Paranasal Sinus Neoplasms
Paranasal sinus neoplasms, both benign and malignant, are found relatively rarely in the head and
neck. Malignant neoplasms of the paranasal sinuses account for approximately 3.0% of head and neck
cancers and 0.5% of all malignant tumors.. In general, these tumors are identified and treated at
advanced stages as their symptoms usually mimic benign inflammatory conditions. The most common
malignant neoplasm of the nose and paranasal sinuses is squamous cell carcinoma. This tumor most
commonly arises from the maxillary antrum and secondarily from the ethmoid sinus
Clinical Findings
Symptoms and Signs
The presenting symptoms are
nasal obstruction,
rhinorrhea,
and sinus congestion.
facial pain and epistaxis.
In addition, symptoms related to the orbit, such as diplopia, proptosis, visual loss, and
epiphora, can occur with either a neoplastic invasion or expansion into the orbit.
Entry through the skull base into the anterior cranial fossa can lead to the symptoms of
headache, cranial neuropathies, and occasional frontal lobe symptoms (such as personality
alterations).
Tumors can also invade the maxilla and present as a hard-palate mass.
Physical Examination
Nose and Paranasal Sinus
1- mass that often fills the nose. Polyps or polypoid mucosa may be overlying the mass.
2- The septum can be markedly deviated to the contralateral side because of the expansion of the
neoplasm;
3- sometimes the tumor can erode into the contralateral nasal cavity.
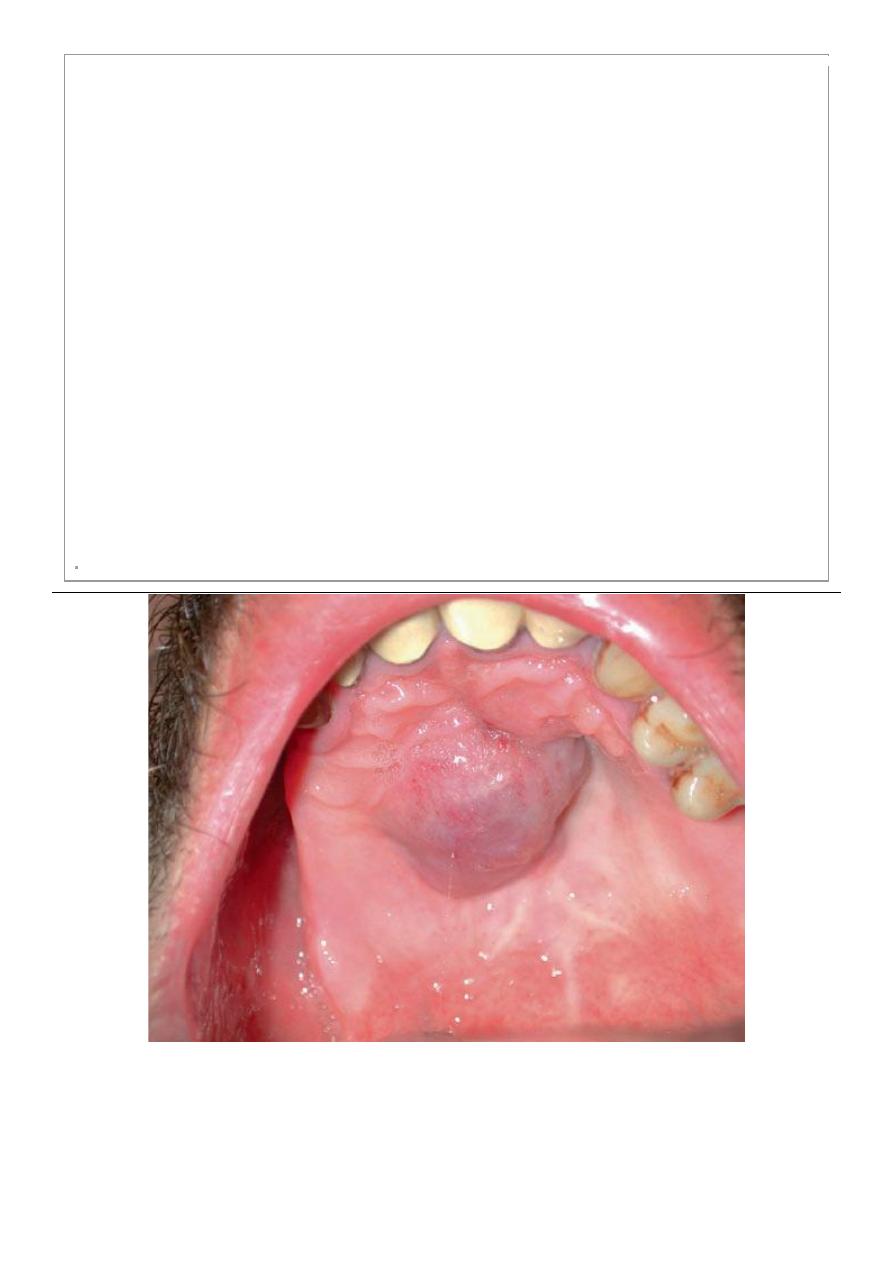
Oral Cavity
An expanded alveolar ridge or loose maxillary dentition indicates early bony invasion of the maxilla.
Sometimes a mass is seen on the hard palate, indicating frank invasion into the maxilla.
Face and Orbit
Facial swelling and thickening of the cheek and nose skin is an indication that the neoplasm
has invaded the soft tissue through the anterior bony walls.
