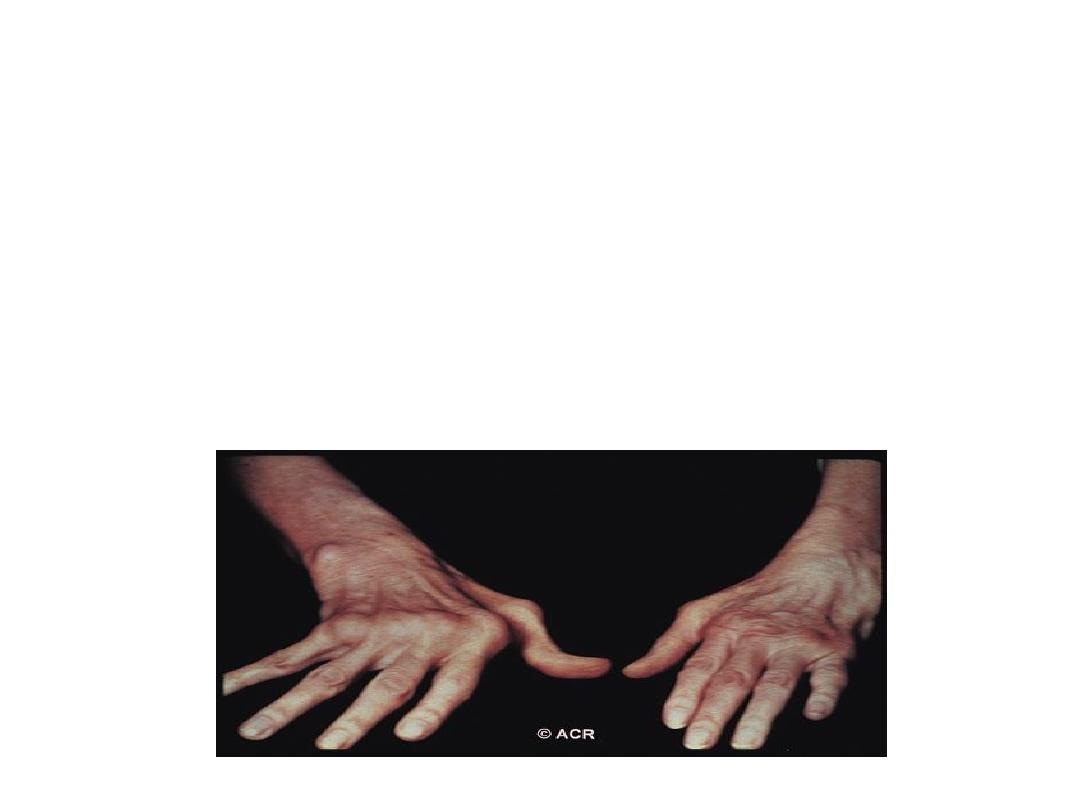
HAND
JOINTS
Swelling of proximal
interphalangeal
(fusiform)
and metacarpophalangeal
joints. The distal
interphalangeal joints are
rarely involved "usually
spared".
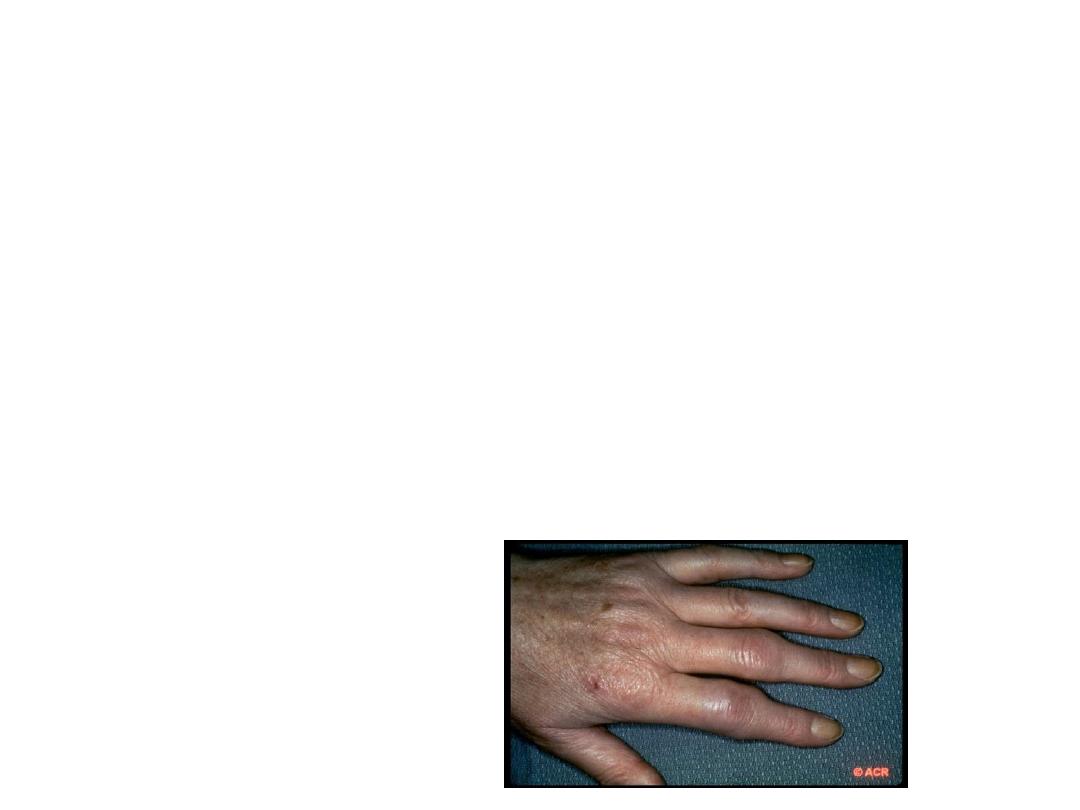
Synovitis of the wrist usually
uniform feature of RA,
may lead to limitation of
movement, Dorsal
subluxation of ulnar
styloid is common and
may contribute to
