
Tracheostomy
By
Dr Ammar Mohammed Alwan
TUCOM
2019

definition
Tracheotomy >>>means making an opening in the trachea,while
tracheostomy>>>> means converting this opening to a stoma on the
skin surface.
Laryngotomy (Crricothyroidotomy)>>>>means opening the larynx at the
cricothyroid membrane
Percutaneous procedure use guide wire dilator
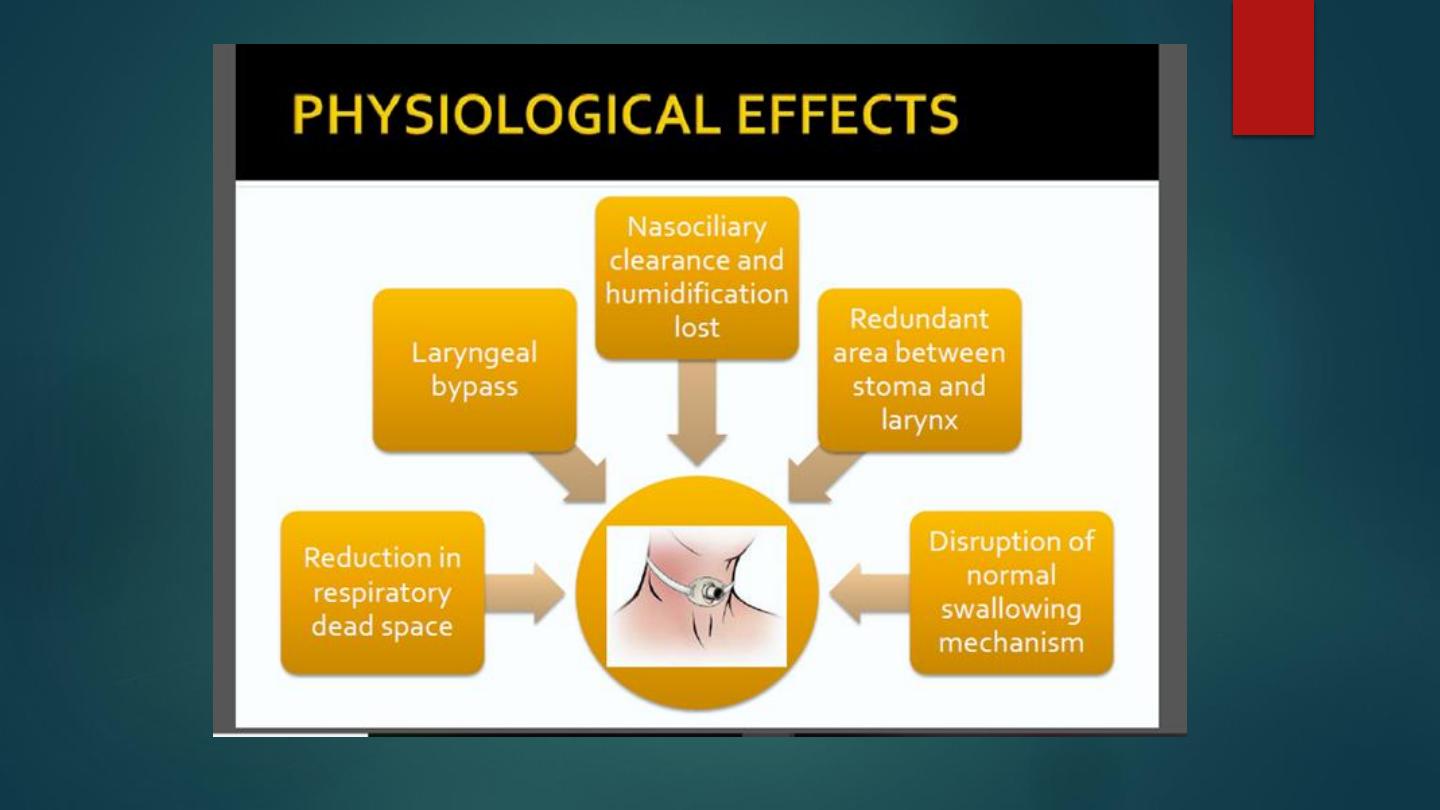

Functions of tracheostomy
1-Relief from upper airway obstruction as it act as bypass.
2-Reduce the airway resistance which in turn reduces the force required to move
the air.
3-Decrease the dead space in the tracheobronchial tree.
4-Enable the patient to swallow without reflex apnea.
5-Helps in better tracheobronchial toilet.
6-Prevent aspiration by cuff.
7-It provide airway for general anesthesia.
8-Prolonged assisted ventilation.

