Immune Response
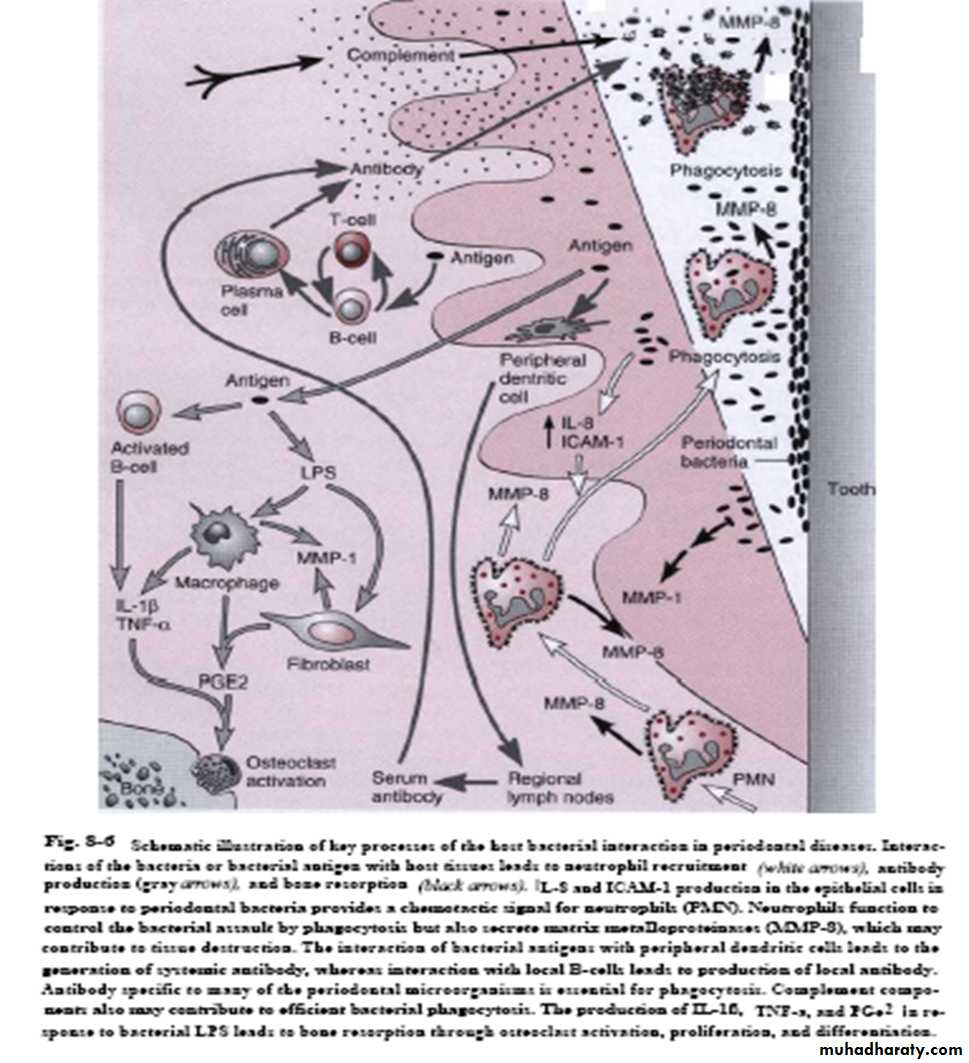
Immune response-ImmunityDefined as: the response of host to the presence and activities of MOs. It protects tissue against local microbial attack & prevent their spreading to become systemic & life threatening, however, it will cause cellular and tissue damage (sacrifice the local tissues)
Immune response-Immunity
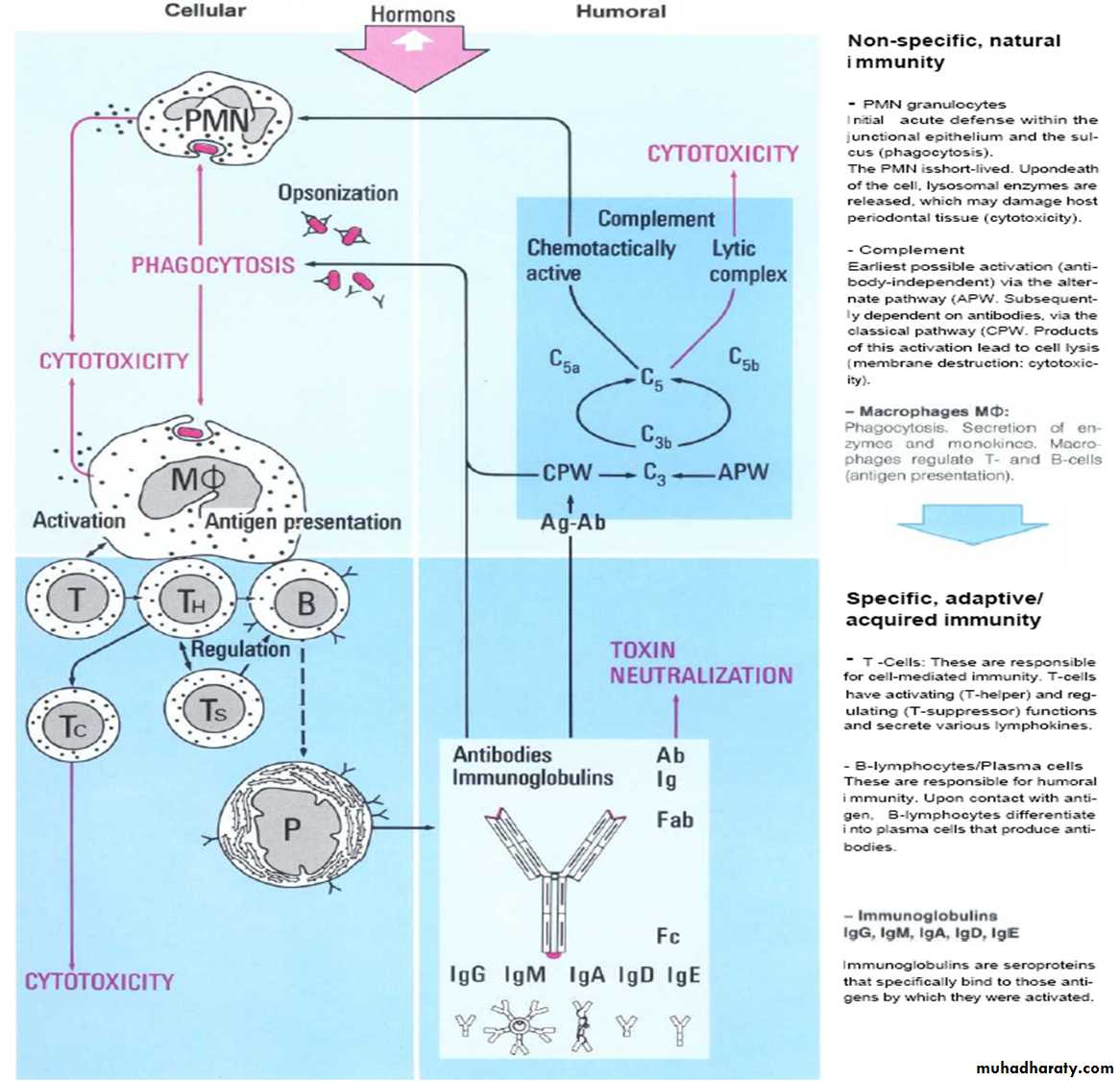
Innate immunity, early or first response, PNLPNL + cytokines+ chemokines + MO and their products (antigens) will stimulate, help and focus the adaptive immunity
We have 2 types of adaptive immune responses
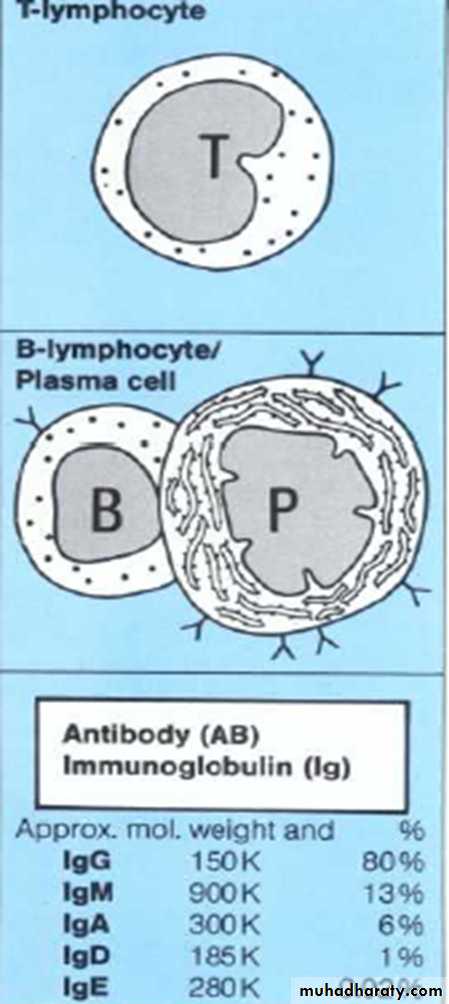
The humoral or anti-body-mediated by plasma cells & B cells
The cellular mediated by T-lymphocytes and their lymphokines
Immune response-Immunity
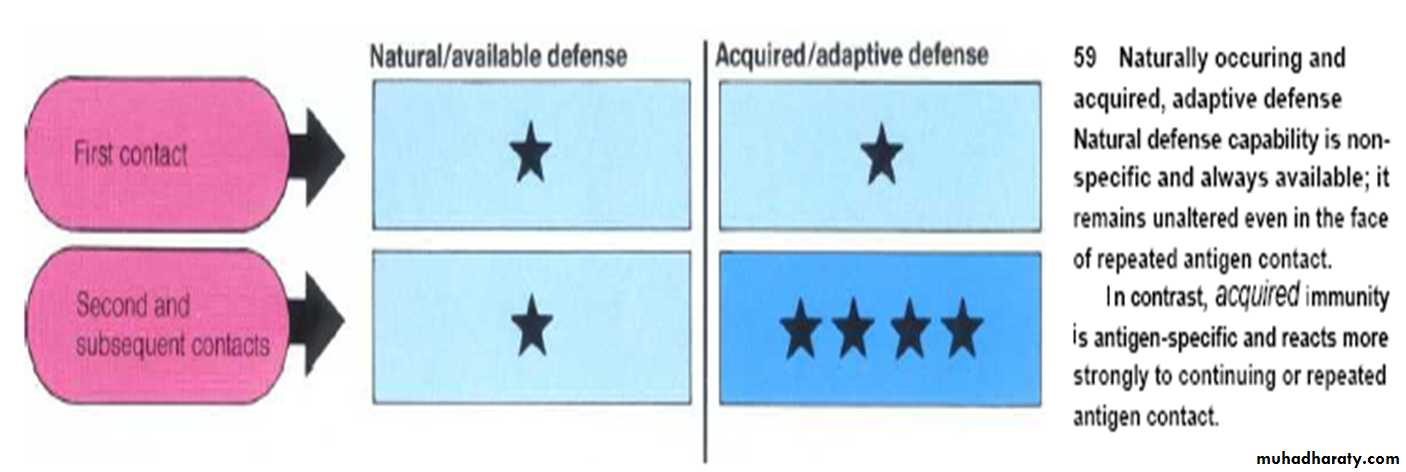
• Immune response take 2 paths:• 1. Non-specific path:1st line of defense, is the innate immune response which don’t adapt with repeated exposure to same pathogen
