
Systemic Sclerosis

Systemic Sclerosis (definition)
• Multisystem disorder
• Unknown etiology
• Thickening of skin caused by accumulation of
connective tissue (collagen types I and III)
• Involvement of visceral organs

Epidemiology
• Peak age range: 35-64
• Younger age in women and with diffuse
disease.
• Female:Male = 3:1
• 8:1 in child bearing years
• Incidence: 20/million per year in US
• Prevalence: 240/million in US.

Etiology
• Unknown
• Environmental Exposures
• Silica exposure in men conferred increased risk
• Silicone breast implants: no definite risk
identified
• Aniline laced Contaminated rapseed oil in
Spain
• Vinyl chloride exposure increased risk of SSc
like disorder: Eosinophilic Fasciitis
• bleomycin
• L-tryptophan: Eosinophilia Myalgia syndrome

Etiology
• Genetic Factors
• Familial Clustering: 1.5-2.5% of those with 1
st
degree relative
–Choctow Native Americans: prevalence
4720/million.
• HLA-haplotypes: there are higher risk
haplotypes in certain populations

Pathogenesis: general principles
• Endogenous or exogenous pathogen stimulates antigen
presenting cells.
• Antigen presenting cells stimulate CD4+ T cells
• Cytokines are produced by both of these cells.
• Cytokines stimulate growth factors to stimulate fibroblasts
to produce collagen
• Vascular damage occurs with thickened intima and
narrowing of the lumen.
• Narrowing of the lumen leads to ischemia.
• Ischemia leads to prostacyclin production which is a
platelet aggregant and platelets bind to endothelium and
release PDGF which is chemotactic and mitogenic for
fibroblasts.
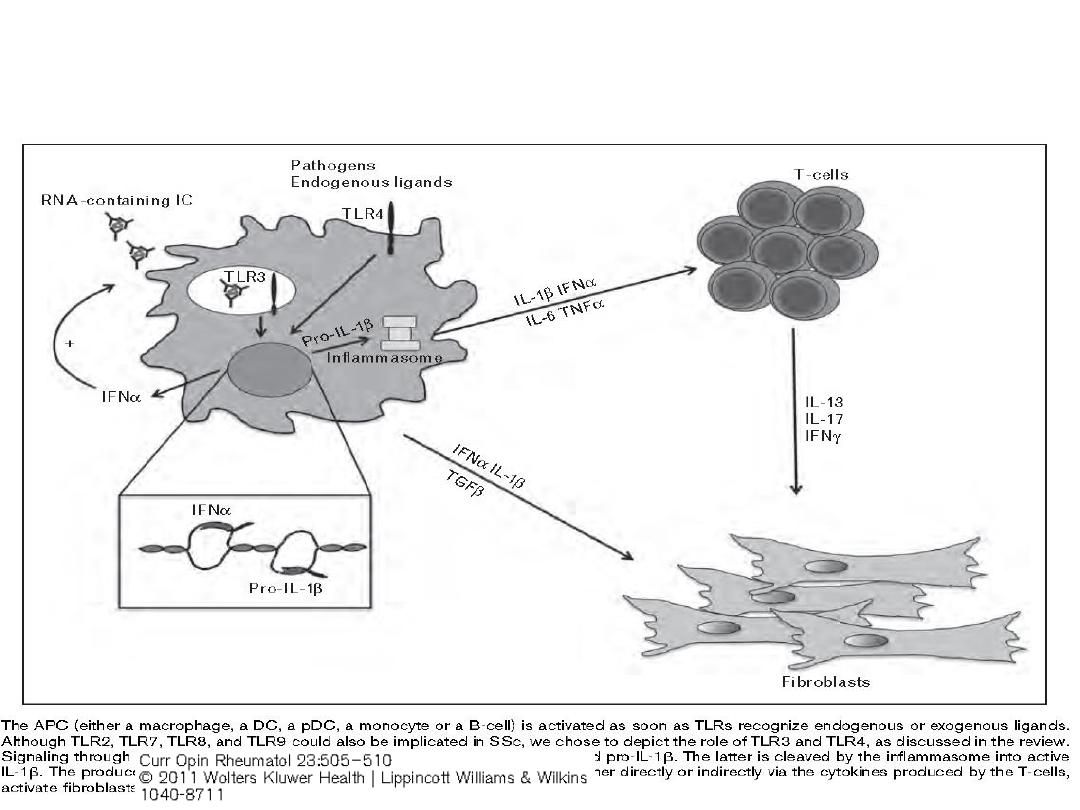
Pathogenesis
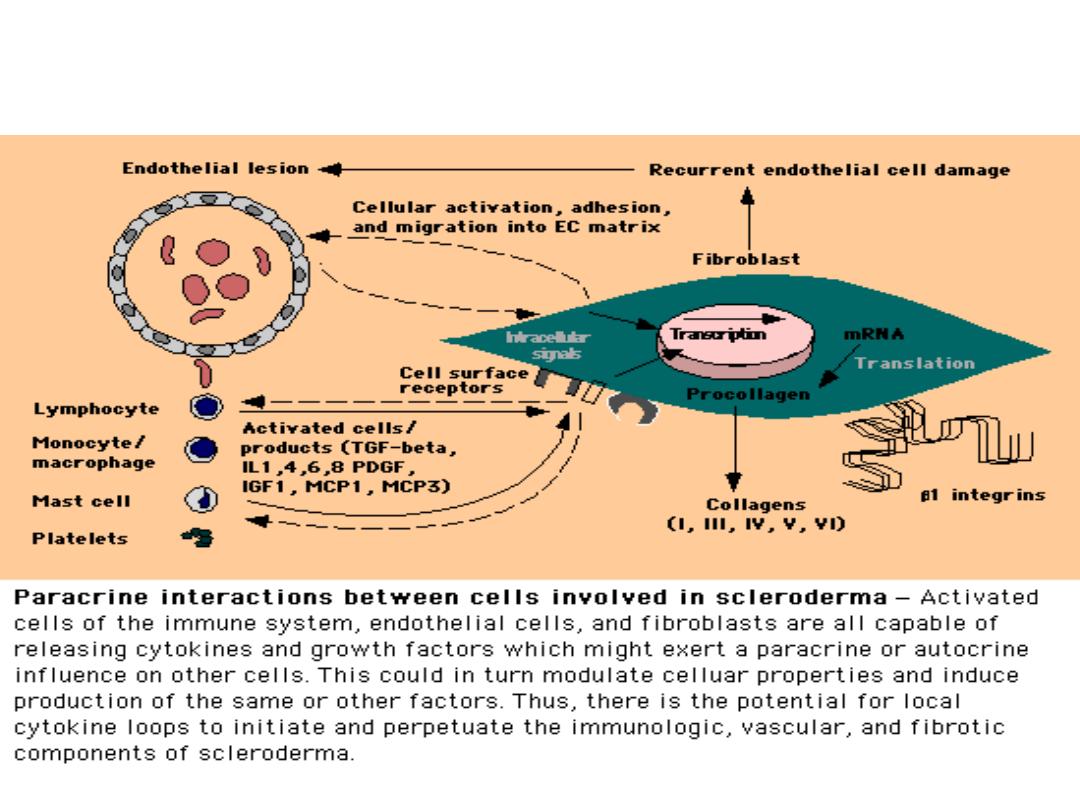
Pathogenesis of Scleroderma
Up to Date