rupture of the 4th and
5th extensor tendon.
Median nerve
entrapment can be
occur.
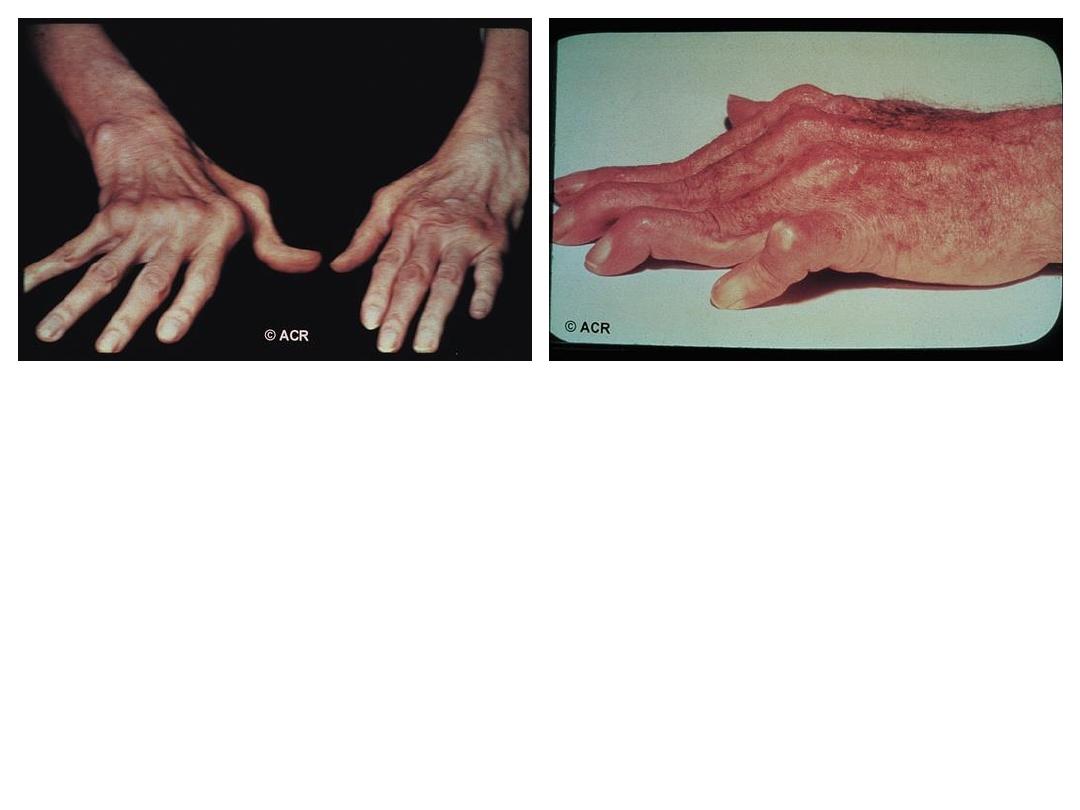
* Radial deviation at the wrist. Ulnar deviation
of MCP joints.
* Swan neck deformity.
* Boutonniere deformity.
* (Z) deformity of the thumb.
* Triggering of finger may occur due to nodules
formation in flexor tendon sheath.
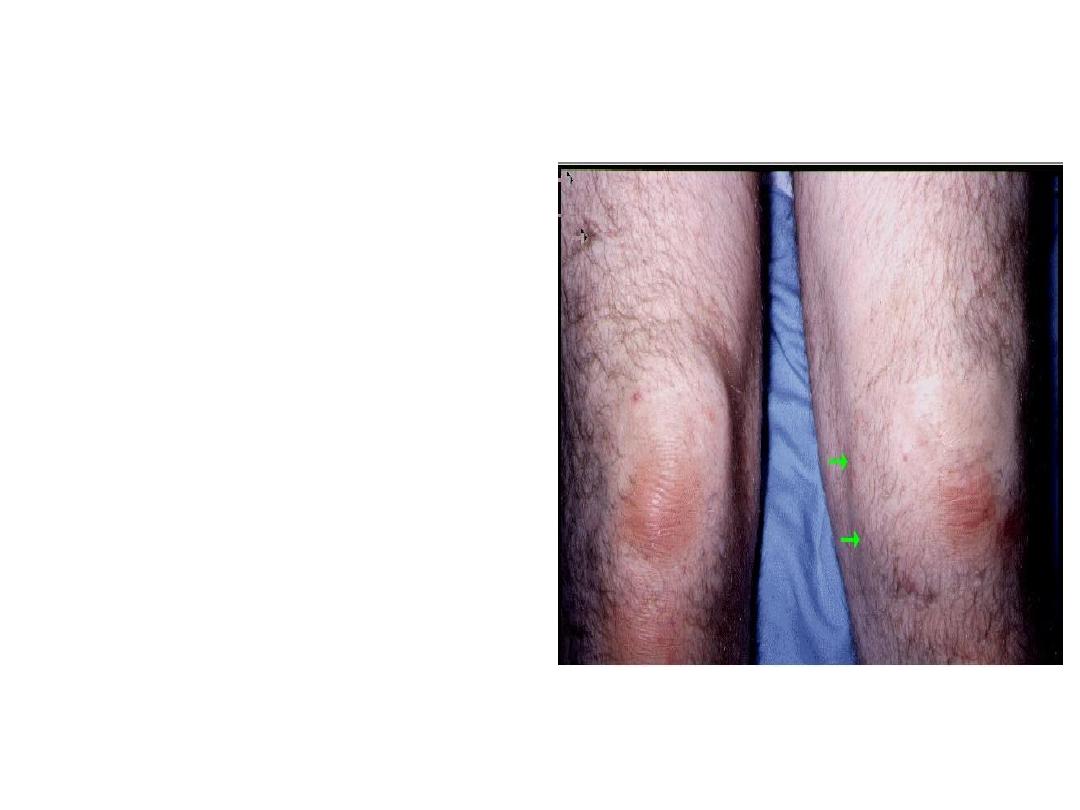