Proptosis and/or Diplopia is commonly seen when the mass expands through the lamina
papyracea . Visual loss also can be a sign of orbital apex involvement with compression of the
optic nerve.
Cranial Nerves
Cranial nerve (CN) involvement is common in advanced malignant neoplasms of the paranasal
sinuses.
Other Physical Findings
serous otitis media, which is often due to eustachian tube involvement,
and neck masses due to metastatic neoplastic spread into the regional lymph nodes. The most
commonly involved lymph nodes are the upper jugulodigastric nodes.
Imaging Studies
A computed tomography (CT) scan can delineate the mass well and can be sufficient for both bony
and benign diseases. It is excellent for determining bony invasion but is limited in its inability to
distinguish between edematous mucosa and tumor involvement.
Magnetic resonance imaging (MRI) with both T1- and T2-weighted images with gadolinium
enhancement is superior in determining the true involvement of the anterior cranial fossa, the skull
base, and the orbit. MRI is also superior at soft-tissue delineation, can distinguish a tumor from
obstructed secretions in the sinus.
Biopsy
If the mass is large enough for easy visualization in the physician's office, then a biopsy can be
obtained with biopsy forceps through a transnasal route.
Differential Diagnosis
The most common benign lesion of the paranasal sinuses is the inverted papilloma. The most
common malignant neoplasm of the paranasal sinuses is squamous cell carcinoma. Additional
tumors that are frequently seen are adenocarcinoma, adenoid cystic carcinoma, olfactory
neuroblastoma, malignant mucosal melanoma, and sinonasal undifferentiated carcinoma.
Benign Neoplasms
Inverted Papillomas
An inverted papilloma, also called a schneiderian papilloma from the name of the mucosa from
which it arises, is typically located on the lateral nasal wall; rarely is it found on the septum. The
incidence of this tumor is between 0.5% and 7.0% of all nasal tumors.
Inverted papillomas typically involve the middle meatus and the most common sinuses involved are
the maxillary and ethmoid sinuses, followed by the sphenoid and frontal sinuses.
Inverted papillomas are usually unilateral, but they have been reported to be bilateral in up to 13% of
cases.Whether because of multicentricity or incomplete excision, these neoplasms have a high rate of
recurrence with any procedure—as high as 75%. Patients also have a 5–15% risk of developing
squamous cell carcinoma within the inverted papilloma.
Diagnosis
On gross examination, there are no clear distinguishing characteristics between an inverted papilloma
and an inflammatory polyp, although an inverted papilloma may be firmer and less translucent than an
"average" polyp. On histopathologic examination, however, one feature of inverted papillomas is
distinguishing: There is proliferation of the epithelium with fingerlike inversions into the underlying
epithelium.
Treatment
The treatment consists of total excision of the tumor.
An important feature in the management of patients with these neoplasms is that all of the excised
specimens should be closely examined with multiple sections to rule out invasive squamous cell
carcinoma.
Malignant Neoplasms
Squamous Cell Carcinomas
Squamous cell carcinoma is the most common malignant neoplasm of the paranasal sinuses,
accounting for 60–80% of paranasal sinus tumors.
The etiology and epidemiology of this tumor are poorly understood,. Nickel workers have a markedly
increased risk of developing a squamous cell carcinoma of the paranasal sinuses.
Treatment & Prognosis
For nearly all patients, the treatment is surgical resection followed by radiation therapy. Treatment
with this combination of modalities has shown markedly improved results compared to radiation
therapy alone..
Adenocarcinomas & Adenoid Cystic Carcinomas
Adenocarcinomas arise from the mucous gland of epithelial surface of the sinonasal mucosa. there has
been a documented association between woodworkers and these neoplasms, and an increased
prevalence of these tumors in leather workers.
adenoid cystic carcinomas arise from the minor salivary glands. Adenoid cystic carcinomas tend to
arise from the maxillary antrum and can infiltrate into the surrounding tissue. They demonstrate
perineural spread into the maxillary and mandibular branches of the trigeminal nerve (CN V), with
extension into the foramina ovale and rotundum. Adenoid cystic carcinomas have a low incidence of
regional metastases but greater distant metastases.
Treatment
The treatment for both of these tumors consists of multimodality therapy ,surgical resection and
postoperative radiation therapy is frequently employed in treating patients with all of these tumors.
Malignant Mucosal Melanomas
They are exceedingly rare, with only 0.5–1.5% of all melanomas occurring in the sinonasal cavity.
These neoplasms originate from melanocytes within the submucosa and from the mucosa of the
paranasal sinuses. They are located most frequently in the anterior septum, followed by the middle and
inferior turbinates. The maxillary sinus is the most common sinus cavity involved.
Treatment & Prognosis
The treatment consists of surgical excision followed by postoperative radiation therapy. As a result of
this combined treatment approach, the 5-year disease-specific survival rate for sinonasal mucosal
melanomas is approximately 47%.
Sinonasal Undifferentiated Carcinomas
Sinonasal undifferentiated carcinomas are highly aggressive tumors of the paranasal sinuses They
grow rapidly, with extensive local invasion into the sinuses, the orbit, and the brain .Surgical resection
with postoperative radiation therapy is the mainstay of therapy, although this combined approach
results in a very poor prognosis.
Hard palate tumor mass
==
indicating frank invasion into the maxilla

0
CT SCAN; axial section of the nose and paranasal sinus (the neoplasm has invaded the soft tissue
through the anterior bony walls).