Forms of Systemic Sclerosis
• Limited Scleroderma
• Skin thickening is distal to elbows and knees, not
involving trunk
• Can involve perioral skin thickening (pursing of lips)
• Less organ involvement
• Seen in CREST syndrome
• Isolated pulmonary hypertension can occur
• Diffuse Scleroderma
• Skin thickening proximal to elbows and knees,
involving the trunk
• More likely to have organ involvement
• Pulmonary fibrosis and Renal Crisis are more
common.
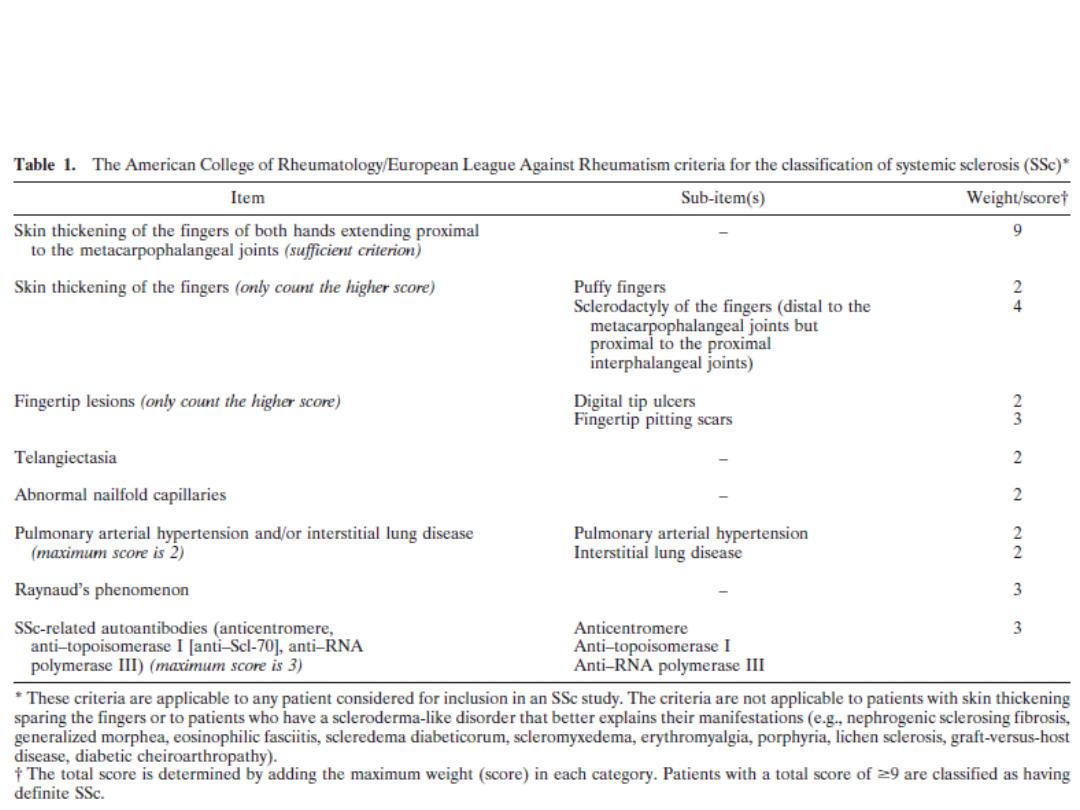
2013 ACR Diagnostic Criteria

Limited Scleroderma
• More gradual process
• Can have Raynaud’s for years (even up to decade)
• Skin involvement distal to elbows and knees
• Often with perioral involvement (pursing of lips)
• Capillaroscopy
• with dilated capillary loops but without dropout.
• Less organ involvement
• though 10-15% with isolated pulmonary
hypertension.
• Renal involvement is rare.
• Anti-centromere Ab in 70-80%
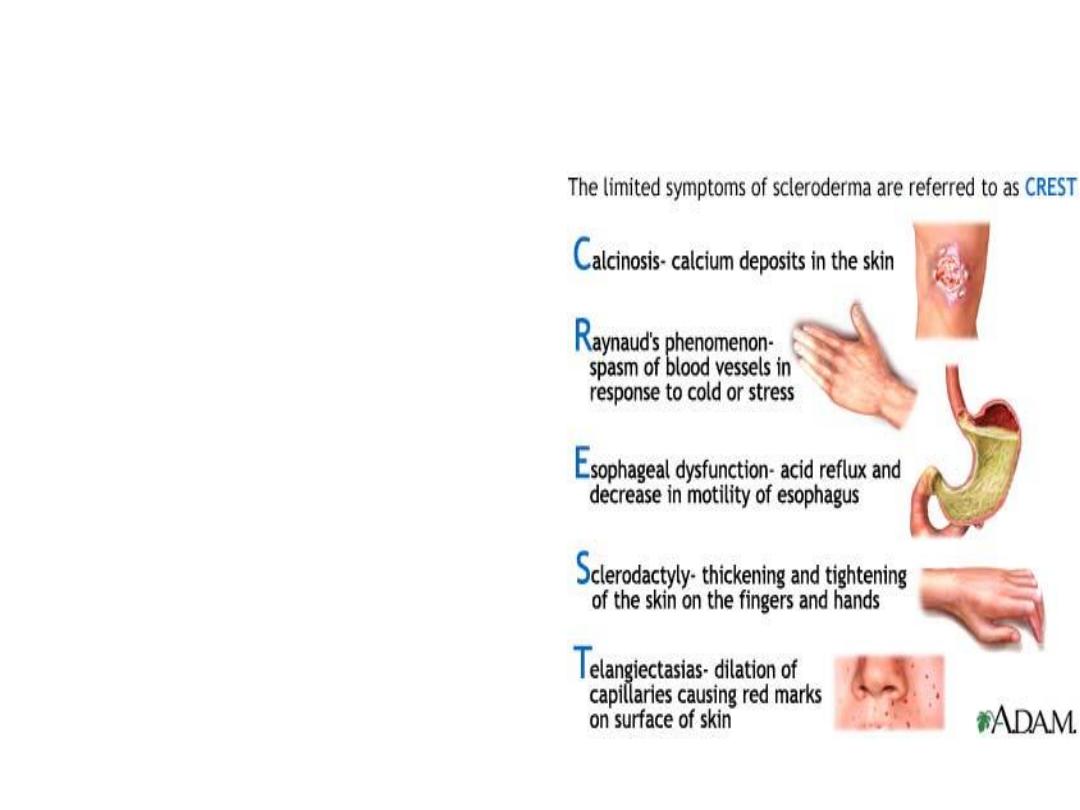
Limited Scleroderma
• CREST Syndrome
• Calcinosis
• Raynaud’s
• Esophageal
Dysmotility
• Sclerodactyly
• Telangiectasisa
A.D.A.M. Images

CREST Syndrome
ACR and Mayo Foundation

Calcinosis on x-ray
Gupta E., et al.
Malaysian Family
Physician. 2008;3(3):xx-xx
ACR
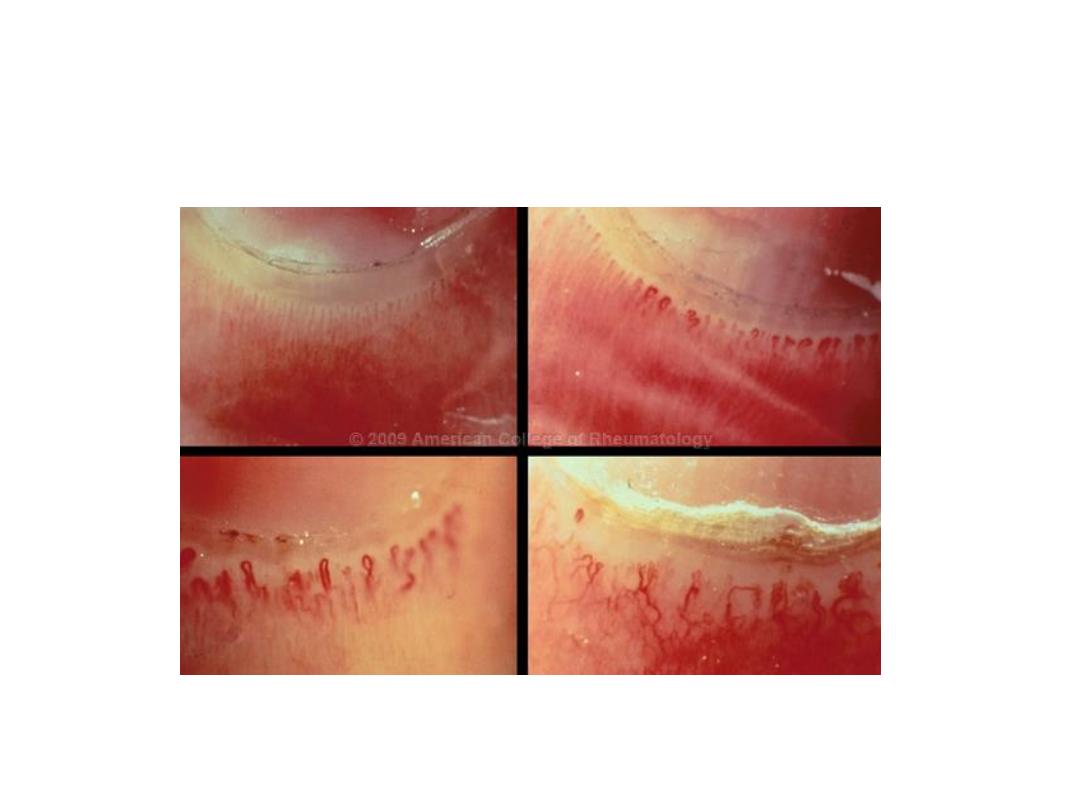
Nailfold Capillaroscopy