Knee joint
Is commonly involved
with synovial
hypertrophy, chronic
effusion
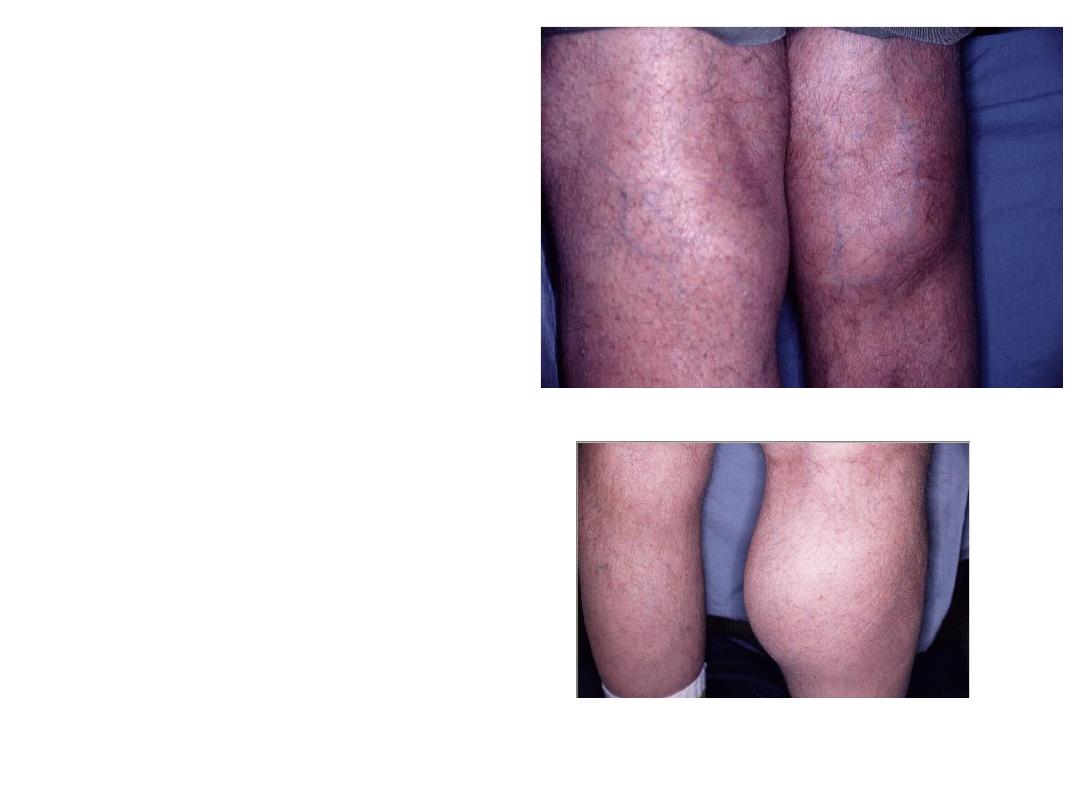
Popliteal (Baker's) cyst
,with knee synovitis
and the synovial fluid
communicating to
cyst in valve- like
mechanism
preventing the fluid to
return back to joint
cavity. Rupture of cyst
producing picture
similar to DVT
Characteristic pre-
existing history of joint
problem. Doppler
