Pelvic ring injuries
• Mechanism of injury
• Often high energy injury( FFH, RTA).Sport injury
• Associated injuries common (chest, head, other
orthopaedic)
• Non pelvic sources of bleeding must be ruled out.
• Mortality usually related to non pelvic injuries
• Radiographs
• Anteroposterior pelvis
• CT
Classification
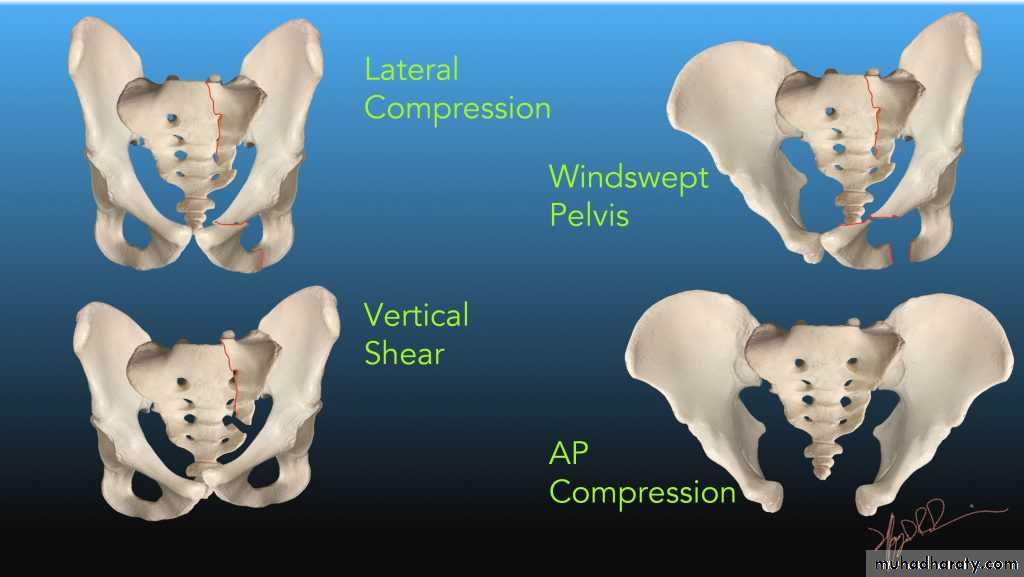
Young-Burgess based on injury mechanism.
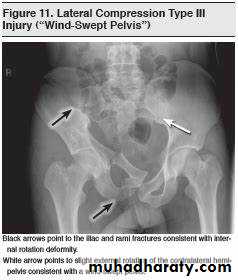
1- Lateral compression (LC)
2- Anteroposterior compression (APC)—all have symphyseal diastasis.
3- Vertical shear (VS)
Usually due to a fall. Vertical displacement of hemipelvis commonly with complete disruption of the SI joint.4- Combined mechanism
Associated injuries
APC pattern has associated urethral and bladder injuries.• Cause of death in LC pattern is primarily due to brain injury, whereas in APC, pattern is primarily due to shock, sepsis, and ARDS.
Tile classification—based on fracture stability
1-Stable (posterior arch intact)Avulsion fractures
ILiac wing fractures
Unstable (complete disruption of posterior arch)
Treatment• General principles
• Emergent treatment: control hemorrhage and
provisionally stabilize pelvic ring
• Important to establish and follow a treatment
protocol to avoid variation in treatment decision
making
85% of bleeding due to venous injury, only 15% arterial source
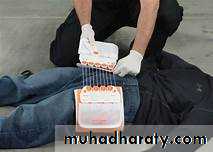
• Volume resuscitation and early blood transfusion• Pelvic binder or wrapped sheet.
• Angiographic embolization
• Pelvic packing, initially popularized in Europe, provides tamponade of venous bleeding.
• External fixation Place before emergent laparotomy
• Non operative treatment
• Indicated for stable fracture patterns
• Weight bearing as tolerated for isolated anterior
injuries
Operative treatment
• Indications• Symphysis diastasis greater than 2.5 cm.
•Vertical instability of posterior hemipelvis
• Sacral fracture with displacement greater than1 cm
Complications
• Severe life-threatening hemorrhage• Neurologic injury
• Urogenital injury/dysfunction
• Urethral stricture most common in men
• Dyspareunia and need for cesarean section childbirth common in women
• Malunion
• Nonunion
• DVT and/or pulmonary embolus
• DVT is the most common complication if thromboprophylaxis is not used.
• Infection—open fracture and associated contaminated
laparotomy
• Death