Diffuse Scleroderma
• More Rapid Process
• Often with onset of skin thickening within a year of
Raynaud’s symptoms
• Skin involvement proximal to elbows and knees
• Often can involve the trunk
• Capillaroscopy reveals dropout
• With capillary dilatation and dropout.
• Early organ involvement
• Renal, interstitial lung disease, myocardial, diffuse
gastrointestinal – often within the first 3 years.
• Antibodies
• Anti-Scl-70, anti-RNA Polymerase III.
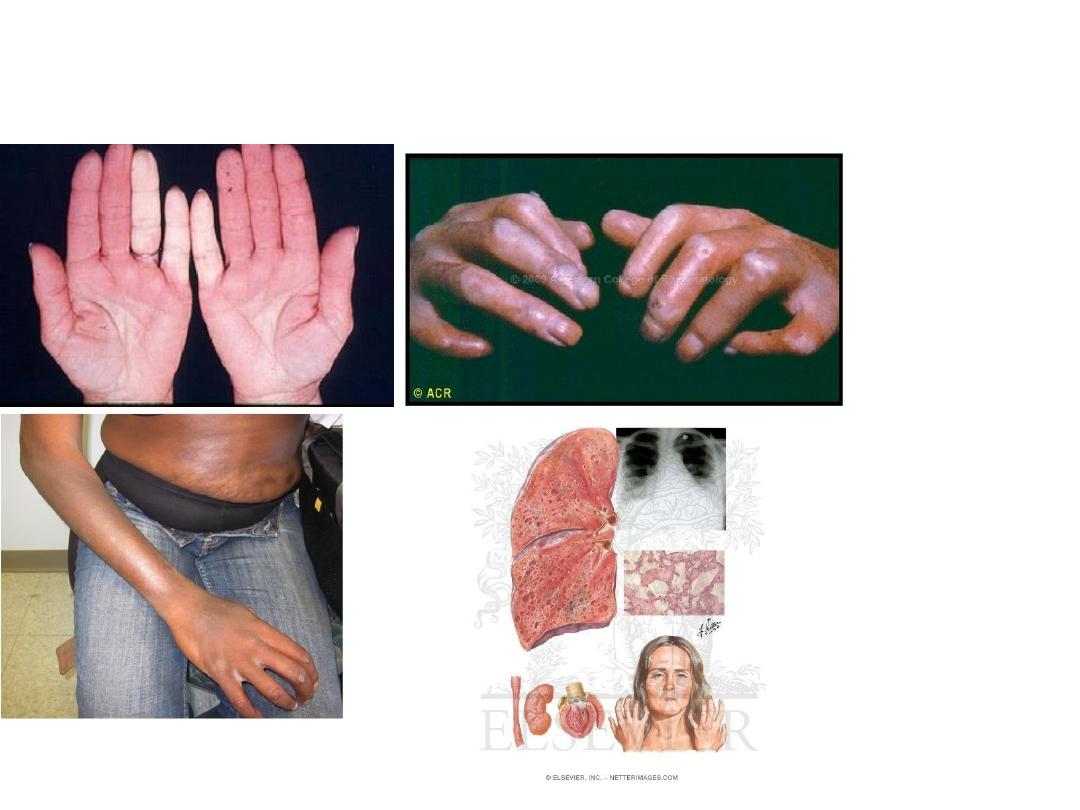
Diffuse Scleroderma
ACR
American Osteopathic College of Dermatology, Grand
Rounds
Netter

Organs Involved
• Skin
• Musculoskeletal
• Pulmonary
• Renal
• Gastrointestinal
• Cardiac

Skin Involvement
• Early stages:
• Perivascular infiltrate which are primarily T cells.
• Skin swelling which eventually becomes skin thickening.
• Involves the hands and/or feet (distal).
• Late Stages:
• Finger-like projections of collagen extend from the dermis to
the subcutaneous tissue to anchor skin deeper.
• Skin becomes firm, thick and tight.
• Skin thickening moves proximally.
• Fibroblasts and collagen deposition.
• Hair and wrinkles overlying area of skin thickening disappears.
Skin involvement in Scleroderma
• May regress on its own over years
• reverse pattern (ie, starting with regression of
skin thickening in the trunk, then proximal
extremities, then more distal).
• Digital Ulcers:
• on extensor surface of PIP’s and elbows; may
become secondarily infected.
• Digital ischemia:
• with pits in the distal aspect of the digits
related to prolonged Raynaud’s.
• Thinning of the lips, beak-like nose.

Skin Manifestations
Kahaleh B. Rheum Dis Clin N Amer 2008:57-71
Sclero.org
International
Scleroderma Network
ACR

Musculoskeletal
• Arthritis
• in > 50% with swelling, stiffness, and pain in
the joints of the hands.
• Carpal Tunnel Syndrome.
• Contractures
• related to skin thickening.
• Polymyositis
• may occur as part of mixed connective tissue
disease or overlap.

Pulmonary
• leading cause of death
• since we are better at control of renal disease.
• Symptoms:
• exertional dyspnea
• Types of lung Involvement:
• Interstitial lung disease.
• Isolated pulmonary hypertension.
Interstitial Lung Disease
• Inflammatory phase
• with ground glass opacities and linear infiltrates
• lower 2/3 of the lung fields on CT scan.
• Fibrosis:
• Late phase with honeycombing.
• Diagnosis
– Pulmonary function tests
• restrictive pattern with low FVC, low residual volume, low
DLCO.
– High Resolution CT Scan
– BAL: often not required
– Lung biopsy: often not required
• ILD is most commonly associated with diffuse scleroderma.
• Anti-Scl-70

