BIRTH ASPHYXIA
Birth asphyxia or hypoxia- ischemia:It refers to a signs & symptoms of hypoxia which means poor oxygen delivery to body organs.
*hypoxemia: which refers to an arterial oxygen concentration of less
than normal.and if hypoxemia is prolonged, cardiac and vascular compromise occur
result in hypotension causing:ischemia: which refers to a blood flow to cells or an organ that is
insufficient to maintain their normal function which will result inmore tissue hypoxia.
Eventually:
*Tissue anoxia occur which is a term used to indicate the consequencesof complete lack of oxygen.
Hypoxemia
Ischemia
Tissue anoxiaAfter an episode of hypoxia an anaerobic metabolism occurs and generates increased amounts of lactate and inorganic phosphates.
Increased amounts of intracellular sodium and calcium may result in tissue swelling and cerebral edema. There is also increased production of free radicals and nitric oxide in these tissues.
Etiology: Hypoxia-ischemia can occur before, during or after
delivery:-Intrauterine (prenatal) asphyxia: here there is no sufficient gas
exchange in the fetus through the placenta, occur in the followingconditions:-
- interuption of the umbilical circulation as in cord prolapse.
- poor perfusion of the maternal side of the placenta as in maternalhypotension, pre eclampsia, abruptio placentae.
- impaired maternal oxygenation as in asthma, pulmonary embolism or
pneumonia.
- impaired fetal oxygenation or perfusion as in fetomaternal
hemorrhage or fetal thrombosis.Causes of asphyxia during delivery:-
- Premature placental separation.- Inadequate relaxation of the uterus to permit placental filling as result
of uterine tetany caused by excessive use of oxytocine during labor.
- Impedence of the circulation of blood through the umbilical
cord as a result of compression or knotting of the cord.Causes of asphyxia after birth:-
- Anemia severe enough to lower the oxygen content of the blood to acritical level due to severe hemorrhage or hemolysis.
- Shock severe enough to interfere with the transport of oxygen to
vital cells as in adrenal hemorrhage, IVH, overwhelming infection, ormassive blood loss.
- Deficit in arterial oxygen saturation resulting from failure to breathe
adequately postnatally due to a cerebral defect, maternal medication
narcosis, or injury or due to neuromuscular disease as myasthenia
gravis or myopathy.
-Failure of oxygenation of an adequate amount of blood resulting from
severe forms of cyanotic congenital heart disease or deficientpulmonary function as hyaline membrane disease, neonatal pneumonia,
meconium aspiration, pneumothorax, diaphragmatic hernia, pulmonary
hypoplasia, or pleural effusion.
Clinical manifestations:-
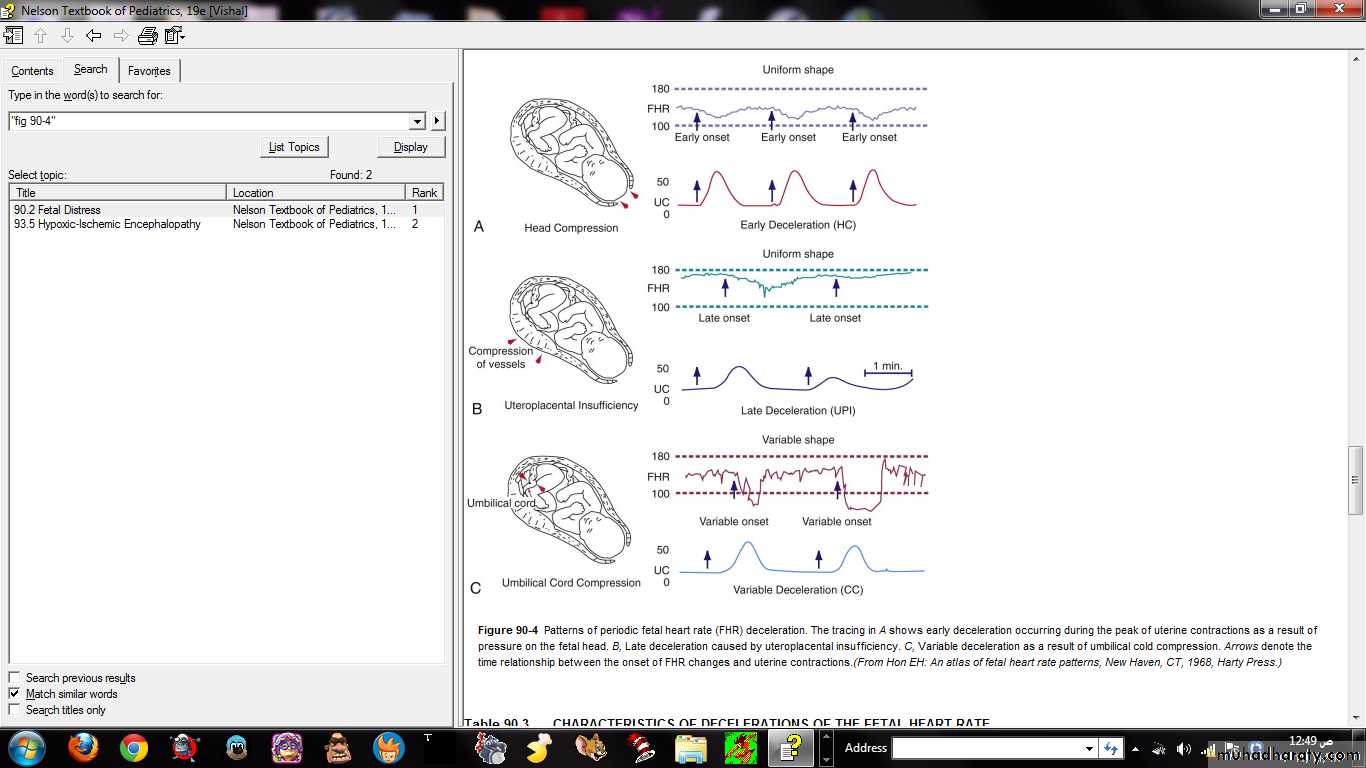