ultrasound study is
required to establish
the diagnosis.
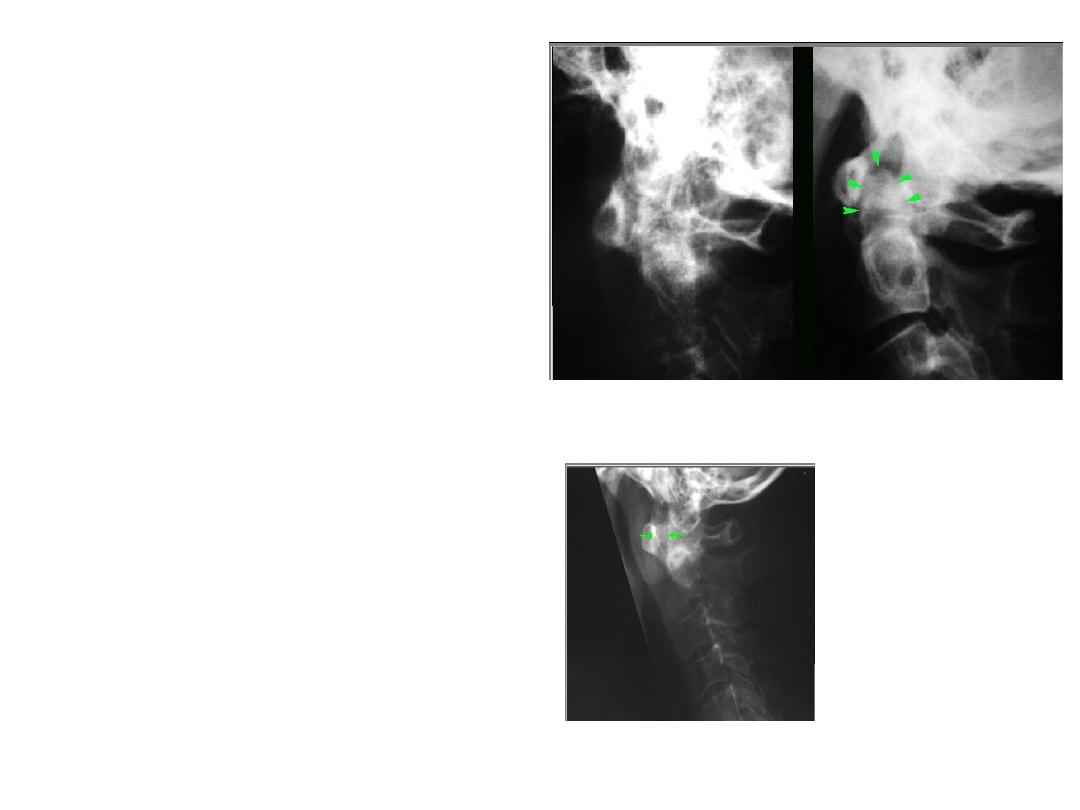
Cervical spine:
*Atlanto-axial
subluxation
*Spinal cord
compression
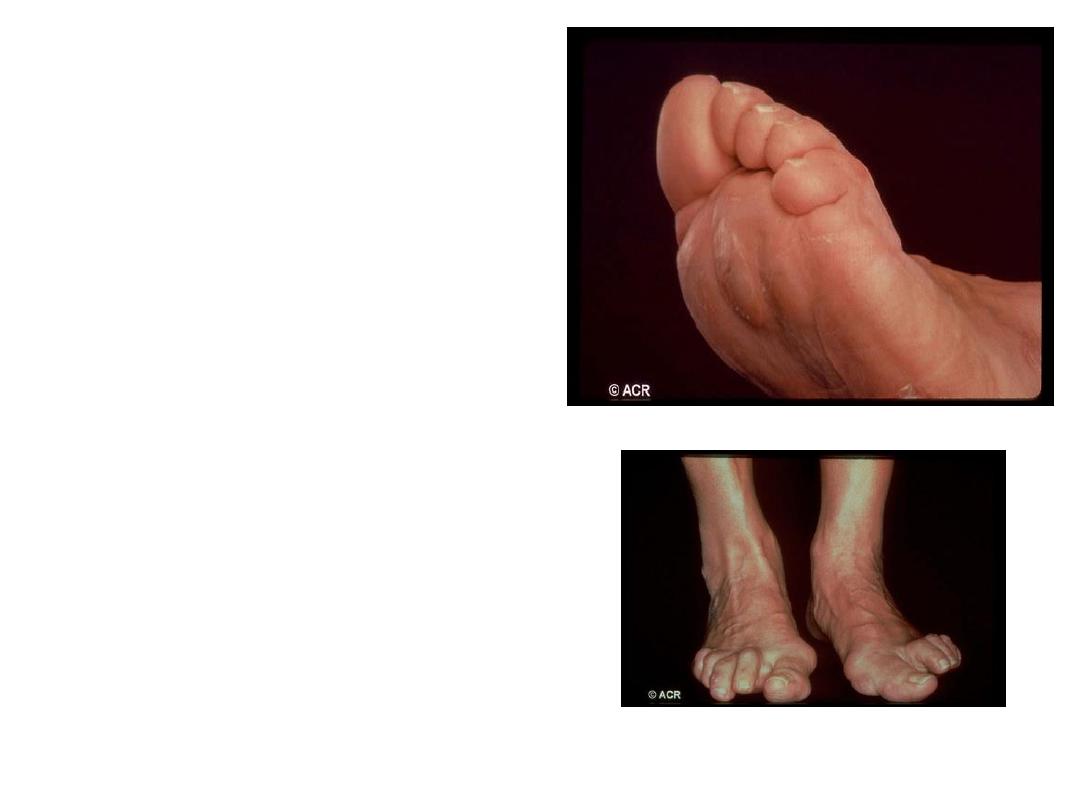
Foot & Ankle
Eversion.
Dorsal sub luxation of MTP
joint may result in Cock-
up toe deformity.
Painful burse and
Callosities.
Flat foot due to rupture
of the tibialis
post.tendon.
Hallux valgus.
.

