
SEIZURES AND EPILEPSY
INTRODUCTION
• Seizure is any clinical event caused by an abnormal electrical discharge in
the brain, whilst epilepsy is the occurrence of more than one unprovoked
seizure more than 24 hours apart.
• Convulsion is a seizure with intense motor component.
• The lifetime risk of having a single seizure is about 5%.
• Epilepsy should be regarded as a symptom of brain disease rather than a
disease itself.
Pathophysiology
• It is likely that both reduction in inhibitory systems and excessive excitation in
the brain play a part in the genesis of seizure activity.
• The inhibitory transmitter gamma-aminobutyric acid (GABA) is particularly
important in this role, and drugs that block GABA receptors provoke seizures.
• Conversely, excessive stimulation by excitatory neurotransmitters e.g.
acetylcholine, glutamate, provoke seizure activity.
• Cells undergoing repetitive 'epileptic' discharges undergo morphological and
physiological changes which make them more likely to produce subsequent
abnormal discharges ('kindling').
Clinical classification of seizures
.
1. Partial seizures
a. Simple partial seizures (with motor, sensory, autonomic, or psychic signs)
b. Complex partial seizures
c. Partial seizures with secondary generalization
2. Primarily generalized seizures
a. Absence (petit mal)
b. Tonic-clonic (grand mal)
c. Tonic
d. Atonic
e. Myoclonic
3. Unclassified seizures
a. Neonatal seizures
b. Infantile spasms
Clinical features
I -GENERALISED
Tonic clonic seizures (grand mal epilepsy)
1- A tonic clonic seizure may be preceded by a partial seizure (the 'aura').
2-Tonic phase: The patient goes rigid and becomes unconscious, falling down
heavily if standing and often sustaining injury.
Respiration is arrested and central
cyanosis may be witnessed. Contraction of the jaw muscles may cause biting of the
tongue.
3- Clonic phase:
rigidity is periodically relaxed, producing clonic jerks
4- Postictal phase:
is characterized by unresponsiveness, muscular flaccidity, and
excessive salivation. Bladder or bowel incontinence may occur at this point.
Patients gradually regain consciousness over minutes to hours, and during this
transition there is typically a period of postictal confusion. Patients subsequently
complain of headache, vomiting, fatigue, and muscle ache that can last for many
hours.
Full memory function may not be recovered for some hours.
Absence seizures
• Absence seizures (petit mal) always start in childhood. The child stares fixedly
with eyes turned upward, blinks, and may make movements of the tongue or
mouth, or pick at his or her clothes.
• The attacks can be mistaken for complex partial seizures but are shorter in
duration they occur much more frequently (20-30/ day) and are not associated
with post-ictal confusion.
• The examining physician may be able to provoke an absence by having the
patient hyperventilate.
• Typical absence seizure may show the typical 3 HZ cycle in the EEG.
II-PARTIAL
Partial seizures are always due to a circumscribed lesion in the brain.
Partial
seizures may occur with the patient remaining fully conscious (simple partial
seizures).
They can, however, involve an impairment of consciousness, in which
case they are called complex partial seizures.
Partial motor seizures
• Seizures are characterised by rhythmical jerking or sustained spasm of the
affected parts.
• Some attacks begin in one part (e.g. mouth, thumb, great toe etc.) and spread
gradually; this is 'Jacksonian march’.
• More prolonged episodes may leave paresis of the involved limb lasting for
several hours after the seizure ceases (Todd's palsy).
Partial sensory seizures
• Seizures arising in the sensory cortex cause unpleasant tingling or 'electric'
sensations in the contralateral face and limbs.
• A spreading pattern like a Jacksonian seizure may occur, the abnormal
sensation spreading much faster over the body (in seconds) than the 'march'
of a migrainous focal sensory attack, which spreads over 10-15 minutes.
Complex partial seizures
• Partial seizures may cause episodes of altered consciousness without the
patient collapsing to the ground.
• The patient stops what he or she is doing and stares blankly.
• This behavioral arrest is usually accompanied by automatisms, which are
involuntary, automatic behaviors that have a wide range of manifestations.