Interstitial Lung Disease
Up to Date 2005
Up to Date 2005

Primary Pulmonary Hypertension
• Symptoms:
• exertional dyspnea.
• Frequency
• 10-15% of patients with systemic sclerosis
• Definition:
• Mean PA blood pressure >25mmHg at rest or
>30mmHg with exercise on right heart
catheterization.
• Estimated systolic pulmonary artery pressure of
>35mmHg on Echocardiogram
• Pathogenesis
• Intimal fibrosis and medial hypertrophy of the
pulmonary arterioles and arteries.
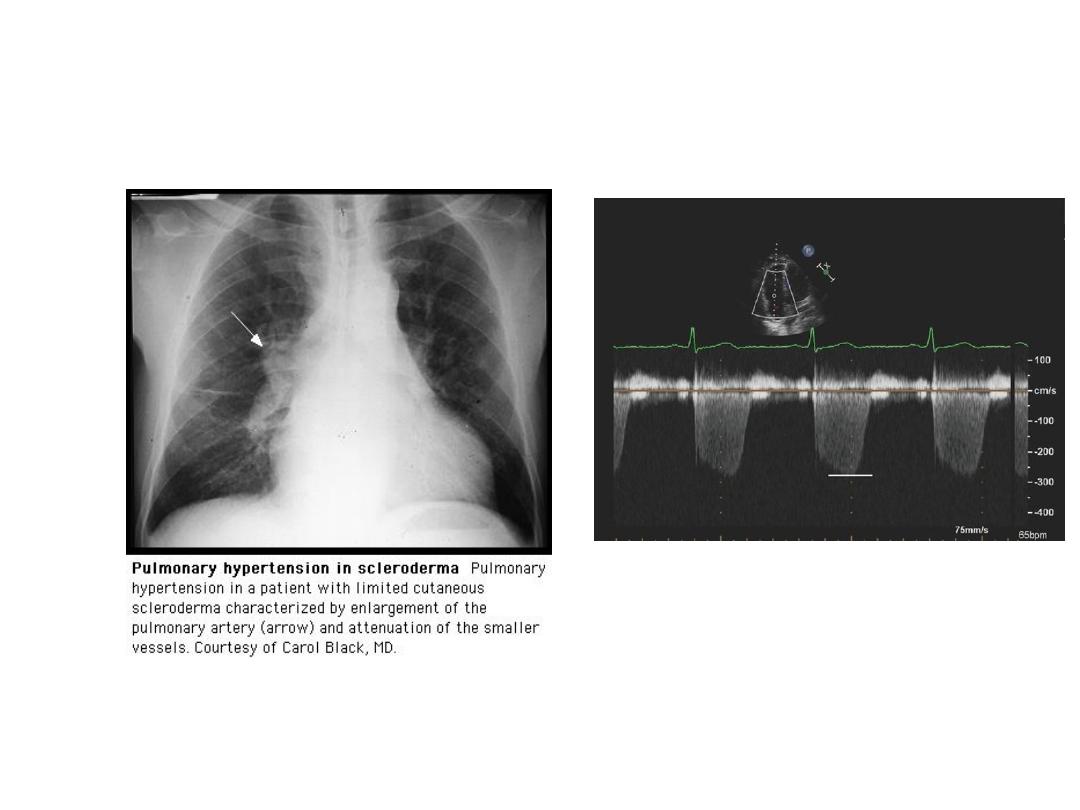
Pulmonary Hypertension
Up to Date 2005
Doppler Echocardiogram to estimate
pulmonary artery pressure.
Roberts JD. Pulm Circ 2011;1:160-181.

Other Pulmonary Associations
• Pneumonia:
• due to aspiration secondary to GERD; skin thickening
of chest may reduce effectiveness of cough.
• Alveolar carcinoma: increased incidence
• Bronchogenic carcinoma: increased incidence.
Renal Manifestations of Systemic Sclerosis
• Scleroderma Renal Crisis
• Abruptly developing severe hypertension
– Rise in SBP by > 30 mmHg, DBP by > 20 mm Hg
• One of the following:
– Increase in serum creatinine by 50% over baseline or creatinine > 120%
of upper limit.
– Proteinuria > 2+ by dipstick.
– Hematuria > 2+ by dipstick or > 10 RBC/HPF
– Thrombocytopenia < 100
– Hemolysis (schisctocytes, low platelets, increased reticulocyte count).
• Can cause headache, encephalopathy, seizures, LV failure.
• 90% with blood pressure > 150/90.
• Can occur also with lower blood pressures < 140/90 and this
confers worse prognosis.
Steen et al., ClinExp. Rheumatol. 2003
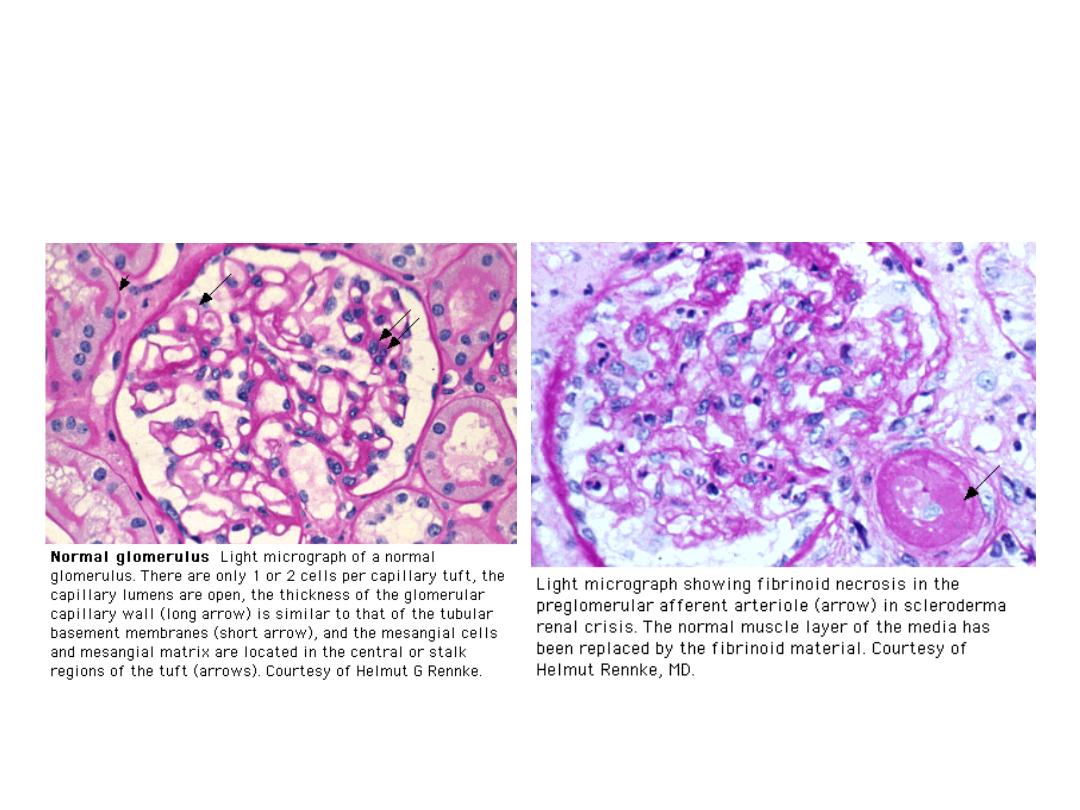
Scleroderma Renal Crisis
Up to Date 2012

Risk Factors for Renal Crisis
• Rapidly progressive skin thickening within the first
2-3 years.
• Steroid use (prednisone > 15 mg)
• Anti-polymerase III Ab.
• Pericardial Effusion.

