
Vertigo and
Dizziness
DR. AMMAR MOHAMMED
2016/2017
Vertigo and Dizziness
Prevalence
1 in 5 adults report dizziness in last month
Increases in elderly
Worsened by decreased visual acuity, proprioception and
vestibular input
Dizziness
Non-specific term
Different meanings to different people
Could mean
-
Vertigo
- Syncope
- Presyncope
-
Weak
- Giddiness
- Anxiety
-
Anemia
- Depression
- Unsteady

Vertigo and Dizziness
Vertigo
Perception of movement
Peripheral or Central
Syncope
Transient loss of consciousness with loss of postural
tone
Vertigo and Dizziness
Presyncope
Lightheadedness-an impending loss of
consciousness
Psychiatric dizziness
Dizziness not related to vestibular dysfunction
Disequilibrium
Feeling of unsteadiness, imbalance or sensation of
“floating” while walking

Pathophysiology
Normally there is balanced input from both
vestibular systems
Vertigo develops from asymmetrical vestibular
activity
Abnormal bilateral vestibular activation results in
truncal ataxia

Vertigo and Dizziness
Nystagmus
Rhythmic slow and fast eye movement
Direction named by fast component
Slow component due to vestibular or brainstem activity
Slow component usually ipsilateral to diseased structure
Fast component due to cortical correction
Physiologic Vertigo
“motion sickness”
A mismatch between visual, proprioceptive and
vestibular inputs
Not a diseased cochleovestibular system or CNS
Vertigo-Characteristics
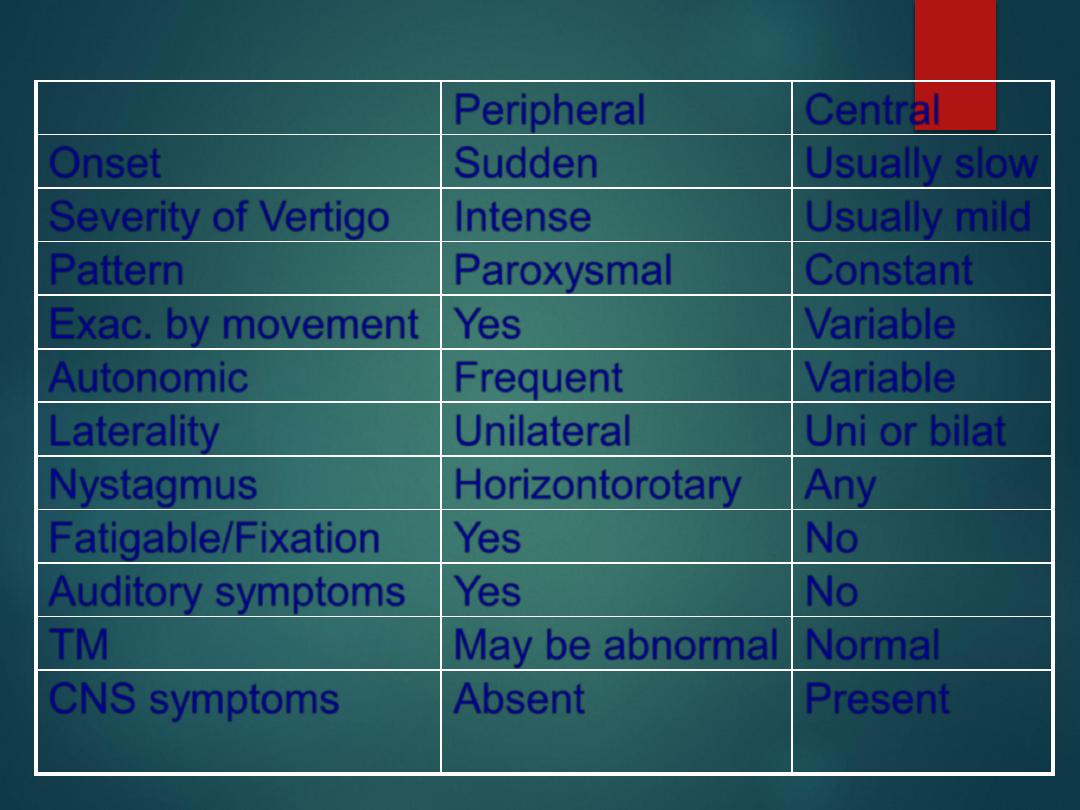
Peripheral
Central
Onset
Sudden
Usually slow
Severity of Vertigo
Intense
Usually mild
Pattern
Paroxysmal
Constant
Exac. by movement Yes
Variable
Autonomic
Frequent
Variable
Laterality
Unilateral
Uni or bilat
Nystagmus
Horizontorotary
Any
Fatigable/Fixation
Yes
No
Auditory symptoms
Yes
No
TM
May be abnormal Normal
CNS symptoms
Absent
Present
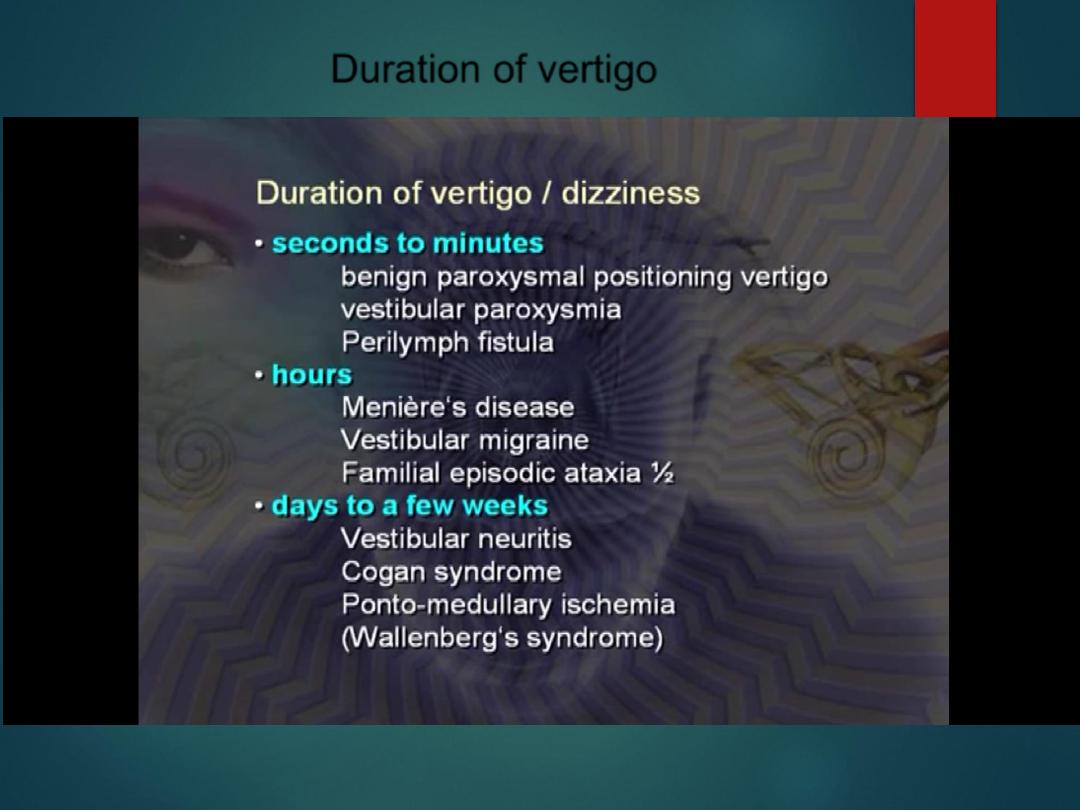
Duration of vertigo
Duration
BPPV
Seconds, always < 1 min
VBI
Few minutes,
focal neurological signs
Migraine Varies sec, minutes, hours or days
Meniere’s
20 minutes to hours
Vest.neuritis
Days
Stroke
Days

