Gastrointestinal Diseases
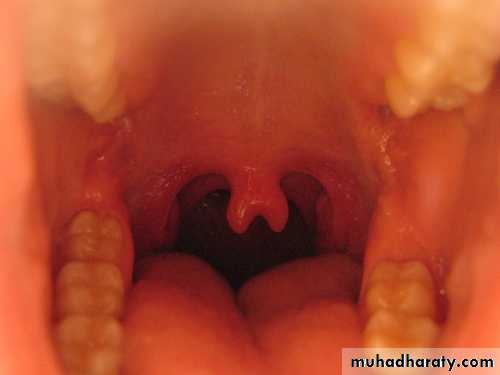
• Normal Digestive Tract Phenomena :short lingual frenulum (tongue-tie)
Surface furrowing of tongue (a geographic or scrotal tongue)bifid uvula
Regurgitation
Tongue tie
Geographical tongue
Bifid uvula
• The number, color, and consistency of stools can vary greatly in the same infant & between infants of similar age without apparent explanation.• Stool frequency is extremely variable in normal infants and can vary from none to 7 per day.
The color of stool has little significance except for the presence of blood or absence of bilirubin products (white-gray rather than yellow-brown).
meconium
Acholic stool
Bloody stool
protuberant abdomen is often noted in infants and toddlersIn the 1st yr of life, it is common to palpate the liver 1-2 cm BCM
A soft spleen tip might also be palpable as a normal finding.Pulsation of the aorta can be appreciated.
Blood loss from GIT is never normalJaundice is common in neonates
• Major Symptoms and Signs of GIT Disorders:
Dysphagia(Difficulty in swallowing )Regurgitation(spitting): effortless movement of stomach contents into esophagus & mouth.
Anorexia: prolonged lack of appetite.
Vomiting:
highly coordinated reflex process that may be preceded by increased salivation and begins with involuntary retching.• Diarrhea :
defined as xs loss of fluid and electrolyte in stool. Acute diarrhea is defined as sudden onset of excessively loose stools of >10 mL/kg/d in infants & >200 g/24 hr in older children & lasts 7 days or less. If lasts 7-13ds ( prolonged), if lasts 14 ds or longer (chronic or persistent diarrhea).Steatorrhea xs fat in stool is a symptom of malabsorption. Disorders that interfere with absorption in the small bowel voluminous diarrhea
Large bowel lower-volume diarrhea.
Dysentery (small-volume, frequent bloody stools + mucus, tenesmus & urgency) predominant symptom of colitis.
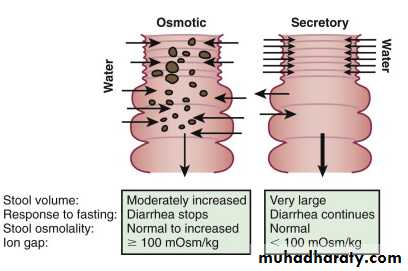
• The pathophysiologic mechanisms for diarrhea are:
• 1.osmotic diarrhea(OD)The ingestion of a poorly absorbable, osmotically active subs & its presence in the bowel lumen create an osmotic gradient that encourages movement of H2O into lumen & subsequently into stool. Electrolyte losses increase because they will follow H2O into lumen through solvent drag .
Two main groups of poorly absorbed solutes exist, the ingestion of which result in OD:
1st normal dietary components that may be malabsorbed ( transiently or permanently). E.g. , disaccharides are usually hydrolyzed to monosaccharides before they are absorbed.
2nd substances that are transported in limited amounts, even by healthy individuals. This includes Mg, PO4, sulfates & lactulose.
The key character of OD is its association with the ingestion of the offending solute. When a pt who has OD is given no oral or enteral feeding, the diarrhea will stop dramatically within 24 hours or less. If the agent is reintroduced, the diarrhea will reappear.
The diarrhea is of a moderate volume compared with that in secretory diarrhea.
An osmotic gap of ˃ 100 mOsm/kg indicates OD.• 2. secretory diarrhea:
• occurs when a physiologic electrolyte secretory process is pathologically stimulated Increase in luminal electrolytes &, subsequently, a secondary increase in water occur.• It is usually of large volume & persists even with fasting. The ion gap is 100 mOsm/kg or less & stool osmolality is normal.
• The prototype for a secretory diarrhea is cholera.
• 3.exudative diarrhea:
A break in the integrity of the mucosal surface of the intestine can result in H2O & electrolyte loss, driven by hydrostatic pressure in bd vessels & lymphatics. The exudate contains mucus, protein & blood cells.e.g:• infectious(Salmonella, Shigella, Yersinia, Campylobacter infection; amebiasis)
• Allergic
• ulcerative colitis.