• Automatisms may consist of very basic behaviors such as chewing, lip
smacking, swallowing, or "picking at their clothes." movements of the hands.
• The patient is typically confused following the seizure, and the transition to full
recovery of consciousness may range from seconds up to an hour.
• Immediately before such an attack the patient may report alterations of mood,
memory and perception such as undue familiarity (déjà vu) or unreality
(jamais vu), complex hallucinations of sound, smell, taste, vision, emotional
changes (fear, sexual arousal) or visceral sensations (nausea, epigastric
discomfort).
Partial seizures with secondary generalization
• Generalised epilepsy may arise from spread of partial seizures.
• Epilepsy presenting in adult life is almost always secondary generalised, even
if there is no clear history of a partial seizure before the onset of a major
attack.
Approach to patient with seizure
• When a patient presents shortly after a seizure, the first priorities are attention
to vital signs, respiratory and cardiovascular support, and treatment of
seizures if they resume
• Goals are
1. Is it seizure or not?
2. What is the cause or precipitating factors?
3. Whether anticonvulsant therapy is required?
History & examination
• In many cases the diagnosis of a seizure is based solely on clinical history —
the examination and laboratory studies are often normal.
• Differential diagnosis of seizure are:
1. Syncope
2. Migraine
3. Transient ischemic attacks
4. Hypoglycaemia

5. Psychogenic seizure (pseudoseizure)
• Features make the diagnosis of seizure more likely:
1. Aura
2. Stereotyped attacks
3. Cyanosis
4. Biting "lateral border" of the tongue
5. Post-ictal confusion
6. Post-ictal amnesia
7. Post-ictal headache
8. Developed during sleep
9. Loss of continence
10. Causing injury
• The general physical examination includes a search for signs of infection or
systemic illness (liver or renal disease), signs of head trauma and use of
alcohol or illicit drugs.
Investigations:
1. Routine blood studies are indicated to identify the more common
metabolic causes of seizures.
2. EEG:
• In the evaluation of a patient with suspected epilepsy, the presence of
electrographic seizure activity during the clinically evident event clearly
establishes the diagnosis.
• The absence of electrographic seizure activity does not exclude a seizure
disorder.
• Inter-ictal records are abnormal in only about 50% of patients so the EEG is
not a sensitive test for the presence or absence of epilepsy.
• Specific epileptiform changes include sharp waves or spikes.
3-Brain imaging:
• Imaging can never establish a diagnosis of epilepsy but is useful in defining or
excluding a structural cause.
Management
Immediate management of seizures
1. Move person away from danger (fire, water, machinery, furniture)
2. After convulsions cease, turn into 'recovery' position (semi-prone)
3. Ensure airway is patent
4. Give oxygen
5. Secure an intravenous access and Draw blood for glucose,urea, electrolytes
and drug or toxin.
6. Give intravenous anticonvulsant (e.g. diazepam 10 mg) ONLY IF convulsions
are continuous or repeated
7. Do NOT insert anything in mouth
8. Person may be drowsy and confused for some 30-60 minutes and should not
be left alone until fully recovered
9. Investigate cause
• Patients should be made aware of the riskiness of any activity where loss of
awareness would be dangerous (driving, swimming, boating) until good
control of seizures has been established.
Anticonvulsant drug therapy
• Drug treatment should certainly be considered after more than one seizure
has occurred.
• The mode of action is either to increase inhibitory neurotransmission in the
brain or to alter neuronal sodium channels in such a way as to prevent
abnormally rapid transmission of impulses.
• Phenytoin and carbamazepine are not ideal agents for a young woman
wishing to use oral contraception, because the drugs induce liver enzymes.