• ex; phagocytic cell that posses a no. of inherently antimicrobial proteins that kill many or different pathogens rather than a specific one
• 2. Specific path: Humoral & Cellular (adaptive IR) increase after exposure to pathogen, the ability of B &T cells to recognize specific structure on a pathogen & generate progeny that also recognize the structure enable IR to respond more rapidly & effectively when exposed to same pathogen again
Immune response-Immunity
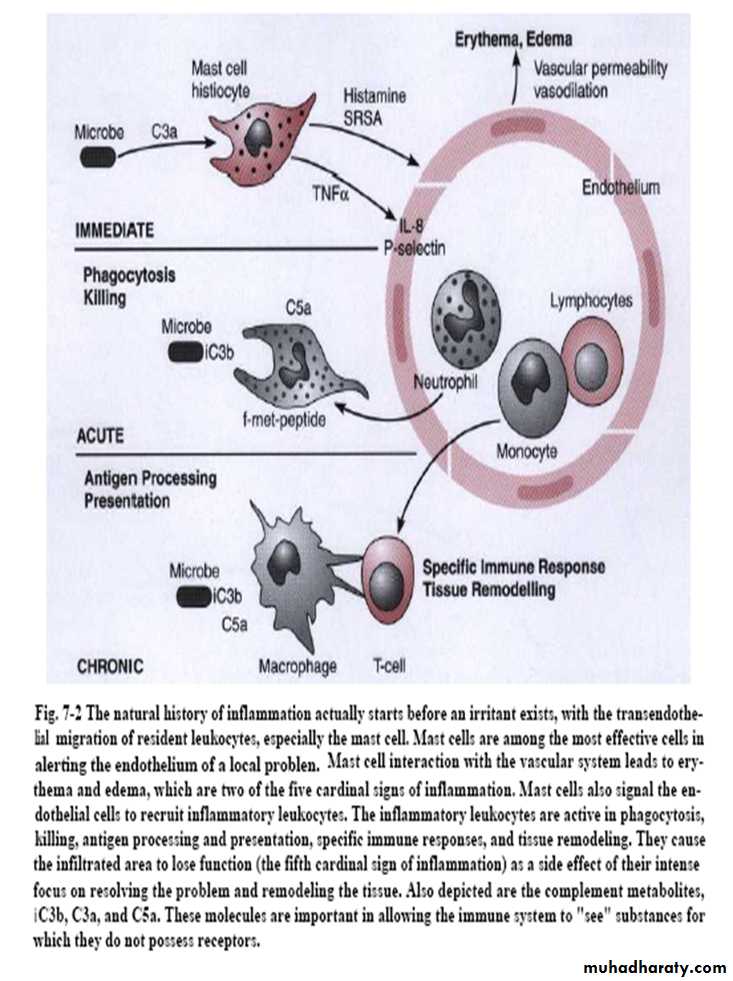
Antigen: Is a substance which is able to elicit an IR when it is introduced into a hostLeukocytes: Originate in bone marrow & exit from the blood by trans-endothelial migration under normal conditions accounting for resident Leukocytes found in tissue
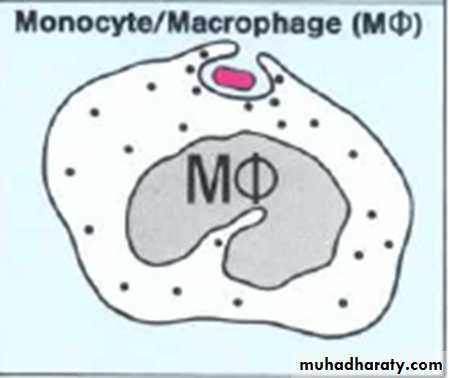
• Most important resident Leukocytes are the mast & monocyte cells that transmit information which initiates the process of immediate inflammation followed within minutes by a short –living period (up to several hours) of acute inflammation where Neutrophils move to area
Immune response-Immunity