EXTRA ARTICULAR MANIFESTATIONS
:
OCCUR MAINLY IN LONG-STANDING
SEROPOSITIVE EROSIVE DISEASE.
- WEIGHT LOSS, ANOREXIA, GENERALIZED
OSTEOPOROSIS, WASTING OF MUSCLES DUE TO
SYSTEMIC INFLAMMATION.

CUTANEOUS
AND VASCULAR FEATURES
:
RHEUMATOID NODULES:
USUALLY OCCUR AT PRESSURE SITE SUCH AS
EXTENSOR SURFACE OF FOREARM , SACRUM,
ACHILLES TENDON.
THE NODULES ARE FIRM NON TENDER . IT
ALMOST EXCLUSIVELY OCCUR IN SEROPOSITIVE
DISEASE.

•
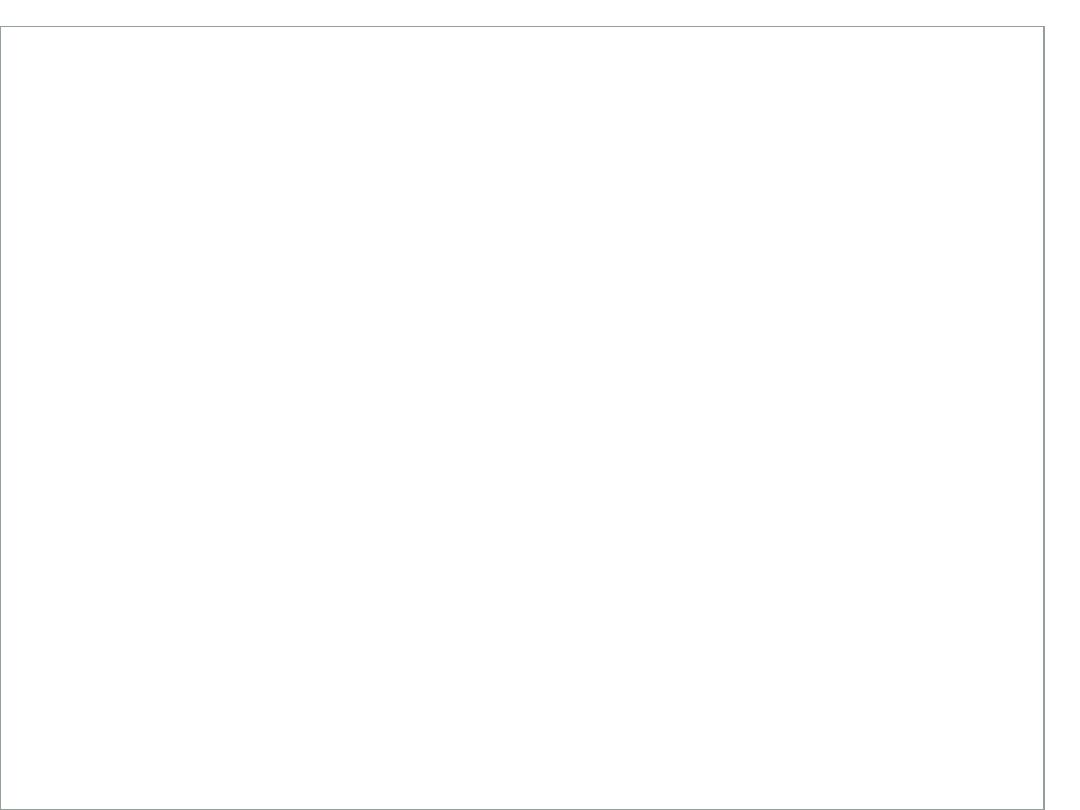
Rheumatoid vasculitis
:
occur in seropositive patients. vasculitis
ranging from benign nail-fold infarct to wide
spread ulceration and skin necrosis.
Vasculitis of medium size artery can lead to
mesentric, renal, and coronory occlusion.
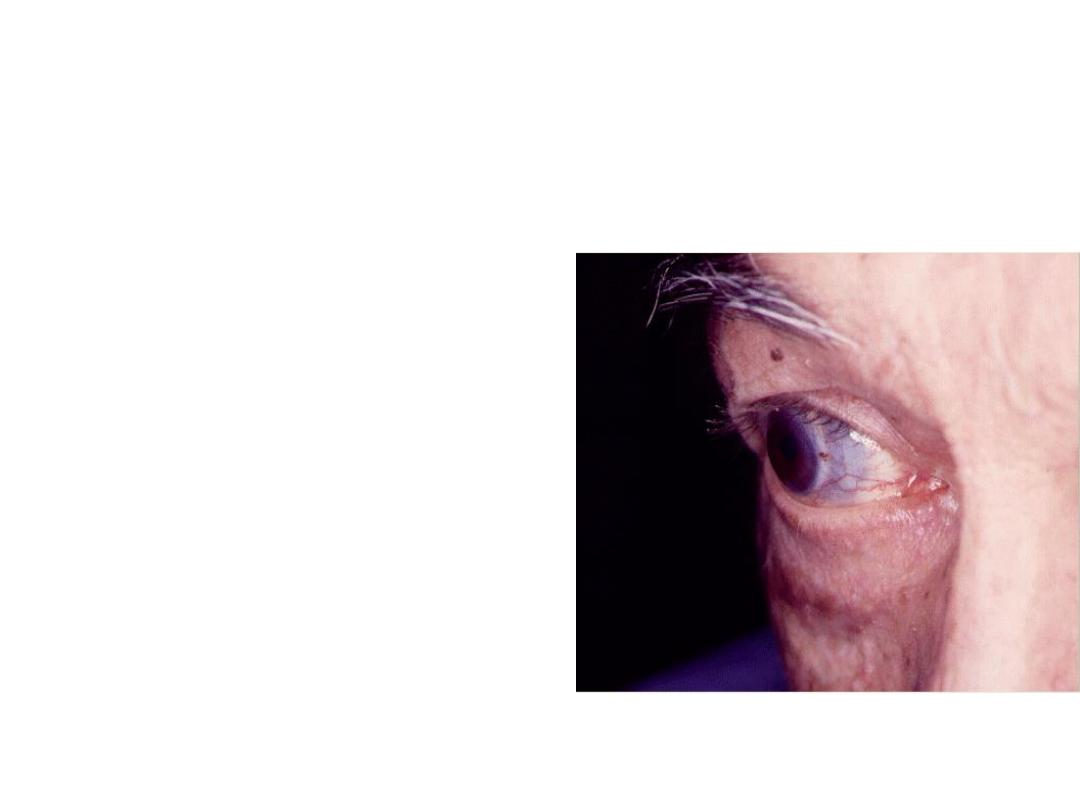
Ocular features:
*Dry eye
Keratoconjuctivitis Sicca"
secondary sjogren
disease. *Episcleritis
(painless unimpaired sight).
*Scleritis (painful and more
serious sight - threatining).
*Scleromalacia (bilateral
thinning of the sclera).
Corneal melting rare, serious,
associated with vasculitis, if
untreated , it can lead to
perforation