Indications for tracheostomy
A - Upper Airway obstruction.It involve the followings
1-Congenital(subglottic stenosis,laryngeal web,laryngeal
cyst)
2-Trauma(foreign body,head and neck injury,inhalation of
irritant,swallowing of corrosive)
3-Tumors(tongue,larynx,pharynx and thyroid)
4-Infections(acute
epiglottitis,laryngotracheobronchitis,diphtheria,ludwigs
angina)
5-Vocal cord paralysis(postthyroidectomy,bulbar palsy)

A->>>Upper airway obstruction
1. Congenital
Laryngeal web/cysts, B/L choanal atresia,
Tracheoesophageal fistula, Craniofacial anomalies,
Subglottic/tracheal stenosis
2. Infective
Acute epiglottitis, Diphtheria, Acute
layngotracheobronchitis, Ludwig’s angina
3. Trauma
External injury to larynx/trachea, maxillofacial
injury, corrosive injury, inhalational injury
4. Neoplasm
Tumours of larynx, pharynx, tongue, upper
trachea
5. Foreign Body
Foreign body lodged in larynx
6. Vocal cords
B/L abductor paralysis, Bulbar palsy

B ->>>Removal of secretions and protection of
tracheobronchial tree from aspiration
Neurological diseases- GBS, MS, Bulbar palsy
Coma- head injury, poisoning, tumour
In such situations- laryngeal/pharyngeal incompetence
Cuffed tube useful

C->>>Respiratory failure
Tracheostomy- dead space, effort of breathing, alveolar
ventilation
Ease of removal of secretions
Pulmonary diseases- exacerbation of chronic bronchitis,
emphysema, severe pneumonia
Neurological diseases- MS, Motor neuron disease
Severe chest injury- flail chest

D->>> Prolonged ventilation
T-tube more secure than ET tube;
easier to wean off ventilation.
>3wks of intubation
length of ventilation and hospital
stay
E->>>As a part of another procedure
Temporary tracheostomy in head and neck surgeries

The signs of hypoxic patient need urgent
tracheostomy include
1-Increase pulse rate in children >140 beat per minute,in
adult>100 beat per minute.
2-Increase respiratory rate, use of accessory muscle of
resoiration(flaring of alae nasi,recession of suprasternal
notch
3-Restlessness,pallor and facial sweating and hypotension
4-Cyanosis.Indicate late grave sign
5-Blood gases.when Po2<50 or P co2 >70mmhg are bad
signs