If the problem not resolved,• inflammation shall pass to
• chronic which is
• characterized by migration
• of lymphocytes and
• macrophages to local tissue
•
Cells of the immune system
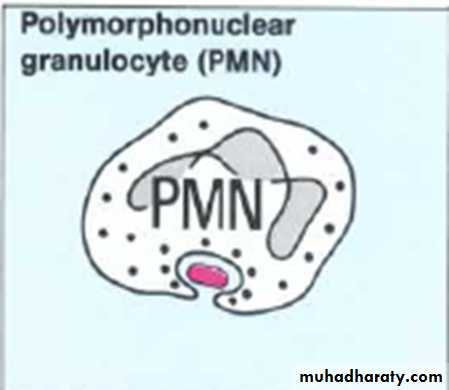
• Cells mainly involved in immune response:Nonspecific
phagocytic cells includes
• Eosinophils
• 2. Macrophage (MNL)
• 3. Neutrophils (PNL)
Mediator cells includes: (basophiles, mast cells & platelets)
Specific immune response cells
Plasma cell
B & T lymphocytes
Cells of the immune system
•Tissue destruction
• Immune response has both• Protective
• &
• Destructive
• Which is either
• *Direct through bacteria and their products (exogenous)
• *Indirect through endogenous mediators
Exogenous mediators
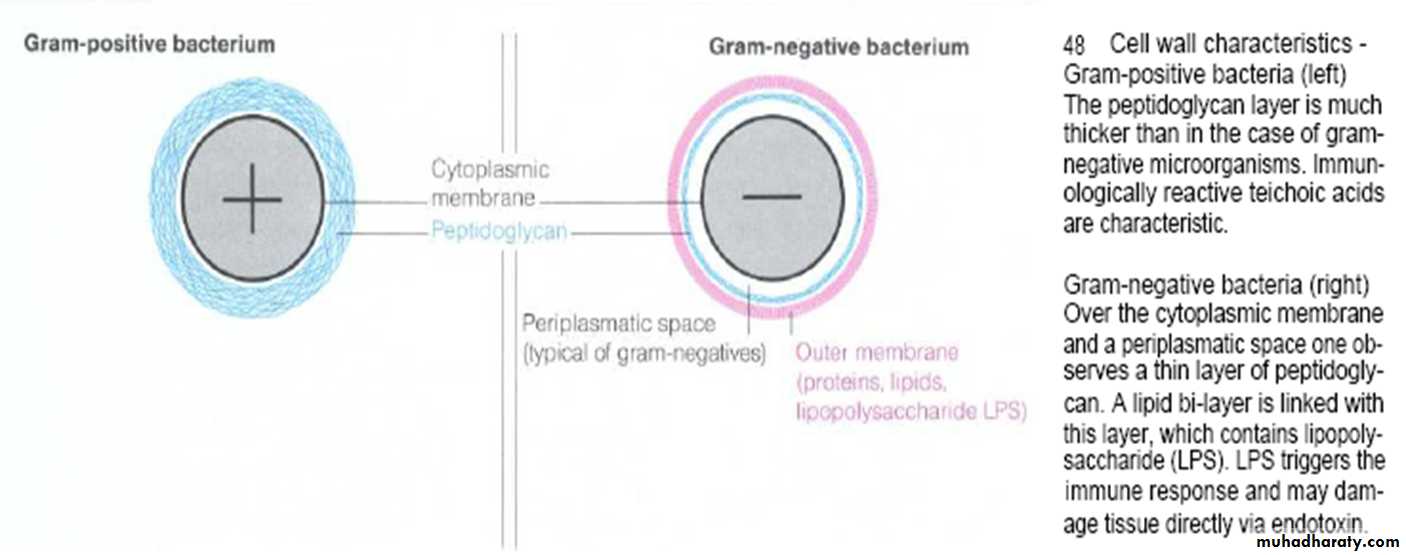
• 1. MO metabolites (byproducts): organic, acids (such as lactic, formic, acetic), NH3, H2S• 2. G-ve toxins: Endotoxins such as lipopolysacharide (LPS)
• 3. G+ve toxins: Such as peptidoglycan
• 4. MO enzymes: Such as protease, collagenase, hyaluronidase, & elastase
• 5. Leukotoxin secreted by A.a