Treatment of Scleroderma Renal Crisis
• Medical Emergency: generally with admission.
• Initiation of ACE inhibitors such as captopril;
lifelong treatment with ACE inhibitors.
• Dose escalation of captopril.
• ACE-inhibitors do not prevent SRC.
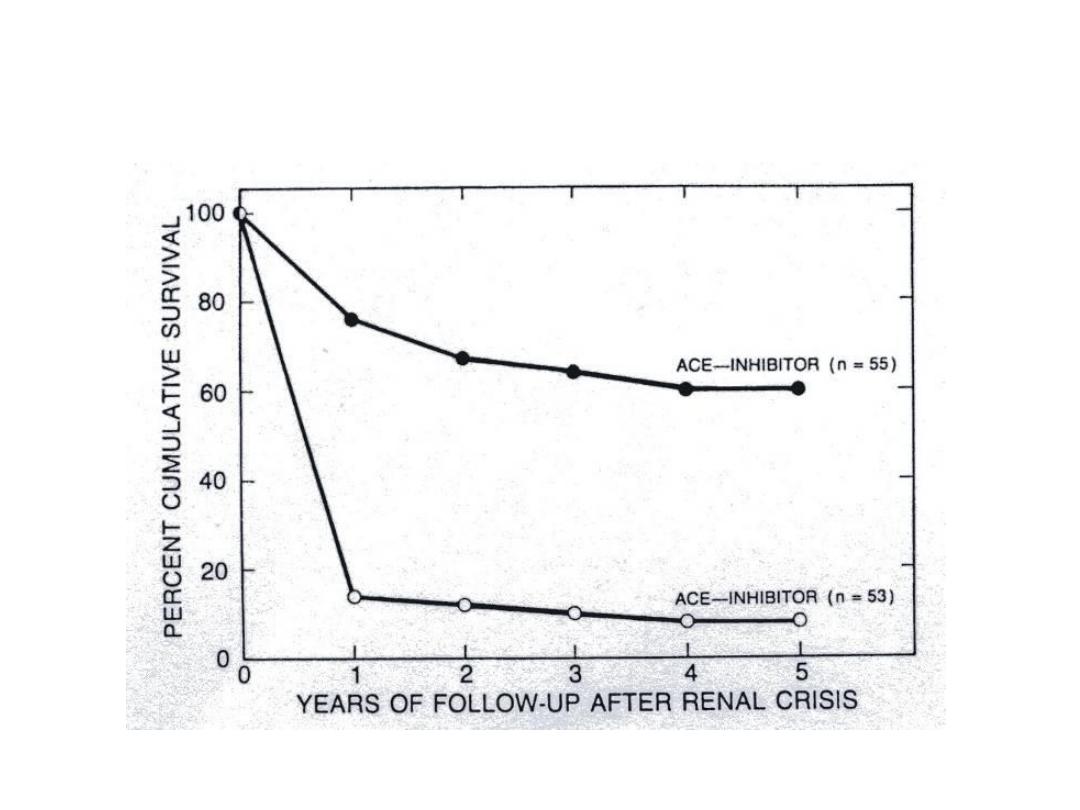
Treatment of Scleroderma Renal Crisis
Steen, Clinics in Dermatology, 1994
Without

Renal Crisis - Prognosis
• Improved overall with ACE-inhibitors.
• Even with ACE-inhibitors 20-50% will progress to
ESRD.
• Among patients who required dialysis during the
acute phase, an appreciable proportion (40-50%)
will be able to discontinue dialysis.

Gastrointestinal Manifestations
• Esophageal dysmotility: in up to 90%.
• Pathophysiology:
– reduced tone of gastroesophageal sphincter and distal dilatation of the
esophagus.
– Lamina propia and submucosal tissue with Inflammatory changes and
increased collagen on pathology.
• Symptoms
– Dysphagia, GERD; many asymptomatic.
• Diagnosis:
– Esophageal manometry, Esophagram, CT scan.
• Treatment
– Proton Pump Inhibitors
– Elevation of head of the bed.
• Complications:
– Barret’s Esophagus.

Gastrointestinal Manifestations
• Gastric Involvement:
• Symptoms: Early satiety.
• Diagnosis: Nuclear Gastric Emptying Test.
• Treatment: promotility agents
• Watermelon Stomach: dilated vessel which can cause bleeding.
• Small Intestinal involvement
• Symptoms: distension, pain, bloating, steatorrhea
• nutritional deficiencies secondary to bacterial overgrowth.
» Vitamin B6/B12/folate/25-OH Vit D, low albumin
• Diagnosis:
– glucose hydrogen breath test
– Low D-xylose absorption test
– small bowel aspiration (only if resistance to rotating antibiotics)
• Treatment: Rotating antibiotics, Reglan, Erythromycin
Image of Watermelon Stomach: University of Michigan Rheumatology Website
Gastrointestinal Manifestations
• Colon Involvement:
• Can cause symptoms of constipation due to
decreased peristalsis.
• Fecal incontinence can occur due to alterations
of internal and external sphincter.

Cardiac Manifestations
• Forms of cardiac involvement
• Pericardial Effusion
– symptomatic pericarditis in 20%
• Microvascular CAD:
– recurrent vasospasm of coronary arteries
– Necrosis
– patchy myocardial fibrosis; leads to diastolic > systolic
dysfunction.
• Myocarditis
– Inflammation which leads to fibrosis
• Arrhythmias and conduction abnormalities
– Fibrosis of cardiac conduction system.
– AV conduction defects and arrhythmias.
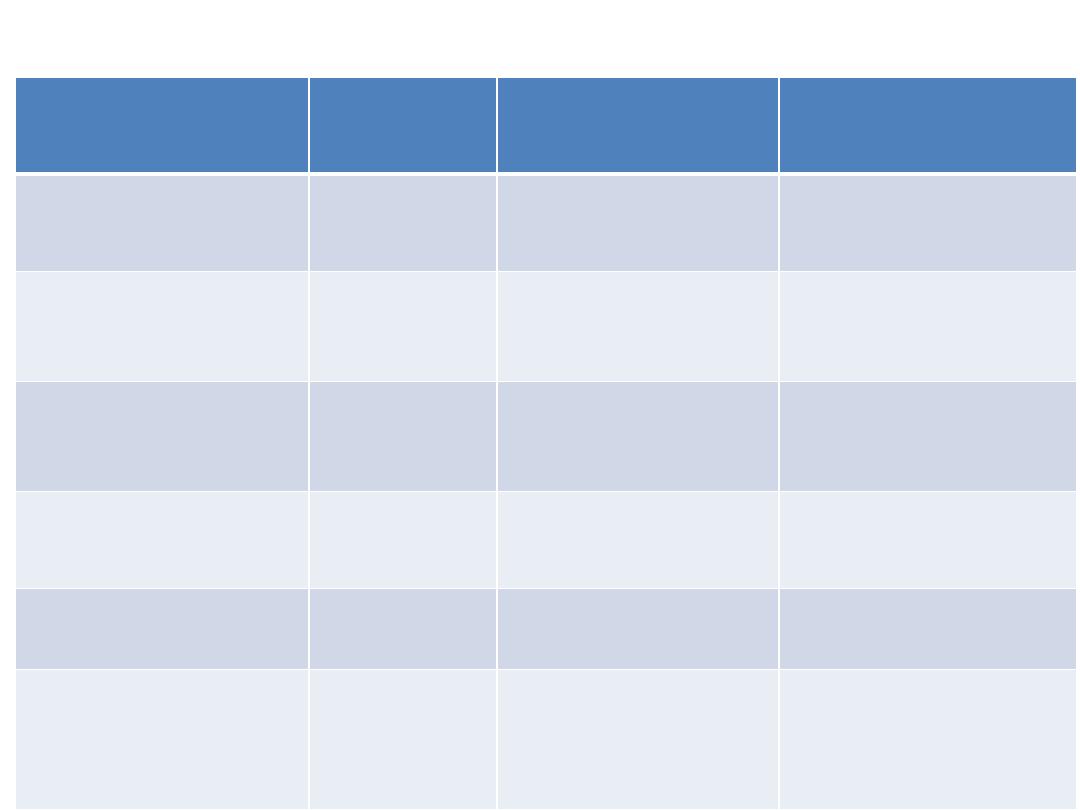
Cardiac Involvement
Adapted from Desai, et al; Curr Opin Rheumatol 2011m 23:545-554
Cardiac
Manifestation
Prevalence Diagnosis
Treatment
Myocarditis
Rare
Cardiac MRI,
Biopsy
Cytoxan + steroids
Pericardial
effusion
5-16%
Echocardiogram
None; NSAIDs if
symptomatic
Microvascular
CAD
> 60%
MRI/nuclear
medicine
Calcium channel
blockers
Macrovascular
CAD
25%
Coronary
Angiogram
Stenting/medical
tx
Bradyarrhythmias Rare
EKG/Holter
Pacemaker
Tachyarrhythmias 15%
EKG/Holter
Diltiazem,
ablation,
defibrillator
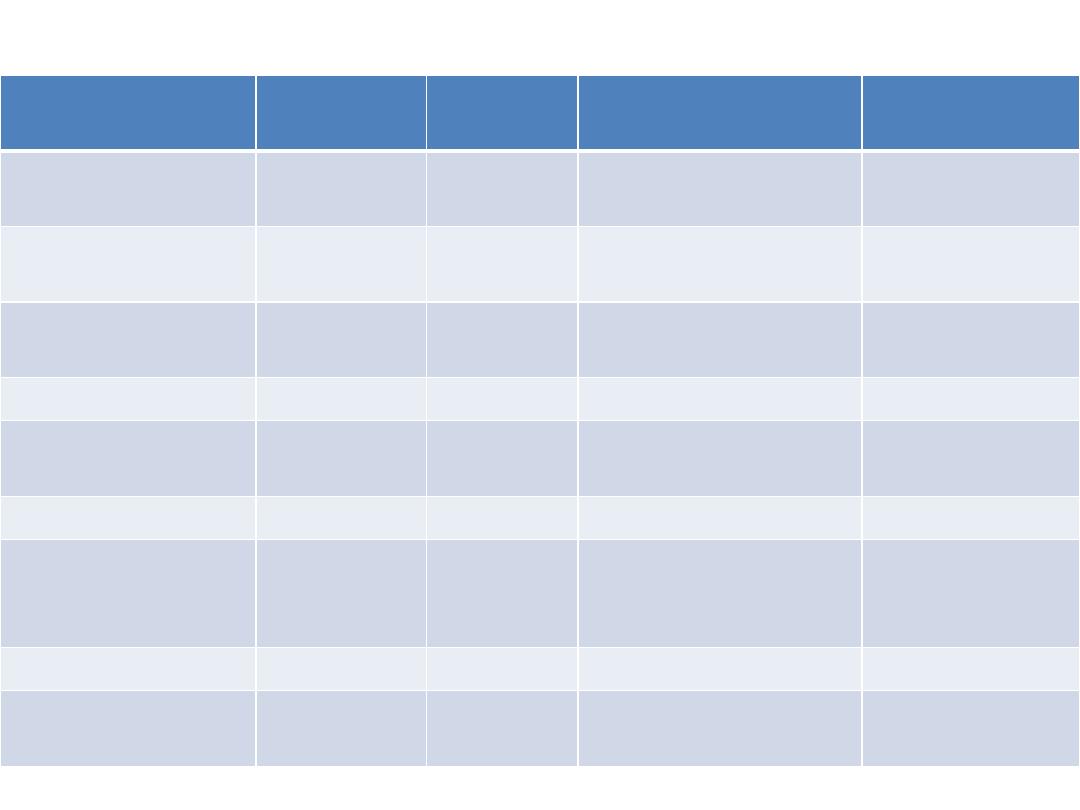
Scleroderma Autoantibodies
Antigen
ANA
Pattern
Frequency
Clinical
Associations
Organs Involved
Scl-70
(topoisomerase 1)
Speckled
10-40
dcSSC
Lung fibrosis
RNA Polymerase III
Speck/Nuc
4-25
dcSSC
Renal, Pulmonary
HTN
Centromere
Centromere
15-40
lcSSc, CREST
Pulmonary HTN
Esophageal
U1-RNP
Speckled
5-35
lcSSC, MCTD
Muscle
U3 RNP (fibrillarin)
Nucleolar
1-5
dcSSC, poor prognosis
Muscle
Pulmonary HTN
PM-SCL
Nucleolar
3-6
Overlap, mixed
Muscle
Th/To
Nucleolar
1-7
lcSSc
Pulmonary HTN,
Lung fibrosis,
Small bowel
Anti U11/U12
Nucleolar
1-5
lcSSc & dcSSC
Lung Fibrosis
Anti-Ku
1-3
Overlap Ssc
Muscle, Joint, SLE
overlap
Adapted from: Nihtyanova SI, Denton CP. Nat Rev Rheumatol 2010; 6:112