CARDIAC MANIFESTATIONS
:
OCCUR UP TO 30%USUALLY ASYMPTOMATIC.
SYMPTOMATIC PERICARDIAL EFFUSION AND
CONSTRICTIVE PERICARDITIS ARE RARE.
HEART BLOCK, CARDIOMYOPATHY, CORONARY ARTERY
OCCLUSION OR AORTIC REGURGITATION CAN OCCUR.
ACCELERATED ATHEROSCLEROSIS ALSO OCCUR.
PATIENTS WITH RA HAVE AN INCREASED MORTALITY
WHEN COMPARED WITH AGE-MATCHED CONTROLS,
PRIMARILY DUE CARDIOVASCULAR DISEASE
FURTHERMORE THE NSAIDS AND CORTICOSTEROID
EXACERBATE CARDIAC DISEASES.

Pulmonary features
[Rheumatoid lung]
•Pulmonary fibrosis • Pleural
effusion.
• Rheumatoid nodule
(pulmonary)
Bronchitis and bronhiectasis are
common in RA..
•
Rarly potentially fatal
oblitrative bronchiolitis may
occur .
•
Bacterial infection especially
those on cortico steroid.
•
Pulmonary fibrosis may
caused by methotrxate.
•
Anti TNF therapy associated
with TB reactivation..

NEUROLOGICAL COMPLICATIONS
:
-
ENTRAPMENT NEUROPATHY . COMPRESSION
OF MEDIAN NERVE IS COMMON (CARPAL
TUNNEL SYNDROME). ULNAR NERVE
COMPRESSION AND TARSAL TUNNEL
SYNDROME CAN ALSO OCCUR.
- DIFFUSE PERIPHERAL NEUROPATHY AND
MONONUERITIS MULTIPLEX (IN RHEUMATOID
VASCULITIS)
-CERVICAL CORD COMPRESSION AT ATLANTO-
AXIAL JOINT OR SUB AXIAL LEVEL
SUBLUXATION
.

Hematological features:
-Microcytic iron deficiency anaemia (NSAID-
induced GIT blood loss).
-Normochromic normocytic anaemia,
thrombocytosis in active disease.
Felty's syndrome: constitute of: RA , splenomegaly
and neutropenia, in long standing seropositive at
age between 50-70 ,female>male, associate
with sjogren
disease,lymphadenopathy,thrombocytopenia,
recurrent infection, leg ulcer (vasculitis)

•
Other complications
:
-Amyloidosis (rare) presented as nephrotic
syndrome
-Generalized or localized
lymphadenopathy. In persistent
lymphadenopathy biopsy indicated
because there is risk of associated
lymphoma in patient in long standing
disease.
-Osteoporosis
-Ante -date or accelerated atherosclerosis
- Infections

Investigations:
The diagnosis of RA usually done on clinical
background.
The lab. Invest. is needed for confirmation of
diagnosis or for monitoring of disease
--Acute phase response. ESR and CRP are elevated and may
be not in isolated joint arthritis ..so normal values don’t
exclude the diagnosis.

--RHEUMATOID FACTOR (RF)AND ANTI CITRULINE
PEPTIDE ANTIBODIES (ACPA) ARE PRESENT IN
ABOUT(70%).
RF HAS LOW DIAGNOSTIC SPECIFICITY. THE
PRINCIPLE USE OF RF IS FOR PROGNOSIS SINCE A
HIGH RF TITER AT PRESENTATION CARRY POOR
PROGNOSIS

(ACPA) ANTIBODIES. IT IS SUPERIOR TO RF TO SUPPORT
DIAGNOSIS OF RA. IT MORE SPECIFIC. IT USUALLY
ASSOCIATED WITH MORE SEVERE, EROSIVE RA.
--INVESTIGATION TO MONITOR DRUG SAFETY:
URINALYSIS, LIVER ENZYME, S. UREA AND CREATININE ,
FULL BLOOD COUNT , CXR.

DISEASE ACTIVITY SCORE :DAS-28
IS FREQUENTLY USED TO ASSESS THE DISEASE ACTIVITY AND
RESPONSE TO TREATMENT AND THE NEED FOR BIOLOGICAL
THERAPY.
TO CALCULATE DAS- 28 :
COUNT THE NUMBER OF TENDER AND SWOLLEN JOINTS IN
UPPER LIMBS AND KNEES
• MEASURE THE ESR
• ASK THE PATIENT TO RATE GLOBAL ACTIVITY OF ARTHRITIS
DURING THE
PAST WEEK USING VISUAL ANALOGUE SCALE (VAS) FROM 0
(NO SYMPTOMS) TO 100 (VERY SEVERE)
• ENTER DATA INTO CALCULATOR OR WORK OUT USING A
SPECIAL FORMULA.

A DAS28 SCORE OF HIGHER THAN 5.1 IS INDICATIVE OF
HIGH DISEASE ACTIVITY, WHEREAS A DAS28 BELOW 3.2
INDICATES LOW DISEASE ACTIVITY. A PATIENT IS
CONSIDERED
TO BE IN REMISSION IF THEY HAVE A DAS28 LOWER THAN
2.6 .