• 6. Extracellular macromolecules such as dextran
•
Exogenous mediators
Some bacterial products inhibit the growth or alter the metabolism of the host tissue cells. Includes a no. of metabolic byproducts such as: volatile sulfur compounds, fatty acids , ammonia & peptidesIn addition to enzymes that are capable of destructing all host cells & intercellular-matrix molecules like enzymes that degrade collagen, fibronectin & AB that facilitate bacterial invasion
• Examples of bacterial enzymes:
• Collagenase by P.g. & A.a.
• Keratinase by P.g. &T.denticola Fibronectin-degrading enzyme By P.g. & P.i
• Phospholipase A by P.i. & P.melaninogenica
Endogenous mediators
• 1- Vasoactive amines• 2- Cytokines
• 3- Lysosomal components or enzymes
• 4- O2 derived metabolites (oxygen radicals)
• 5- Arachidonic acid (AA) derivatives:
• prostaglandins & leukotrienes
• 6- Plasma proteases, complements & kinin
• 7- Neutral proteases
Destruction mechanisms
• Destructive phase of immune response• What is called hypersensitivity reactions defined as IRs that are excessive or that are not appropriate to the challenge
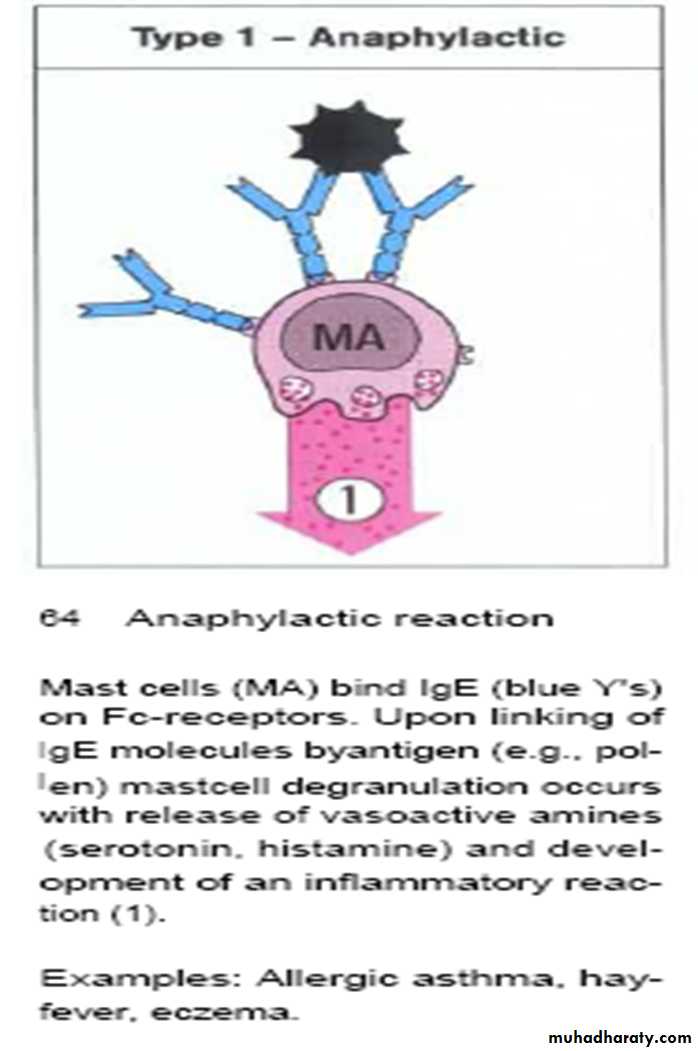
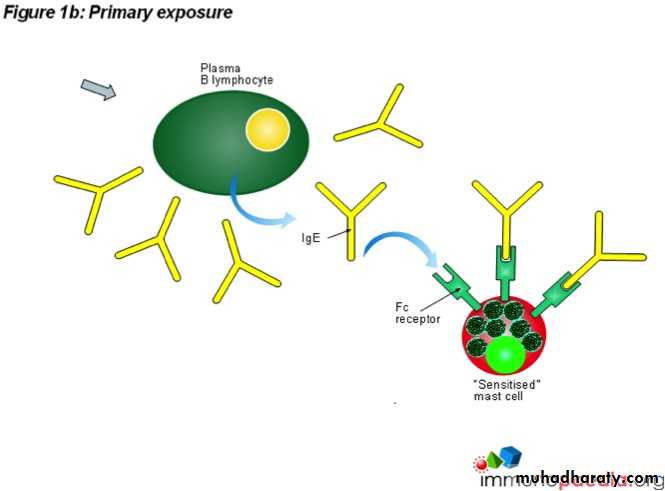
Type 1anaphylactic type of inflammatory injury or response
Occur when IgE fixed to mast cell or basophile on the fc portion react with antigen, will lead to mast cell degranulation
As mast cell posses receptor for complements (C3a&C5a) & for fc portion of AB molecules (IgE & IgG)
Mast cell
Has prominent cytoplasmic granules known as lysosomes that store inflammatory mediatorsMast cell degranulation occur through :
• 1- Directly by bacteria
• 2- IgE
• 3- Immune complex
Mediators
• 1. Proteolytic enzymes• 2. Arachidonic acid (AA)
• 3. Heparin: induce bone resorption by potentiating parathyroid hormone
• 4. Alfa-2- macroglobulin (α2M) (synthesized in liver, & found in macrophages & fibroblasts) collagenase activator. Though it’s proteinase inhibitor, but α2M found to form complexes with collagenase-1 (MMP-1) during injury and inflammation
• 5. Slow-reacting substance of anaphylaxis or SRS-A: secreted from Mast cells during anaphylactic reaction. It mediates smooth muscles contraction & increases vascular permeability