Scleroderma Treatment
• Depends on clinical manifestations
• Aggressive disease versus stable disease
• Reversible inflammation vs Vasoconstriction.
• Organ Involvement
• Treatment is directed at organ involved.

Raynaud’s
• Calcium Channel Blockers: nifedipine
• Nitroglycerin patches
• Sildenafil (Viagra) (but not in combination with
nitroglycerine) –usually for refractory Raynaud’s.
• Parental vasodilators (iloprost) – for severe disease
with impending digital ischemia.

Gastrointestinal Involvement
• GERD
• Proton pump inhibitor.
• Delayed Gastric Emptying and peristalis
disorders
• Supportive
• Promotilants are sometimes used.

Pulmonary Involvement
• Interstitial Lung Disease: with active
inflammation
• Mycophenolate
• Azithioprine
• Cytoxan - IV
• plus lower dose of steroids if RNA Poly III neg (ie 10
mg daily); avoid steroids if RNA Poly III positive.
• Pulmonary Hypertension
• Vasodilators: bosentan, sildenafil, epoprostenol,
treprostinil, iloprost.
• Lung Heart Transplant

Myositis
• Polymyositis overlap or MCTD
• Similarly to myositis alone with methotrexate,
azathioprine in combination of low dose
steroids.
• Tend to keep prednisone dose at around 10
mg or less to avoid risk of renal crisis.

Cardiac Involvement
• Pericarditis:
• NSAIDs
• Drainage of effusion if tamponade
• Myocarditis with elevated CK-MB & troponin
• If CAD is excluded, MRI and biopsy confirms, then
treatment would generally be with low dose
prednisone (10 mg/day) and cytoxan; nifedipine may
also be helpful.

Skin Disease
• Stable disease: no treatment
• Advancing diffuse skin involvement:
• Methotrexate
• Mycophenolate
• Current trial with Tocilizumab (Actemra)
• D-penicillamine 125 mg/day.
• Research on various anti-fibrosis therapies is
being performed (imatinib, Gleevac).

Differential Diagnosis
• Scleredema
• No Raynauds, negative antibodies, seen in IDDM
• Proximal skin thickening (trunk, shoulders, back)
• Scleromyxedema
• Skin thickening/induration on head, neck, arms, trunk
• Monoclonal gammopathy (multiple myeloma/AL amyloid)
• Skin biopsy differentiates.
• Endocrinologic: diabetes and hypothyroid myxedema
• Can be associated with skin induration.
• In diabetes can have sclerodactyly (Diabetic Cheiroarthropathy) -
dorsal
• POEMS (polyneuropathy, organomegaly, endocrinopathy,
monoclonal gammopathy, skin thickening).

• Nephrogenic Systemic fibrosis
• Chronic kidney disease and gadolinium MRI contrast
• Can involve hands and feet.
• Eosinophilic fasciitis:
• Hands and feet are spared, peripheral blood
eosinophilia, peau de orange appearance
• Diagnosis is via skin biopsy.
• Graft versus Host disease
• History of bone marrow transplant, no Raynaud’s
symptoms.
• Diagnosis is via skin biopsy.

Cases
Case 1
• 50 year old female who has CREST syndrome with anti-
centromere antibody:
• Raynaud’s controlled with nifedipine
• only digital skin thickening of the hands which is unchanged
• GERD on omeprazole
• telangiectasia.
• She currently has no complaints.
• Labs:
• CMP, CBC, ESR, CRP, total CK all normal, anti-centromere Ab
positivity.
• Echocardiogram and PFT’s 1 month ago:
• Echo: normal with normal estimated PA pressures.
• PFT’s: normal lung volumes, normal DLCO.
• What is next step:
Case 1
• Renew medications
• Nifedipine and omeprazole
• This case highlights the most typical case seen in
clinics with stable disease.
• Things to watch for:
• Change in skin disease
• Periodic echocardiogram and PFT’s.
• General exam

Case 2
• 60 year old male with Raynaud’s for 4 months prior to onset of skin
involvement
• Skin thickening has ascended to involve proximal extremities, chest, and abdomen within
1 year.
• The patient reports mild shortness of breath recently.
• Exam:
• Vitals: T 98.9, BP 124/73, pulse 80, resp rate 18
• Raynaud’s is noted without digital ulcer.
• Cardiovascular exam normal.
• Gastrointestinal exam is normal.
• Dry crackles noted at both bases.
• Extremities: no edema.
• Labs:
• CBC, CMP, total CK are all normal
• ESR 35, CRP 1.8 (upper limit of normal is 1.0).
• Anti-Scl-70 Ab positive, RNA Pol III negative.
• What is next step?

