
Obsessive-Compulsive and Related Disorders
د.وليد عزيز العميدي
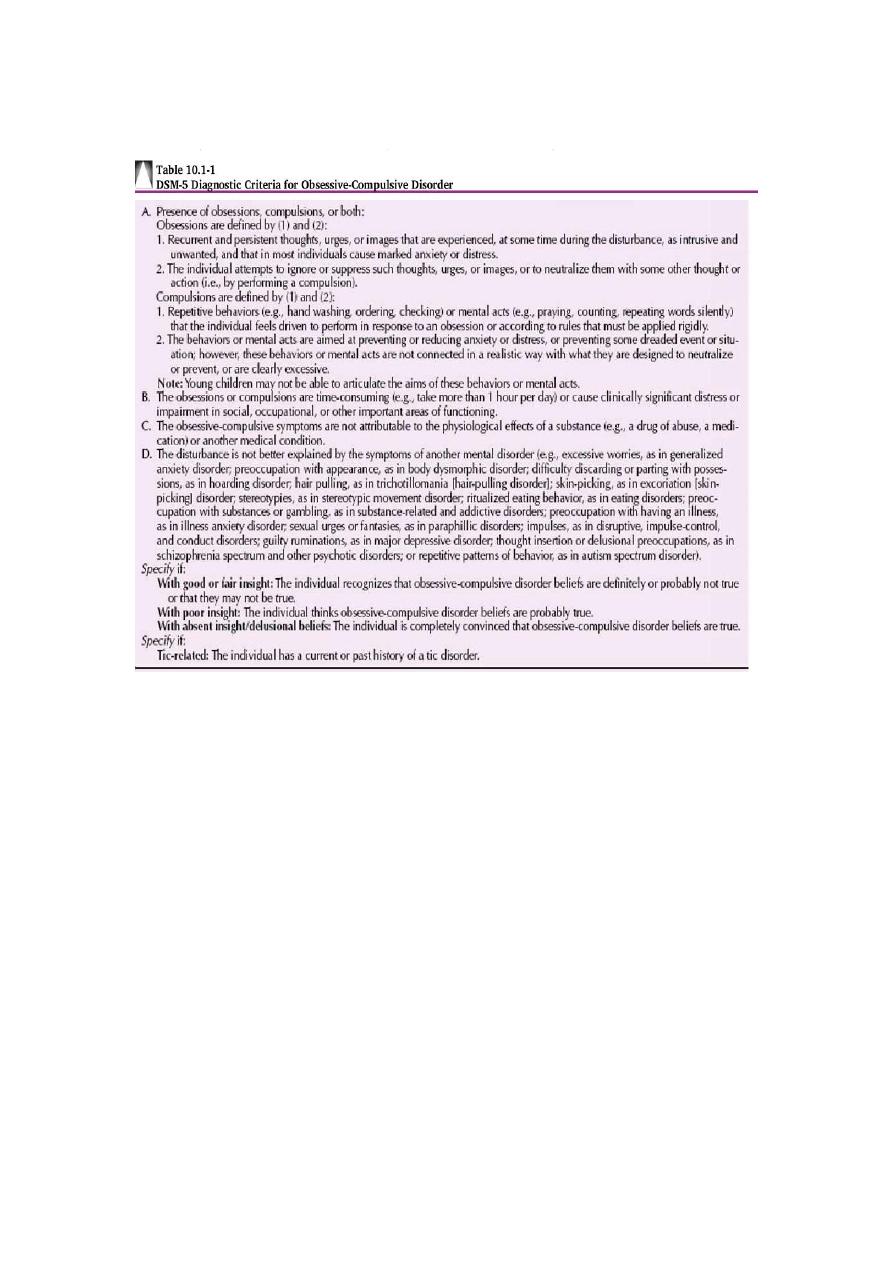
Obsessive-compulsive disorder (OCD) is represented by a diverse group of symptoms
that include intrusive thoughts, rituals, preoccupations, and compulsions. A patient
with OCD may have an obsession, a compulsion, or both.
An obsession is a recurrent and intrusive thought, feeling, idea, or sensation. In
contrast to an obsession, which is a mental event, a compulsion is a behavior.
Specifically, a compulsion is a conscious, standardized, recurrent behavior, such as
counting, checking, or avoiding. A patient with OCD realizes the irrationality of the
obsession and experiences both the obsession and the compulsion as ego dystonic
(i.e., unwanted behavior). Although the compulsive act may be carried out in an
attempt to reduce the anxiety associated with the obsession, it does not always
succeed in doing so.