Vertigo-Physical Exam
Cerumen/FB in EAC
Otitis media
Pneumatic otoscopy
Tympanosclerosis or TM
perforation
Nystagmus
Fundoscopic exam
Pupillary abnormalities
Extraocular muscles
Cranial nerves
Auscultate for carotid bruits
Orthostatic vital signs
BP and pulse in both arms
Gross hearing
Weber-Rinne test
External auditory canal
vesicles
Gait and Cerebellar function

Investigations
CT-if cerebellar mass, hemorrhage or infarction
suspected
Glucose and ECG in the “dizzy” patient
Cold caloric testing
Angiography for suspected VBI
MRI
Electronystagmography and audiology

Benign Paroxysmal Positional Vertigo
Extremely common
Otolithic calcium carbonate crystals
become loose, and fall into the posterior
semicircular canal
No hearing loss or tinnitus
Short-lived episodes brought on by rapid
changes in head position
Usually a single position that elicits vertigo
Less pronounced with repeated stimuli
Typically can be reproduced at bedside
with positioning maneuvers
Vestibular paroxysmia
Due to neurovascular cross- compression
Short attacks of rotational vertigo
Treated by 200-600 mg/ day carbmazepine
Labyrinthitis
Associated hearing loss and tinnitus
Involves the cochlear and vestibular systems
Abrupt onset
Usually continuous

Oto-Toxic drugs
Due to toxic effects of medications
Still relatively common
Mild tinnitus and high frequency hearing loss
Vertigo in acute phase
Ataxia in the chronic phase
Common etiologies
-Aminoglycosides
-Vancomycin
-Erythromycin
-Barbiturates
-Phenytoin
-Furosemide
-Quinidine
-Salicylates
-Alcohol
Vestibular Neuronitis
Suspected viral etiology
Sudden onset vertigo that increases in intensity over several
hours and gradually subsides over several days
Mild vertigo may last for several weeks
May have auditory symptoms
Highest incidence in 3
rd
and 5
th
decades