Mediators
• 6. Bradykinin: smooth muscles contraction, vasodilation,
• increases capillary permeability, leukocytes migration &
• stimulate pain reception
• 7. Histamine: released by basophils, mast cell, platelets,
• endothelial cells & others. Causes smooth m.cont.,
• increases cap. perm., increases dilation & venules perm.,
• stimulation of exocrine glands, skin response
• (erythematous wheal or rash), & bone resorption
• 8. Serotonin
Mediators
• 9. Anti-collagenase inhibitors• 10. Prostaglandins: Their functions depends on their
• binding receptors on cells, for example: the may
cause constriction or dilation in vascular smooth muscle cells
cause aggregation or disaggregation of platelets
Significant correlation was found between incidence of type 1 inflammatory response (reaction) & the severity of PD diseases
• Examples of type 1 inflammatory reaction: Anaphylactic shock, Allergic asthma, Hay fever, & Eczema
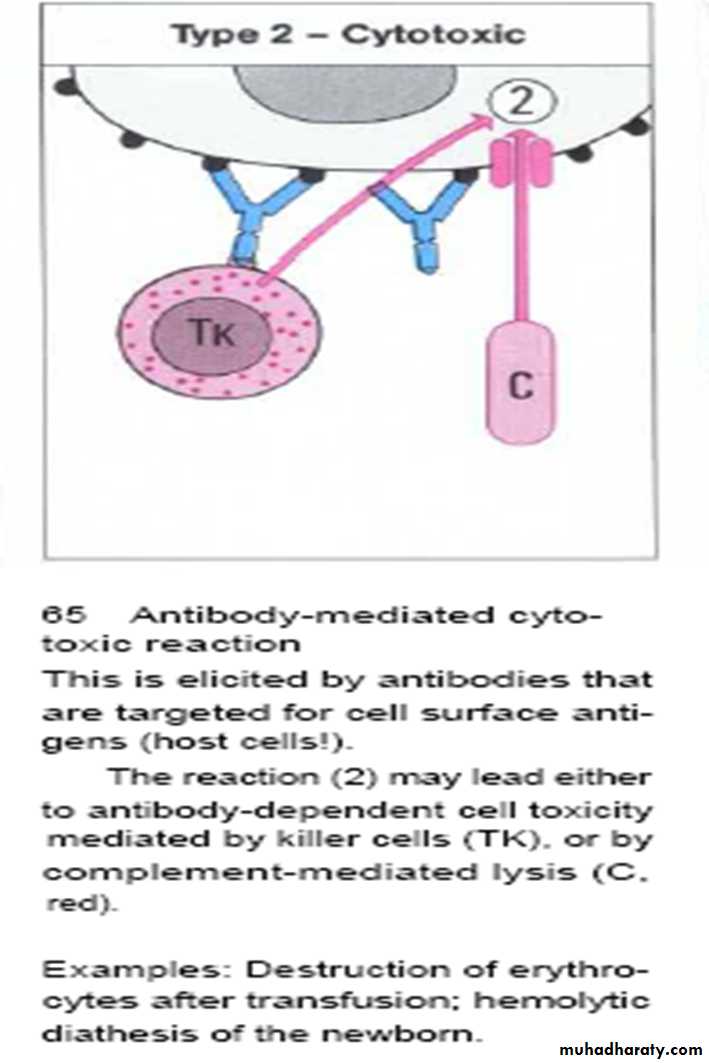
Type 2 cytotoxic inflammatory injury