EPIDEMIOLOGY : The rates of OCD are fairly consistent, with a lifetime
prevalence in the general population estimated at 2 to 3 percent. Among adults, men
and women are equally likely to be affected, but among adolescents, boys are more
commonly affected than girls. The mean age of onset is about 20 years, although men
have a slightly earlier age of onset (mean about 19 years) than women (mean about 22
years).
ETIOLOGY
1-
Biological Factors
SEROTONERGIC SYSTEM. : Data show that serotonergic drugs are more
effective in treating OCD than drugs that affect other neurotransmitter systems.
Brain-Imaging Studies: Various functional brain-imaging studies—for example,
positron emission tomography (PET)—have shown increased activity (e.g.,
metabolism and blood flow) in the frontal lobes, the basal ganglia (especially thexz
dsAERQDF caudate), and the cingulum of patients with OCD. Both computed
tomographic (CT) and magnetic resonance imaging (MRI) studies have found
bilaterally smaller caudates in patients with OCD.
Genetics : Relatives of probands with OCD consistently have a threefold to fivefold
higher probability of having OCD or obsessive-compulsive features than families of
control probands.
2-
Behavioral Factors
According to learning theorists, obsessions are conditioned stimuli. A relatively
neutral stimulus becomes associated with fear or anxiety through a process of
respondent conditioning by being paired with events that are noxious or anxiety
producing. Thus, previously neutral objects and thoughts become conditioned stimuli
capable of provoking anxiety or discomfort.
3-
Psychosocial Factors
Personality Factors. OCD differs from obsessive-compulsive personality disorder,
which is associated with an obsessive concern for details, perfectionism, and other
similar personality traits. Most persons with OCD do not have premorbid compulsive
symptoms, and such personality traits are neither necessary nor sufficient for the
development of OCD. Only about 15 to 35 percent of patients with OCD have had
premorbid obsessional traits.
Symptom Patterns :
OCD has four major symptom patterns:
Contamination. The most common pattern is an obsession of contamination,
followed by washing or accompanied by compulsive avoidance of the presumably
contaminated object. The feared object is often hard to avoid (e.g., feces, urine, dust,
or germs). Patients may literally rub the skin off their hands by excessive hand
washing or may be unable to leave their homes because of fear of germs.
Pathological Doubt. The second most common pattern is an obsession of doubt,
followed by a compulsion of checking. The obsession often implies some danger of
violence (e.g., forgetting to turn off the stove or not locking a door). The checking
may involve multiple trips back into the house to check the stove, for example. These
patients have an obsessional self-doubt and always feel guilty about having forgotten
or committed something.
Intrusive Thoughts. In the third most common pattern, there are intrusive
obsessional thoughts without a compulsion. Such obsessions are usually repetitious
thoughts of a sexual or aggressive act that is reprehensible to the patient.
Symmetry. The fourth most common pattern is the need for symmetry or precision,
which can lead to a compulsion of slowness. Patients can literally take hours to eat a
meal or shave their faces.

Other Symptom Patterns. Religious obsessions and compulsive hoarding are
common in patients with OCD. Compulsive hair pulling and nail biting are behavioral
patterns related to OCD. Masturbation may also be compulsive.
Treatment :
Pharmacotherapy
Selective Serotonin Reuptake Inhibitors : fluoxetine (Prozac), fluvoxamine ,
paroxetine , sertraline (Zoloft), citalopram —has been approved for the treatment of
OCD.
Clomipramine: Of all the tricyclic and tetracyclic drugs, clomipramine is the most
selective for serotonin reuptake versus norepinephrine reuptake and is exceeded in
this respect only by the SSRIs.
Other Drugs: If treatment with clomipramine or an SSRI is unsuccessful, many
therapists augment the first drug by the addition of valproate (Depakene), or
carbamazepine (Tegretol). Other drugs that can be tried in the treatment of OCD are
venlafaxine and the monoamine oxidase inhibitors (MAOIs), especially phenelzine .
Other pharmacological agents for the treatment of unresponsive patients include
buspirone and clonazepam . Adding an atypical antipsychotic such as risperidone has
helped in some cases.