4.diarrhea resulting from abnormal intestinal motility:
Increased, decreased, or disordered movement of intestine can lead to diarrhea.
e.g. short-bowel syndrome, irritable bowel syndrome.
It denotes infections of GIT caused by bacterial, viral, or parasitic pathogens. Many of these infections are foodborne illnesses. The most common manifestations are diarrhea & vomiting, which can also be associated with abdominal pain & fever. It is common in children, transient & usually self-limited.• USUALLY WITHOUT BLOOD IN STOOL
• Viral enteritis : rotavirus, caliciviruses, enteric adenovirus, astrovirus….• Enterotoxin : Escherichia coli, Klebsiella
• Parasitic : Giardia.
• Extraintestinal infection( parenteral) : otitis media,UTI,pneumonia,meningitis & sepsis.
• Antibiotic-induced and Clostridium difficile toxin (without pseudomembranous colitis)
Causes of Acute Diarrhea
• COMMONLY ASSOCIATED WITH BLOOD IN STOOL
• Bacterial : Shigella, Salmonella, and Campylobacter organisms, Yersinia enterocolitica, invasive E coli,• Cytomegalovirus (especially in immunocompromised individuals)
• Amebic dysentery, Trichuris trichiura (whipworm)
• Hemolytic-uremic syndrome (enterohemorrhagic E coli—E coli O157:H7 and other Shiga toxin-producing E coli)
• Henoch-Schonlein purpura
• Pseudomembranous enterocolitis (C difficile toxin)
• Ulcerative or granulomatous colitis (acute presentation)
• Necrotizing enterocolitis (neonates)
• Risk Factors for Gastroenteritis :
• Environmental contamination
• increased exposure to enteropathogens
• young age
• immunodeficiency
• measles
• malnutrition
• lack of exclusive or predominant breast-feeding
vitamin A deficiency risk of dying from diarrhea, measles, and malaria is increased by 20-24%.
Zinc deficiency risk of mortality from diarrhea, pneumonia, and malaria is increased by 13-21%.
DDx of diarrhea in Infant and Child
Most episodes of acute diarrhea are transient and benign. First one should: assess the hydration status then to know the cause.It is usually the result of viral enteritis, typically occurring with low-grade fv, v & frequent watery stools. Generally, the stools without bd or WBC.
Enterotoxin-producing organisms (eg toxigenic E coli) are associated with watery stools and are without evidence of mucosal invasion (no high fever or bd in stool).
Diarrhea in association with extraintestinal infections, most notably otitis media and pyelonephritis, has been called parenteral diarrhea; its mechanism is obscure
Certain antibiotics, especially ampicillin, have been associated with transient diarrhea. Less common but of greater danger is antibiotic-associated pseudomembranous colitis(PMC) which may occur acutely or as a more chronic illness of 1 or 2 months' duration. C difficile toxin, the cause of most cases of PMC, may also be assoc. with chronic childhood diarrhea in the absence of colitis.
The presence of bd in stool, especially with symptoms of colonic involvement should make the clinician think of infection with :
Campylobacter (Up to 40% of individuals who have Guillain-Barre syndrome have evidence of a Campylobacter infection occurring before the onset of neurologic symptoms).
Shigella (Patients who have Shigella organisms tend to appear severely ill and may have meningismus or seizures. The stools tend to be foul smelling).
Salmonella organisms
C. difficile toxin-associated pseudomembranous colitis.Yersinia enterocolitis .
E coli can produce diarrhea by several pathogenic mechanisms; the enteroadherent, enteroinvasive, enterohemorrhagic, and enteroaggregative .Amebiasis ( Entamoeba histolytica) can produce a picture of acute colitis.
Non infectious causes of bloody diarrhea:intussusception
immune deficienciesChronic inflammatory bowel disease (IBD)
Food-borne spread of organisms or toxins is an important cause of acute diarrheal illness.