Type II hypersensitivity is an antibody (AB)-mediated inflammatory response (cytotoxic reaction) in which specific antibodies bind to antigens, resulting in tissue damage or destruction
The resultant destruction of host cell due to activation of complements
IgG, IgM interaction with antigens on the surface of target cells leads to complement activation that form membrane attack complex
Active MAC is composed of the subunits C5b, C6, C7, C8 and several C9 molecules
Type 2 cytotoxic inflammatory injuryTarget cell destruction could also occur by:
Macrophages, PNL,T-killer cells that bound with fc portion of AB
It has not been proved in periodontal diseases
Examples: Auto-immune diseases,
Erythrocyte destruction after blood transfusionType 2 cytotoxic inflammatory injury
Theoretically, could happen in gingival lesion under the following circumstances:
• Antigen (AG) adsorbed onto the membrane of
host cell
2. AG closely similar the structure of host
membrane
3. Inflammatory or immune aberration produced
during long period of infection
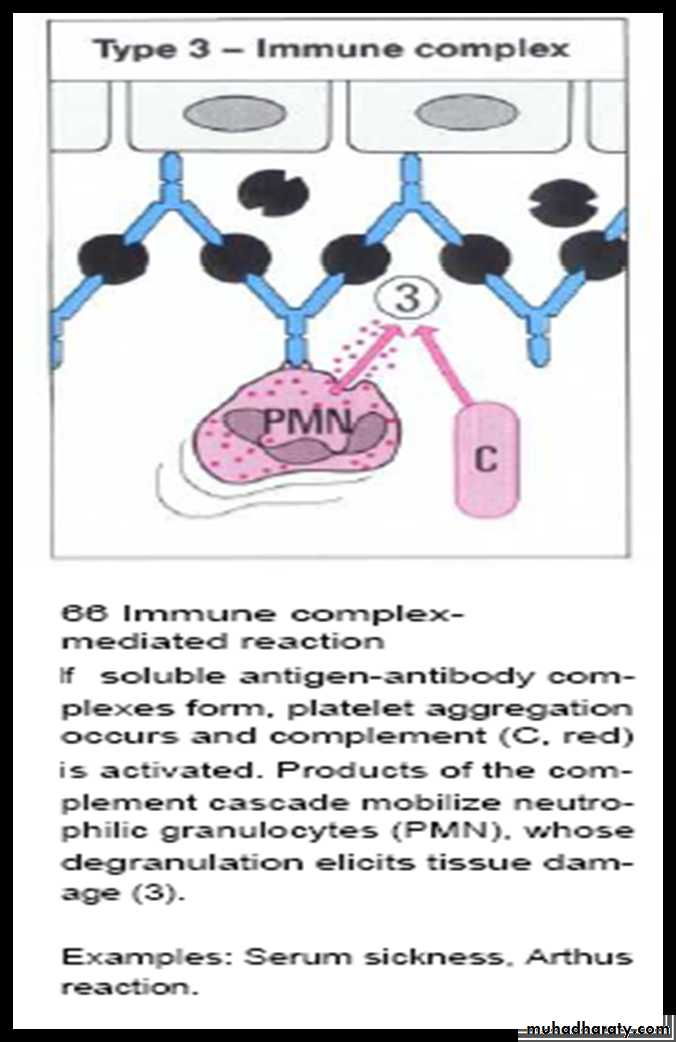
Type 3 Immune complex-mediated inflammatory injury
Interaction of AB (IgM) with AG that lead to formation of Immune complex which in turn activates the Complements that attract PNLPNL accumulated & phagocytize AB-AG complex with release of mediators thereby damaging host cells
Such reactions may progress to immune complex diseases
Its associated with loss of CT attachment, apical proliferation of JE & bone loss
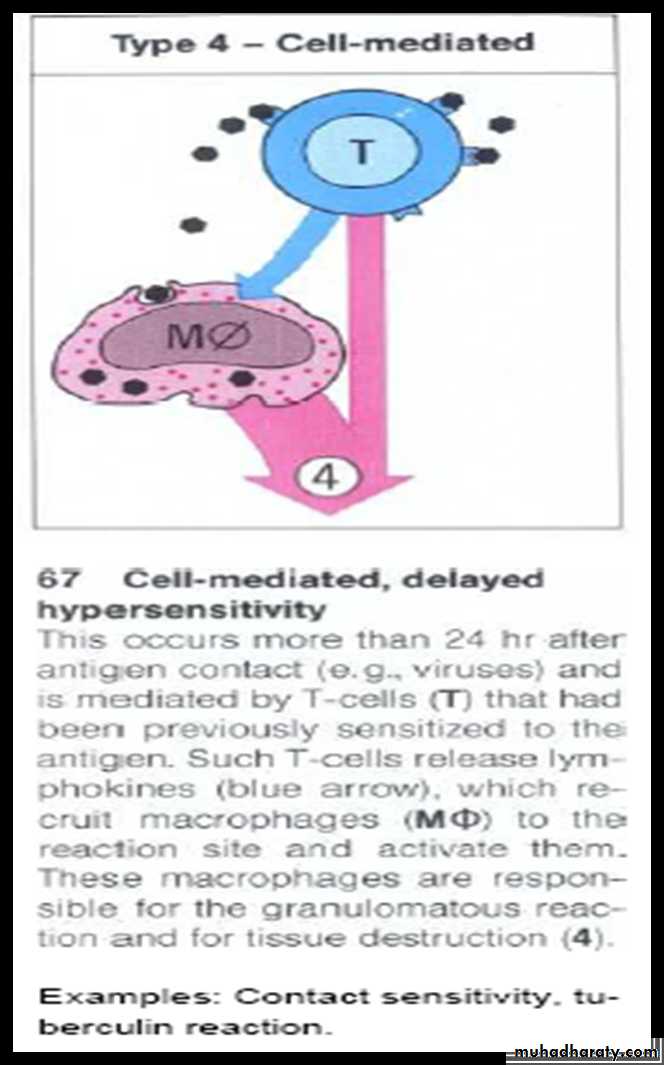
Example: Arthus reaction local vasculitis rarely reported after vaccinationType 4 cell mediated (delayed hypersensitivity) reaction
Interaction of AG with the surface of lymphocyte & macrophage with elaboration of effecter molecules which lead to the destruction of normal CT & its replacement by proliferating fibroblasts & small blood vessels (fibrosis)
It occurs more than 24h after AG contact & is mediated by T-cell that has been previously sensitized to AG
Cytokines, fibroblast chemotactic factor & fibroblast activating factor
Example: Contact sensitivity (contact dermatitis)