Synovial fluid examination :shows non specific
inflammatory changes.
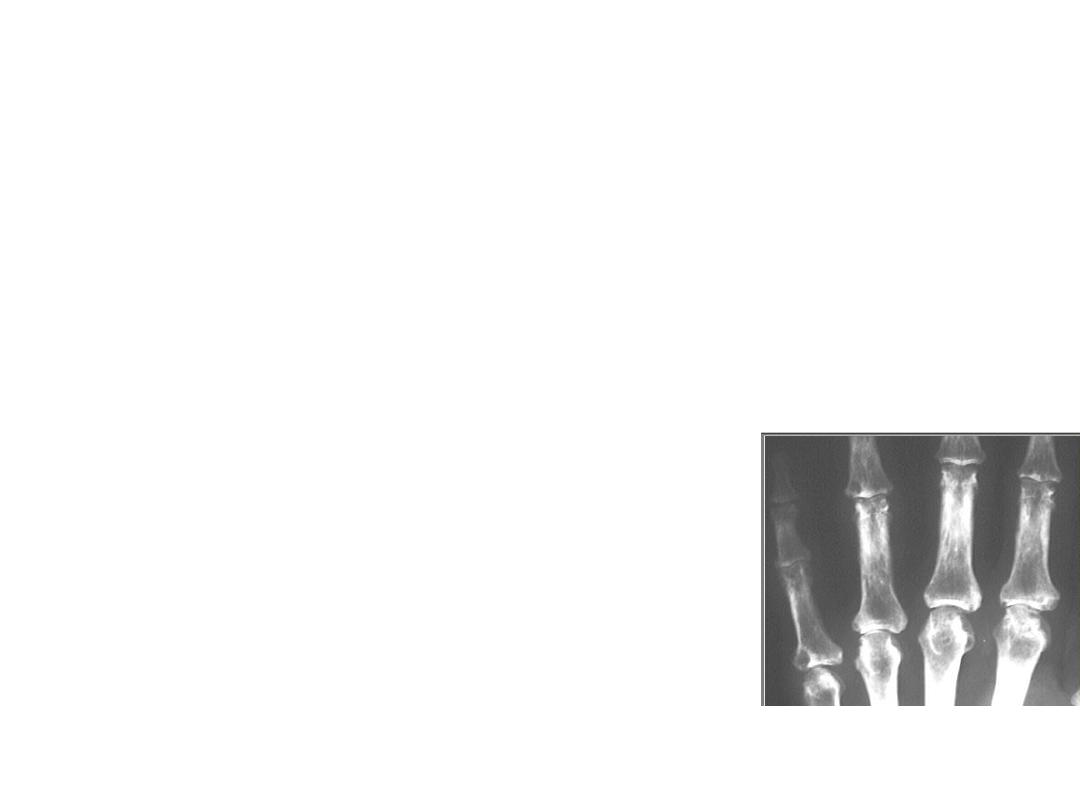
Radio graphical features:
Plain radiography: Can be normal in early stage of disease
apart from soft tissue swelling
Periarticular osteopenia.
marginal non-proliferative erosions and symmetrical joint
narrowing. Plain x-ray also used to detect atlanto-axial
or subaxial subluxation(in flexion and extension
position) where as the degree of cord compression need
MRI.

-MRI AND ULTRASOUND ARE MORE SENSITIVE IN
DETECTING EARLY EROSIONS AND WHEN UNCERTAINTY OF
SYNOVITIS .(NOT USED ROUTINELY IN CLINICAL OBVIOUS
CASES).
-ULTRA SOUND IS INDICATED IN RUPTURE OF BAKER CYST
TO CONFIRM DIAGNOSIS AND TO EXCLUDE POSSIBILITY OF
DVT AS IN SOME INSTANCES BOTH CAN CO EXIST.
the American College of Rheumatology (ACR), in
collaboration with European League Against Rheumatism
(EULAR), released the updated classification criteria
EULAR/ ACR which depend mainly on the number and
distribution of involved joints, serology, acute phase
reactants, and duration of disease , with goal of
distinguishing newly presenting patients with early
undifferentiated arthritis who had a high probability of
developing persistent or erosive RA.

The ACR/ EULAR criteria
Criterion
Score
Joint affect
1 large joint 0
2-10 large joints 1
1-3 small joints 2
4-10 small joints 5
Serology
Negative RF and ACPA 0
Low positive RF or ACPA 2
High positive RF or ACPA 3
Duration of symptoms
Less than 6 weeks 0
More than 6 weeks 1
Acute phase reactant
Normal CRP and ESR 0
Abnormal CRP or ESR 1
• Patients with 6 or more are
considered to have RA.

Management
:
goal is disease control and induction of disease
remission
• Patient education
• Multidisciplinary team
• Physical rest and passive exercises.
• Re assessment

Drug Therapy:
• Prompt and early introduction of small molecules
DMARDs and corticosteroid play a central role in
induction of remission.
• The patient should be informed that DMARDs will not
improve symptoms immediately. But in longer term the
symptoms will be under control and joint damaged will
be prevented. If no or partial response to DMARD
therapy this necessities increase the dose or combine
with other DMARD, with progression to biological drugs if
needed.

SOME OF DMARDS ARE CONTRAINDICATED IN PREGNANCY.
REGULAR MONITORING IS NECESSARY TO EXCLUDE SIDE
EFFECT AND TOXICITY (MAINLY HEMATOLOGICAL AND LIVER
TOXICITY) AND TO EVALUATE DRUG EFFICACY.
.
IT NOT REVERSE THE ALREADY PRESENT EROSIONS BUT CAN
STOP OR MODIFY THE DISEASE PROGRESSION .
*THE MOST COMMON DMARD OF CHOICE IS
METHOTREXATE ( MTX).

Disease Modifying Anti-Rheumatic Drugs(DMARDs):
Methotrexate(MTX):
It is considered the main drug of choice or the anchor of
DMARD therapy .
The starting dose is 10-15 mg /week increasing by 2.5 mg
every 2- 4 week until benefit or toxicity. The maximum
dose is 25mg/week.
It can used alone or with other DMARD (combination)
therapy.
benefit appear after 1- 4 months after initiation of drug.