Ménière Disease
First described in 1861
Triad of vertigo, tinnitus and hearing loss
Due to cochlea-hydrops
Unknown etiology
Possibly autoimmune
Abrupt, episodic, recurrent episodes with severe rotational
vertigo
Usually last for several hours
Acoustic Neuroma
Peripheral vertigo that ultimately
develops central manifestations
Tumor of the Schwann cells around
the 8
th
CN
Vertigo with hearing loss and tinnitus
Earliest sign is decreased corneal
reflex
Later truncal ataxia
Most occur in women during 3
rd
and
6
th
decades

Central Vertigo-Differential
Central Vertigo
Vertebrobasilar Insufficiency
Atheromatous plaque
Subclavian Steal Syndrome
Drop Attack
Cerebellar Hemorrhage
Multiple Sclerosis
Head Trauma
Neck Injury
Temporal lobe
seizure
Vertebral basilar
migraine
Metabolic
abnormalities
Hypoglycemia
Hypothyroidism

Head and Neck Trauma
Due to damage to the inner ear and central
vestibular nuclei, most often labyrinthine
concussion
Temporal skull fracture may damage the
labyrinth or eighth cranial nerve
Vertigo may occur 7-10 days after whiplash

Metabolic Abnormalities
Hypoglycemia
Suspected in any patient with diabetes with
associated headache, tachycardia or anxiety
Hypothyroidism
Clinical picture of vertigo, unsteadiness, falling,
truncal ataxia and generalized clumsiness

Management
Based on differentiating central from
peripheral causes
VBI should be considered in any elderly patient
with new-onset vertigo without an obvious
etiology
Neurological or ENT consult for central vertigo
Suppurative labrynthitis-admit and IV
antibiotics
Toxic labrynthitis-stop offending agent if
possible

Management
Severe Ménière disease may require
chemical ablation with gentamicin
Attempt Epley maneuver for BPPV
Mainstay of peripheral vertigo
management are antihistamines that
possess anticholinergic properties
-Meclizine
-Diphenhydramine
-Promethazine
-Droperidol
-Scopolamine
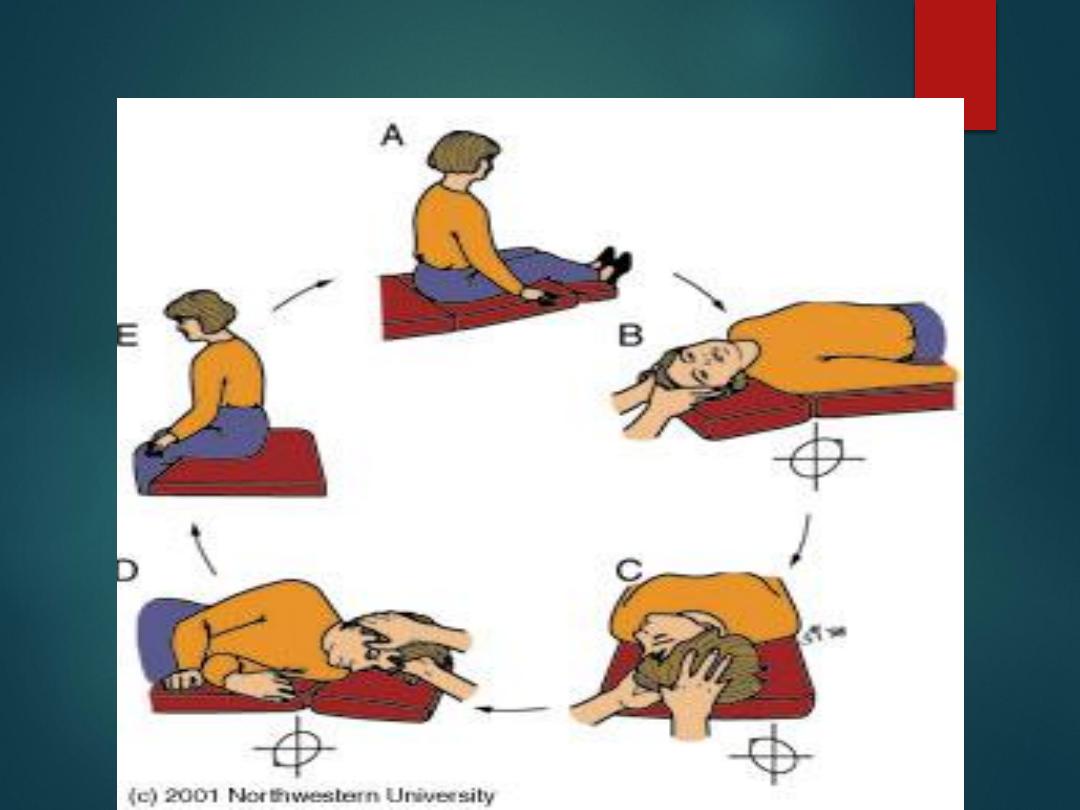
Epley Maneuver

Summary
Ensure you understand what the
patient means by “dizzy”
Try to differentiate central from
peripheral
Often there is significant overlap
Not every patient needs a head CT
Central causes are usually insidious
and more severe while peripheral
causes are mostly abrupt and benign
Most can be discharged with
antihistamines