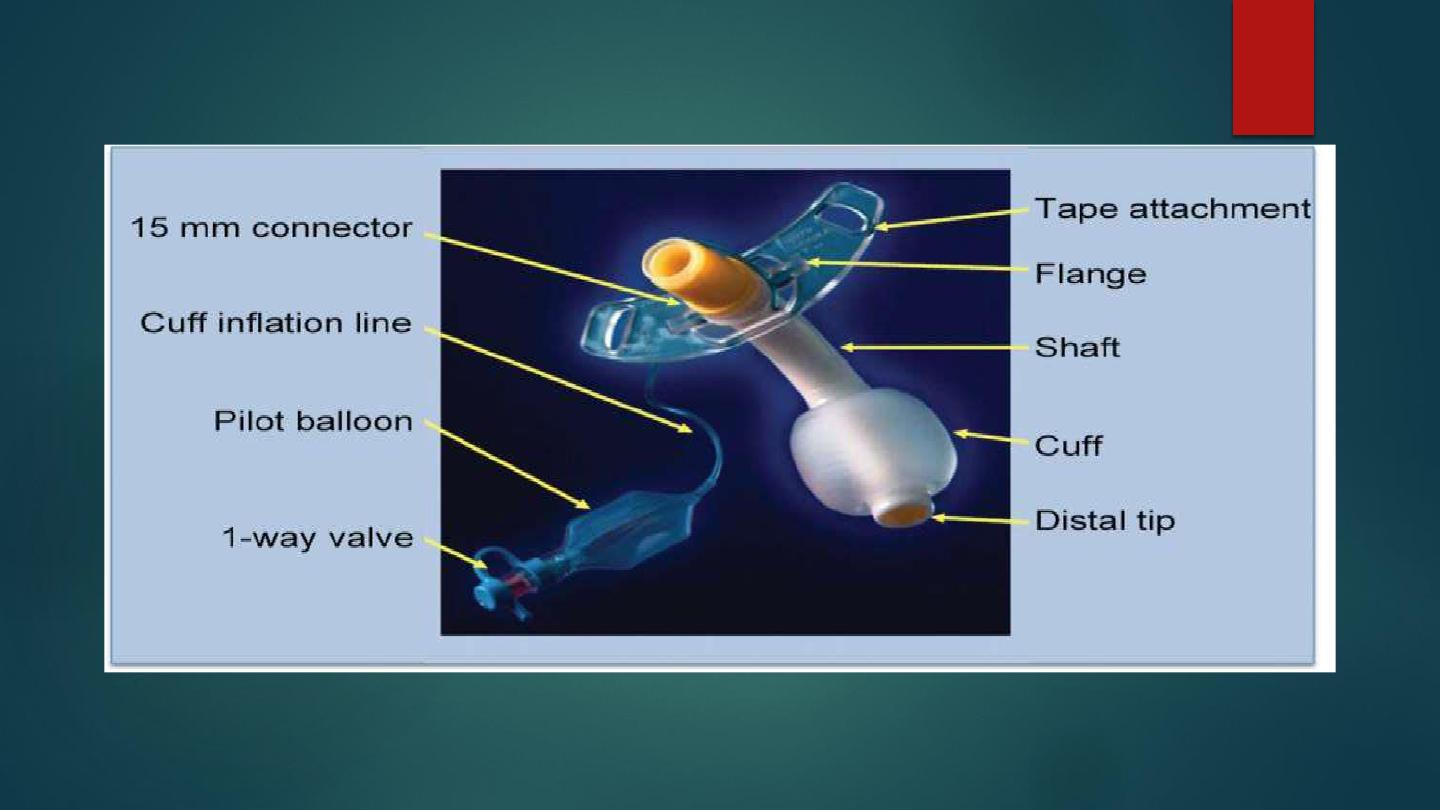
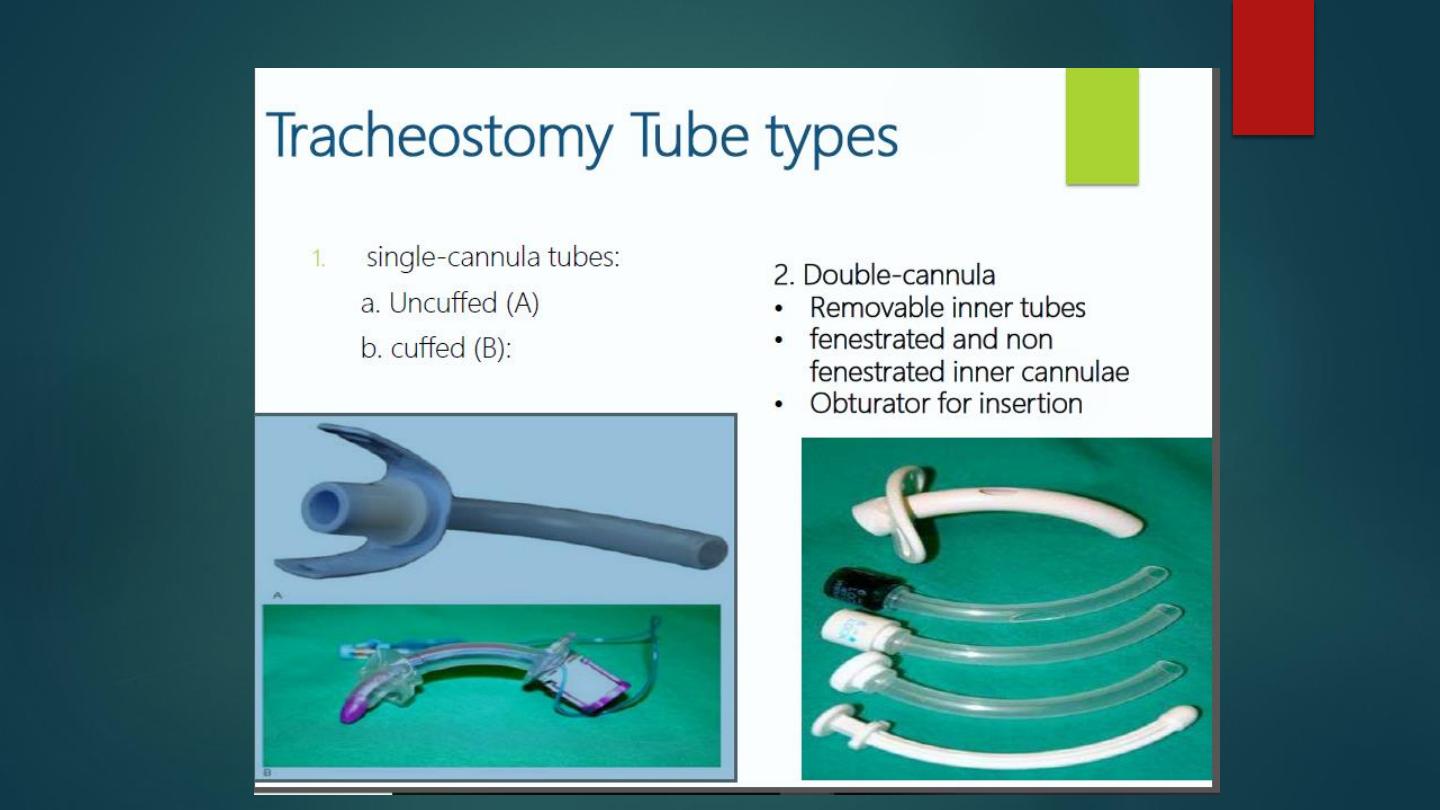
Tracheostomy tubes
The selection of tracheostomy tube depend on the reason for the
procedure and the postoperative requirements.the cuffed tube is
preferred if the patient needs protection of the lower airway from
aspiration or haemorrhage.A fenestrated tube permits the passage
of air upward through the glottis,so allowing the patient to
speak.the removable inner tube facilitate cleaning and removal of
crusted secretion while the outer tube maintains the airway. The
types of tracheostomy tube include the following
1-Metalic.Like Jacksons and Fullers
2-Plastic.
a-Cuffed.
b-Non-Cuffed.
c-Single cannula.
d-Double cannula