Intrauterine growth restriction with increased vascular resistance may be the 1st indication of fetal hypoxia. During labor, the fetal heart rate slows. Continuous heart rate recording may reveal a variable or late deceleration pattern particularly in infants near term.These signs should lead to the administration of high concentrations of oxygen to the mother and consideration of immediate delivery to avoid fetal death and CNS damage.
At delivery, the presence of meconium-stained amniotic fluid is evidence that fetal distress has occurred. At birth, affected infants may be depressed and may fail to breathe spontaneously, having low APGAR scoring. During the ensuing hours, they may remain hypotonic or change from a hypotonic to a hypertonic state, or their tone may appear normal.
Pallor, cyanosis, apnea, a slow heart rate, and unresponsiveness to stimulation are also signs of HIE.
Cerebral edema may develop during the next 24 hr and result in profound brainstem depression. During this time, seizure activity may occur; it may be severe and refractory to the usual doses of anticonvulsants. Though most often a result of the HIE, seizures in asphyxiated newborns may also be due to hypocalcemia, hypoglycemia, or infection.
Signs stage 1 stage 2 stage 3
-level of hyperalert lethargic stuporous,
consciousness coma
muscle tone normal hypotonic flaccid
posture normal flexion decerebratetendon hyperactive hyperactive absent
reflexes
Moro reflex strong weak absent
pupils dilated constricted unequal,poorresponse to
light
seizures none common decerebration
EEG normal low voltage suppression to
changing to isoelectric line
seizur activity
duration < 24 hours 24hr - 14 days days to weeks
outcome good variable death,severedeficits
Treatment:-
Selective cerebral or whole body (systemic) therapeutic hypothermia reduces mortality or major neurodevelopmental impairment in term and near-term infants with HIE.Hypothermia decreases the rate of apoptosis and suppresses production of mediators known to be neurotoxic, including extracellular glutamate, free radicals, nitric oxide, and lactate.
Additional therapy for infants with HIE includes supportive care directed at management of organ system dysfunction
Careful attention to ventilatory status and adequate oxygenation, blood pressure, hemodynamic status, acid-base balance, and possible infection is important.
Effects of asphyxia on different parts of the body
system effectscentral nervous hypoxic ischemic enceohalopathy,
system infarction intracranial hemorrhage,
seizures, cerebral edema, hypotonia
hypertonia.
Cardiovascular myocardial infarction, poor
contractility tricuspid insufficiently
hypotention.
Renal acute tubular or cortical necrosis
adrenal adrenal hemorrhageGIT perforation, ulceration, necrosis
metabolic inappropriate ADH secretion,hyponatremia, hypoglycemia,
hypocalcemia, myoglobinuria.