Behavior Therapy : The principal behavioral approaches in OCD are exposure and
response prevention. Desensitization, thought stopping, flooding, implosion therapy,
and aversive conditioning have also been used in patients with OCD.
Other Therapies :
For extreme cases that are treatment resistant and chronically debilitating,
electroconvulsive therapy (ECT) and psychosurgery are considerations. ECT should
be tried before surgery. A psychosurgical procedure for OCD is cingulotomy, which
may be successful in treating otherwise severe and treatment-unresponsive patients.
Other surgical procedures (e.g., subcaudate tractotomy, also known as capsulotomy)
have also been used for this purpose.
Body Dysmorphic Disorder :
Body dysmorphic disorder is characterized by a preoccupation with an imagined
defect in appearance that causes clinically significant distress or impairment in
important areas of functioning. If a slight physical anomaly is actually present, the
person’s concern with the anomaly is excessive and bothersome.
DIAGNOSIS
The DSM-5 diagnostic criteria for body dysmorphic disorder stipulate preoccupation
with a perceived defect in appearance or overemphasis of a slight defect. It also
stipulates that at some point during the course of the disorder, the patient performs
compulsive behaviors (i.e., mirror checking, excessive grooming) or mental acts (e.g.,
comparing their appearance to that of others). The preoccupation causes patients
significant emotional distress or markedly impairs their ability to function in
important areas. The most common concerns involve facial flaws, particularly those
involving specific parts (e.g., the nose). Other body parts of concern are hair, breasts,
and genitalia.

TREATMENT
Treatment of patients with body dysmorphic disorder with surgical, dermatological,
dental, and other medical procedures to address the alleged defects is almost
invariably unsuccessful. Although tricyclic drugs, monoamine oxidase inhibitors
(MAOIs), and pimozide (Orap) have reportedly been useful in individual cases, other
data indicate that serotonin-specific drugs—for example, clomipramine (Anafranil)
and flouoxetine (Prozac)—reduce symptoms in at least 50 percent of patients.
In any patient with a coexisting mental disorder, such as a depressive disorder or an
anxiety disorder, the coexisting disorder should be treated with the appropriate
pharmacotherapy and psychotherapy
Hoarding Disorder
Compulsive hoarding is a common and often disabling phenomenon associated with
impairment in such functions as eating, sleeping, and grooming. Hoarding may result
in health problems and poor sanitation, particularly when hoarding of animals is
involved, and may lead to death from fire or falling. The disorder is characterized by
acquiring and not discarding things that are deemed to be of little or no value,
resulting in excessive clutter of living spaces. It is commonly driven by an obsessive
fear of losing important items that the person believes may be of use at some point in
the future, by distorted beliefs about the importance of possessions, and by extreme
emotional attachment to possessions.
Hair-Pulling Disorder (Trichotillomania)
Hair-pulling disorder is a chronic disorder characterized by repetitive hair pulling,
leading to variable hair loss that may be visible to others.
The disorder is similar to obsessive compulsive disorder and impulse control in that
there is increased tension prior to the hair pulling and a relief of tension or
gratification after the hair pulling. Before engaging in the behavior, patients with hair-
pulling disorder may experience an increasing sense of tension and achieve a sense of
release or gratification from pulling out their hair. All areas of the body may be
affected, most commonly the scalp Other areas involved are eyebrows, eyelashes,
and beard.
Excoriation (Skin-Picking) Disorder : Excoriation or skin-picking disorder is
characterized by the compulsive and repetitive picking of the skin. It can lead to
severe tissue damage and result in the need for various dermatological treatments.
Throughout history, skin-picking disorder has had many names: skin-picking
syndrome, emotional excoriation, nervous scratching artifact and epidermotillomania,
DSM-5 diagnostic criteria for skin-picking disorder requires recurrent skin-picking
resulting in skin lesions and repeated attempts to decrease or stop picking. The skin-
picking must cause clinically relevant distress or impairment in functioning. The skin-
picking behavior cannot be attributed to another medical or mental condition and
cannot be a result of a substance use disorder (e.g., cocaine or methamphetamine use
).
The face is the most common site of skin-picking . Other common sites are legs, arms,
hands, fingers, and scalp. Although most patients report having a primary picking
area, many times they pick other areas of the body in order for the primary area to
heal. In severe cases, skin-picking can result in physical disfigurement and medical
consequences that require medical or surgical interventions (e.g., skin grafts or
radiosurgery).