• MAIN EARLY SIDE EFFECT ARE NAUSEA , VOMITING ,
MALAISE IF PERSIST PATIENTS CAN EFFECTIVELY TREATED
BY SUBCUTANEOUS ROUT.
PATIENTS SHOULD ALARM ABOUT DRUG INTERACTION
WITH SULPHONOMIDES.
ALSO PATIENT SHOULD AVOID ALCOHOL WHICH MAY
ENHANCE HEPATOTOXICITY.
REGULAR MONITORING IS ESSENTIAL FOR EARLY
DETECTION OF SERIOUS SIDE EFFECT (HEPATIC OR BONE
MARROW TOXICITY) .
PULMONARY PNEUMONITIS IS RARE SERIOUS SIDE
EFFECT, IF OCCUR THE DRUG SHOULD STOPPED
IMMEDIATELY AND PATIENT TREATED WITH HIGH DOSE
OF STEROID.

Sulfasalazine:
CAN Taken orally alone, but usually with MTX.
GIT upset and nausea main side effect.
Starting dose 500mg/day and increasing gradually to 2-4
gm /day
Monitoring for hematological and hepatic toxicity

Hydroxychlorquine:
Ususlly used with comnination with other
DMARD(mainly MTX.sulfasalazine.)
Given in dose of 400mg/d.
Retinal damage may occur in long term
treatment.
Visual acuity should tested before treatment and
repeated regularly as treatment is going on.

Leflunomide:
Can be used alone or with other drug.
Given in dose of 10- 20 mg/day.
Usually well tolerated, low marrow toxicity, but
may cause liver dysfunction.
Require regular liver and hematological
monitoring.

Gold, pencillamine, ciclosporine:
these drugs are occasionally used for RA treatment due
to availability of other drugs with a better risk- benefit
profile.

Corticosteroid : although it has disease modifying effect, but its
main use are:
Induction
of remission in patients with RA who starting synthetic
DMARD. And tapering till the effect of DMARD appear(
bridge
therapy).
In flare up
of disease while patient already on DMARD therapy.
Flare up during pregnancy
Intraarticular injection of
corticosteroid when one or two joints
with persistent synovitis in spite of generalized well
being and
other joints are remitted ( in this situation possibility of infection
should be excluded)
Corticosteroid therapy carry many side effects mainly
osteoporosis, which is also main complication of RA even in
absence of steroid therapy.
DEXA should considered in RA with anti osteoporotic measures
especially for those on steroid of 7.5 mg/day for more than 3
months.

Biological therapies
are reserved for the treatment of patients who
have high disease activity despite having had an adequate
trial of traditional DMARDs.
More effective and cost more greater than synthetic DMARDs.
In UK its used restricted to patient with active RA (DAS28 > 5.1;
when an adequate trial of at least two other
DMARDs (including methotrexate) has dts
.

1-ANTI-TNF THERAPY:
ETANRECEPT
INFLIXIMAB
ADALIMUMAB
GOLIMUMAB
CERTOLIZUMAB
CAN BE USED AS MONOTHERAPY (ALTHOUGH A
COMBINATION WITH MTX GIVE BETTER RESULTS) .
MTX REDUCED NEUTRALIZING EFFECT OF ANTIBODIES
FORMATION AGAINST ANTI-TNF THERAPY

The main side effects of anti TNF alpha therapy are
increase risk of infection mainly reactivation of
latent T.B and increase risk of malignancy mainly
basal cell carcinoma of skin and increase
progression of cancer in patients with prior tumor.

2- Anti B cell therapy: Rituximab
3- Inhibitor of T- cell activation: (Abatacept).
4- ANTI IL-6( Tocillizumab).
5- Anti IL-1(Anakinra).
now
JAK
(janus kinase inhibitor): tofacitinib and
baricitinib.
• New diagnosis of rheumatoid arthritis
• s
Increase dose over 12 week MTX
• +
• Prednisolone Decrease dose
over 12 weeks
• DAS 28 <2.6 DAS 28 >2.6
•
• Continue MTX Add SSZ + HCQ
•
• DAS 28<2.6 DAS 28 2.6-5.1
DAS 28>5.1
•
• Continue triple therapy Change DMARD or
add low-dose prednisolone Add biologic

Surgery:
in complicated conditions surgical interventions may
required as: synovectomy, tendon repair, arthrodeses,
arthroplasty
.

General measures:
Patient education about nature of disease, regular
monitoring and periodic disease assessment.
Physical rest, NSAIDs and analgesia.
Joint protection , splinting, regular active and gentle
passive exercise to preserve joint function prevent
muscle atrophy and joint contracture.
Hospitalization needed in multiple joint injection ,
splinting, joint injections.

*Prognosis:
the following factors at presentation are associated with
poor prognosis:
1- higher base line disability.
2- insidious onset.
3- female gender.
4- positive Rheumatoid factor , anti-ccp(ACPA) and nodule
formation, smoking
5- positive family history of severe RA.
6- involvement of MTP.
7- disease duration of over three months.
8- presence of extra-articular manifestations.

RA during pregnancy: most patients with
RA go into remission during pregnancy.
methotrexate should be discontinued for at least 3 months
and leflunomide discontinued for at least 24 months
before trying to conceive.
Paracetamol: the oral analgesic of choice during
pregnancy.
Oral NSAIDs and selective COX-2 inhibitors: can be used
after implantation to 20 weeks’ gestation.
Corticosteroids: may be used to control disease flares; the
following
maternal risks as hypertension, glucose intolerance
and osteoporosis should be considered.

DMARDs that may be used: sulfasalazine,
hydroxychloroquine, azathioprine if required to control
inflammation.
DMARDs that must be avoided: methotrexate,
leflunomide, cyclophosphamide, mycophenolate ,gold .
Biological therapies: safety during pregnancy is currently
unclear. Theoretical risk is immunosuppression of neonate.
Breastfeedin
g:
methotrexate, leflunomide,
cyclophosphamide, are contraindicated.