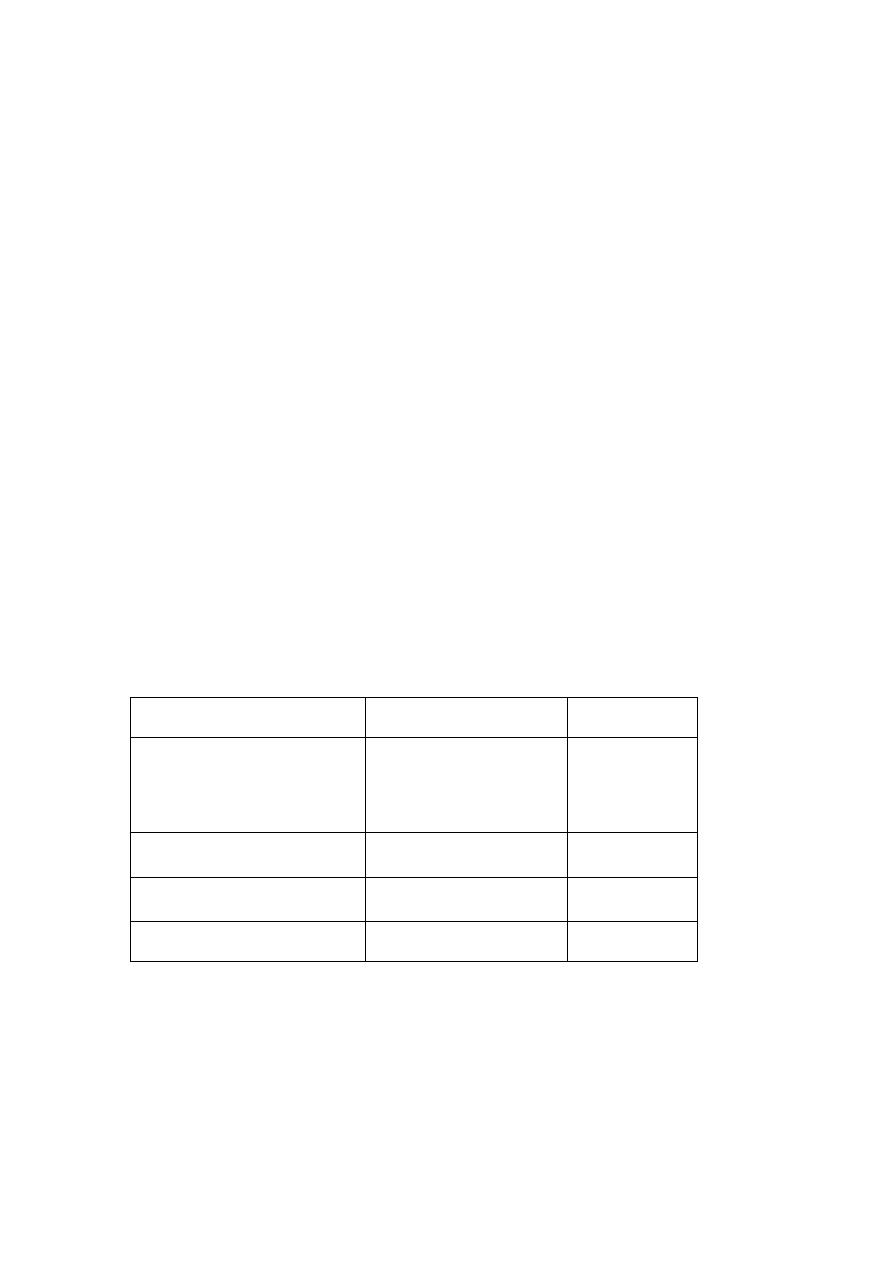
• Guidelines for choice of antiepileptic drugs
Epilepsy type
1
st
line
2
nd
line
Partial and/or secondary GTCS
Lamotrigine
Carbamazepine
levetiracetam
valproate
Topiramate
Primary GTCS
Valproate
Levetiracetam
Lamotrigine
Topiramate
Absence
Ethosuximide or
valproate
Lamotrigine
Myoclonic
valproate
Clonazepam
• The choice of antiepileptic drug depends on seizure type, patient age, side
effect profile of the drug, comorbid illness, drug cost.
• After complete control of seizures for 5 years, withdrawal of medication may
be considered.
• Withdrawal should be undertaken slowly, reducing the drug dose gradually
over 6-12 months.

• Overall, the recurrence rate of seizures after drug withdrawal is about 40%.