Case 2
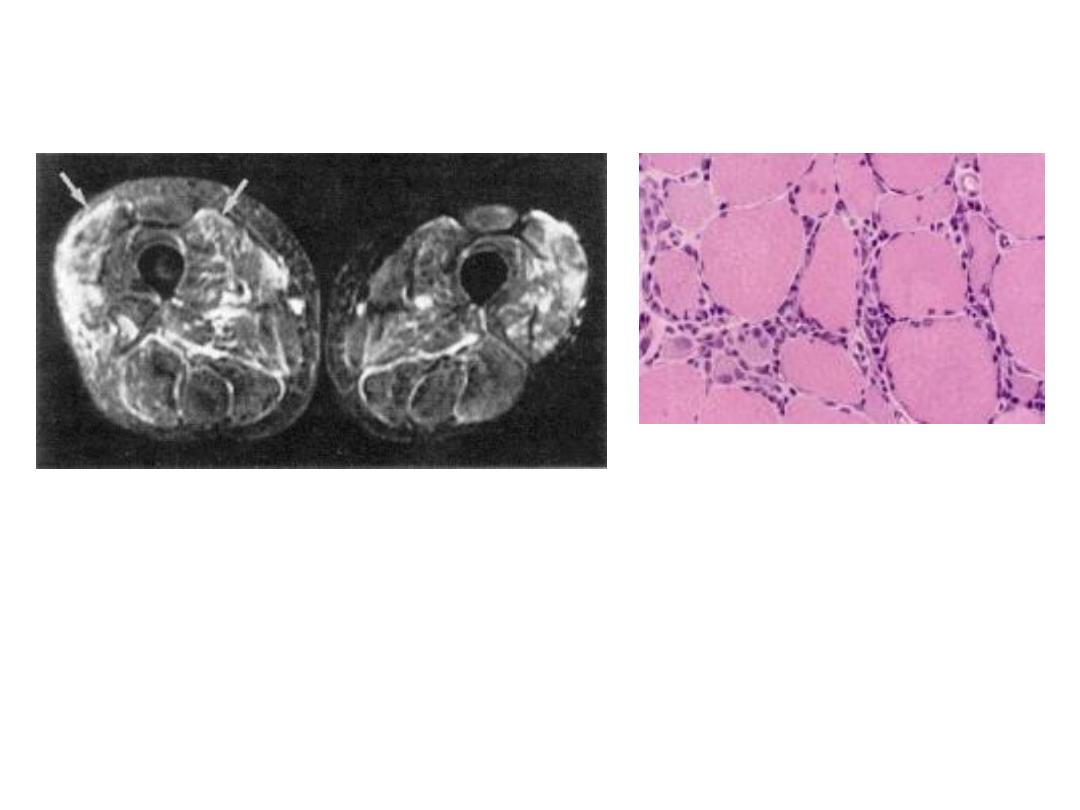
•
PFT’s: TLC decreased 80% to 55%, VC decreased 85% to 50%, RV decreased 83% to 62%, DLCO
decreased 75% to 45%.
•
Bronchoscopy performed: all cultures & cytology negative (neutrophils and eosinophils are
present).
•
Echocardiogram: no pulmonary hypertension.
•
Lung Biopsy shown on right.
•
What is the diagnosis? What is the treatment?
Learningradiology.com
Oikonomou A, Prassopoulos P - Insights Imaging (2012)
Strek, ME. Amer Col Chest
Physicians 2012

Case 2
• Interstitial lung disease associated with
scleroderma with active inflammation.
• Mycophenolate, Cytoxan, or Azathioprine
• Prednisone (low dose) 10 mg daily; gradual
taper

Case 3
• 50 year old female presents with
• onset of Raynaud’s for 1 year,
• developed skin thickening from the digits of the hands to just distal to the
elbows.
• She has noticed difficulty getting out of chairs and lifting objects
overhead.
• Exam:
• VS: Temp 98.2, BP 124/72, pulse 78, respiratory rate 16
• Cardiovascular and pulmonary exams normal.
• Gastrointestinal exam is normal.
• Muscle weakness of thighs and shoulder regions is noted.
• No skin lesions other than skin thickening.
• Labs:
• CBC, chem-7, ESR, CRP all normal, PM-SCL Ab positivity
• Total CK 3000 (mostly CKMM), AST 158, ALT 105, GGT normal.
• What is the next step?
Case 3
• MRI of the thigh
• Biopsy of thigh musculature
• What is the diagnosis? What is the treatment?
EMG, Nerve Conduction Studies
Olsen NJ, et al. Rheum Dis Clin N. Amer 1996;22(4):783-796
Seidman, RJ. Medscape

Case 3
• Scleroderma/Myositis overlap.
• Methotrexate or Azathioprine
• Low dose prednisone: 10 mg daily
• Over the next few months, CK levels normalize
and prednisone dose is gradually tapered, and
the patient’s strength improves.

Case 4
• 35 year old female with
• limited scleroderma for 3 years, anti-centromere Ab positive.
• with stable skin disease involving the digits of the hands
only; new “rash” appeared 1 month ago, gradually
worsening, no change in last week.
• Raynaud’s have been quite severe, but not on therapy.
• Exam
• VS: Temp 97.9, BP 123/76, pulse 82, RR 16
• Cardiac, pulmonary, gastrointestinal exams normal, no
edema
• Skin: see next slide
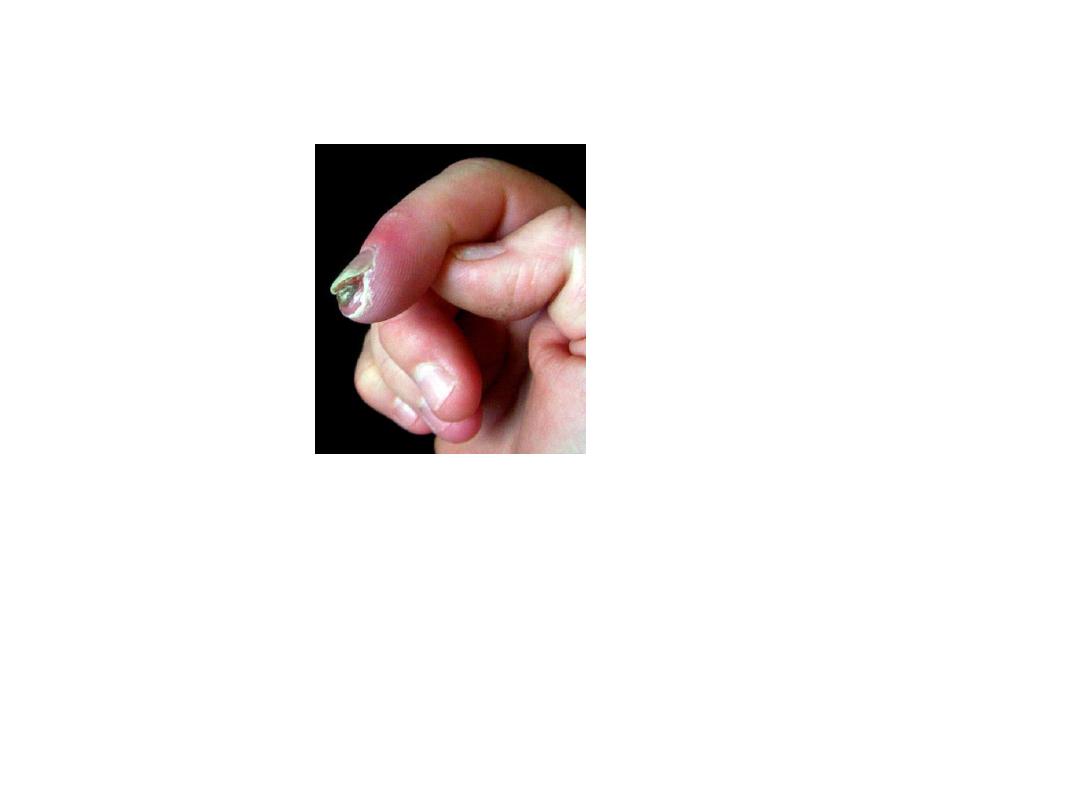
Case 4
• Labs:
• CBC, CMP, ESR, CRP all normal; anti-centromere Ab
positive, anti-phospholipid Ab neg, echo with bubble
study negative
• What is the diagnosis? What is next step?
Sclero.org
International Scleroderma Network

Case 4
• Digital Ischemia due to Raynaud’s
• Start calcium channel blocker
• Nifedipine 30 mg PO daily.
• Close follow-up and increase dose of nifedipine as
blood pressure tolerates.
• If not responding:
• Can start nitroglycerin patch or can start sildenafil (not
both).