Tracheostomy with speaking
valve

postoperative care
1-Tube position and patency should be checked by x-ray.
2-Nursing care .the patient should in upright position , chart for vital signs, give
the patient pens and paper for writing ,give him intravenous fluid especially
in children and depletating patient.
3-Suction. The patient with tracheostomy is unable to cough or clear secretions
so suction should be applied regularly by aseptic technique.
4-Humidification.this procedure is essential to prevent crust formation an
infection,this done by;special humidifier or instillation of normal saline in the
trachea followed by suction
5-Changing the tube.This done after 2-3 days in the adult and after 5-7 days in
children
6-Deflation of the cuff 5minute every hour
7-Swallowing.This aid by defelation of the cuff but sometime the patient needs
nasogastric tube.

Complications
1-Immediate
-Anaesthetic complications
-Apnea or aspiration.
-Bleeding.
-Collapse of the lungs
-Damage to adjacent structures like larynx,esophagus,thyroid,vessels
and recurrent laryngeal nerve
-Embolism-air

2-Intermediate
-Tube obstruction.
-Tube displacement.
-Tracheal erosion.
-Surgical emphysema.
-Wound infection.
-Trachieitis, tracheobronchitis,lung infection
-Bleeding,granulation tissue
-Dysphagia
3-Late.
-Tracheal stenosis
-Subglottic stenosis
-Tracheomalacia.
-Tracheocutenous fistuala
-Traheoasophageal fistuala
-Tracheoarterial or tracheovenous fistula

Other methods of airway management
1-Endotracheal intubation
2-Minitracheostomy\cricothyroidotomy.
The skin and the cricothyroid membrane opened by one cm stab
incision and 4 mm endotracheal tube is passed for ventilation.this is
followed by a regular tracheostomy as infection can occur to the
cricoids cartilage causing subglottic stenosis

3-Percutenous tracheostomy.It is a safe alternative to standard
tracheostomy and is rapid procedure associated with less
bleeding.A one cm skin incision between the first and third tracheal
ring is made followed by dissection of the pretracheal tissues,once
the trachea is reached 14 gauge canula with needle is passed into
the trachea bellow the second tracheal ring.