Case 5
• 58 year old male with:
• Rapid onset scleroderma with Raynaud’s for 6 months then
skin thickening that spread to proximal arm, proximal thigh,
chest, and abdomen within 1.5 years.
• Blood pressure generally runs 110/70
• has mild headache, and has noticed some swelling of the
legs.
• Exam:
• VS: Temp 98.4, BP 160/105, pulse 70, RR 16.
• Cardiac, pulmonary, gastrointestinal exam all normal;
neurologic exam is non-focal.
• There is only mild bilateral lower extremity edema.

Case 5
• Labs
• Creatinine 2.0 (baseline is 0.6), CBC normal, ESR and
CRP normal, urine with 1+ protein, no RBC or WBC;
known to be RNA Pol III positive.
• What is the diagnosis? What is the next step.

Case 5
• Scleroderma Renal Crisis
• Treatment:
• Hospitalization
• Start ACE-inhibitor: captopril with dose escalation.

References
• Medscape
• Up To Date
• Desai, et al; Curr Opin Rheumatol 2011; 23:545-554
• Curr Opin Rheumatol 23;505-510
• Fischer A; CHEST 2006; 130:976 –981
• Rheum Dis Clin N Am;2003;29:293–313
• Arthritis Rheum 2006;54:3962-3970
• Rheumatology 2009;48:iii32–iii35
• Steen VD; Rheum Dis Clin N Am 2003;29:315–333
• Hudson M, et al; Medicine 2010;89:976-981
• Bon LV; Curr Opin Rheumatol 2011;23:505–510
• Barnes J; Curr Opin Rheumatol 2012, 24:165–170
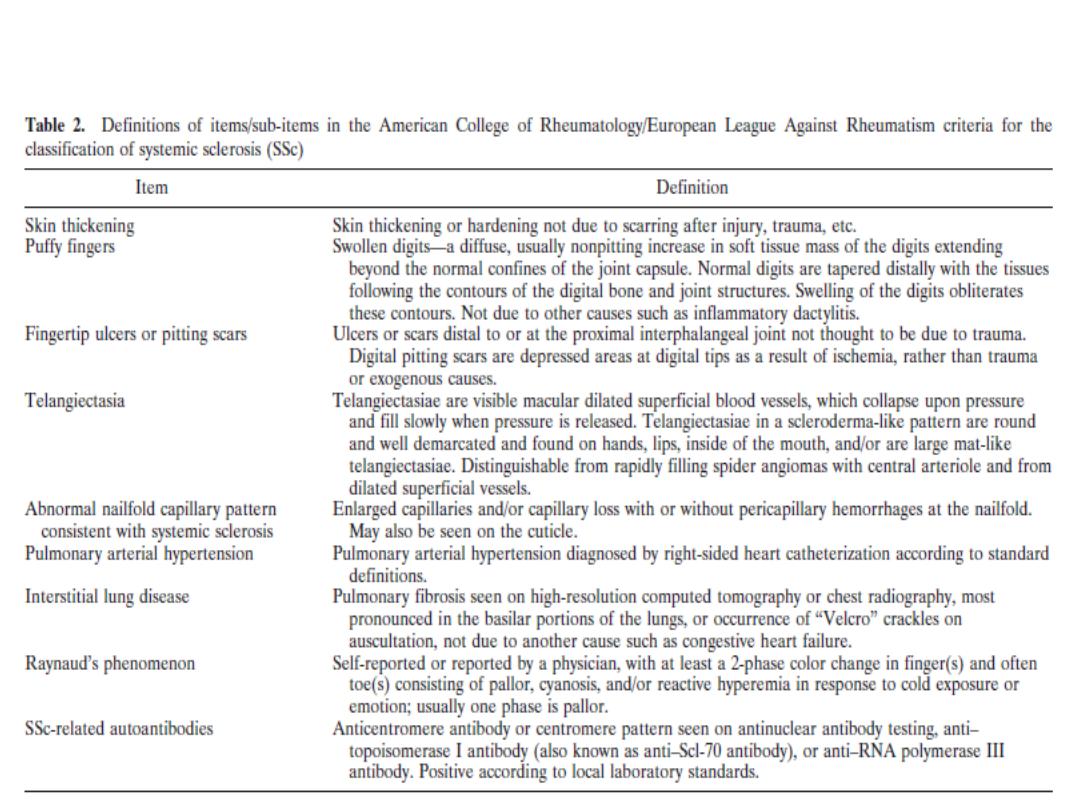
Definition of Criteria
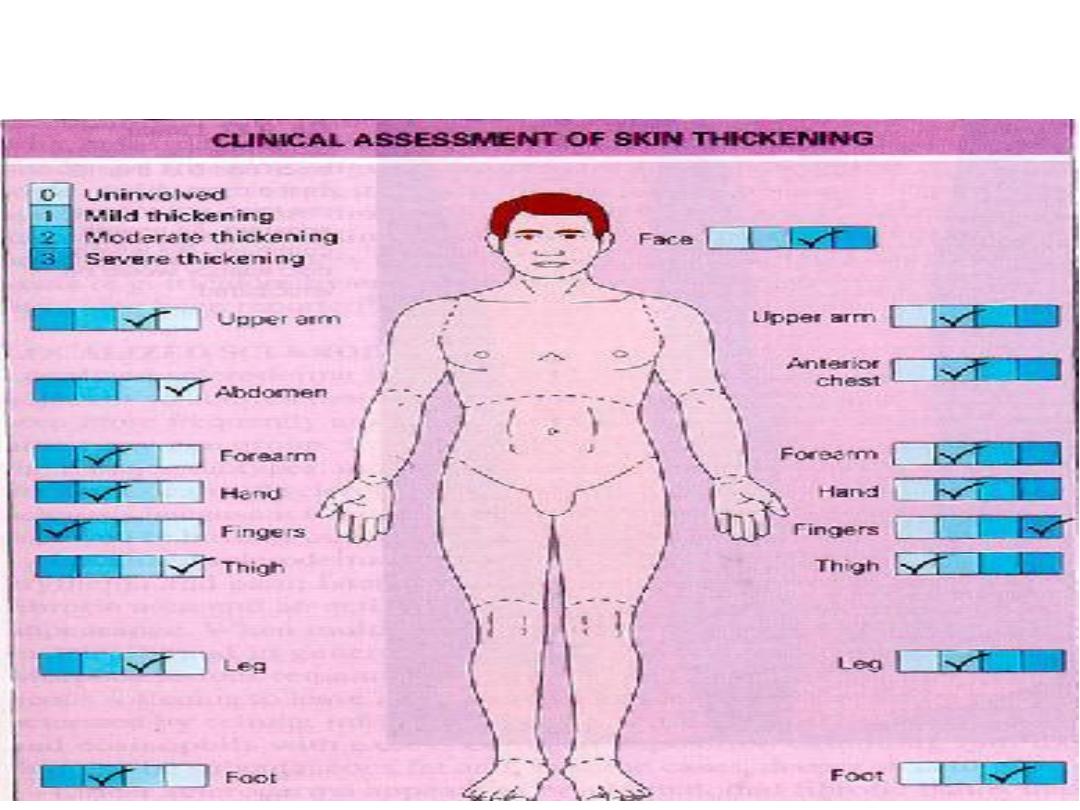
Skin Scoring