• Clinical Evaluation of Diarrhea :
• HISTORY
• 1. Length of illness
• 2. Character of stools: frequency, looseness (watery vs mushy)& presence of gross blood
• 3. Oral intake: diet, quantity of fluids & solids taken
• 4. Presence of vomiting
• 5. Associated symptoms: fever, rash & arthralgia
• 6. Urine output: frequency and qualitative amount
• 7. Possible exposure to diarrheal illness, child-care center attendance
• PHYSICAL EXAMINATION
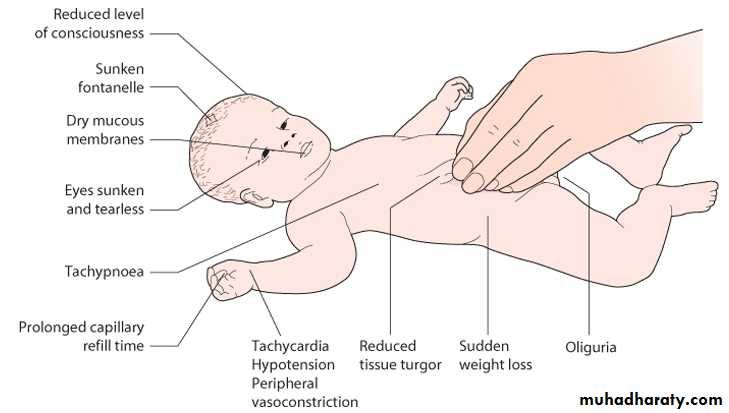
• 1. Hydration status: weight (stable or loss), mucosa (moist or dry), saliva & tears (present or absent), skin turgor (normal or poor), eyeballs & fontanelle (normal or sunken), & vital signs
• 2. Alertness
• 3. Infant: vigor of suck
Assessment of Degree of Dehydration:
Mild
ModerateSevere
wt loss %
‹ 5%
5-10%
› 10%
ml/kg fluid loss
‹ 50
50-100› 100
Infants and young children
Thirsty; alert; restless
Thirsty; restless or lethargic but irritable or drowsyDrowsy; limp, cold, sweaty, cyanotic extremities; may be comatose
Older children
Thirsty; alert; restless
Thirsty; alert (usually)Usually conscious (but at reduced level), apprehensive; cold, sweaty, cyanotic extremities; wrinkled skin on fingers and toes; muscle cramps
Signs and Symptoms
Heart rate
normal
tachycardiaTachycardia,with bradycardia in most severe cases
Palpable pulses
Present
Present (weak)Decreased
Blood pressure
Normal
Orthostatic hypotensionHypotension
Capillary refill
Normal(up to 2 sec)
prolonged
Prolonged,minimal
Skin turgor(skinfold)
Instant recoil
Recoil in < 2 secRecoil >2 sec
Fontanel
Normal
Slightly depressedSunken
Mucous membrane
Moist
DryVery dry
Tears
Present
Present or absent
Absent
Respirations
Normal
Deep, may be rapidDeep and rapid
Urine output
Normal
OliguriaAnuria and severe oliguria
• Being lethargic and sleepy are not the same. A lethargic child is not simply asleep; the child’s mental state is dull and the child cannot be fully awakened; the child may appear to be drifting into unconsciousness.
• In some infants and children, the eyes normally appear somewhat sunken. It is helpful to ask the mother if the child’s eyes are normal or more sunken than usual.
• Dryness of the mouth and tongue can also be palpated with a clean finger. The mouth may be dry in a child who habitually breaths through the mouth. The mouth may be wet in a dehydrated child with recent vomiting or drinking.
• A The skin pinch is less useful in infants and children with marasmus (severe wasting) or Kwashiorkor (severe malnutrition with edema), or obese children
• LABORATORY (PERFORMED AS INDICATED)
• Stool exam: culture, ova and parasites, smear for WBC, C. difficile toxin assay, occult bd & reducing substances.The finding of >5neutrophil/hpf or +ve lactoferrin assay in infant not breastfeeding suggests classical bacterial enteropathogens• 2. CBC: Hemoconcentration ↑ Hb & PCV
• blood urea nitrogen (BUN),serum creatinine & electrolytes
• 4. GUE:the urine SG is usually ↑ (≥1.025) in significant dehyd, but ↓ after rehyd.
• With dehydration, GUE may show hyaline and granular casts, a few WBC & RBC, and 30 to 100 mg/dL of proteinuria
• 5. If child is lethargic or has seizure, culture for sepsis: measure BUN, S. electrolyte, glucose & CSF.
Calculation for correction of dehydration
1.Deficit:A child with dehydration has lost water; there is usually a concurrent loss of Na+ and K+
• Water deficit =%dehydration× weight
• Sodium deficit = Water deficit × 80 mEq/L
• Potassium deficit = Water deficit × 30 mEq/L
e.g. for a 10-kg child with severe dehydration:
deficit of water= 10/100×10=1 liter
2.Maintenace fluid(water):
BODY WEIGHT
FLUID PER DAY
0-10 kg
100 mL/kg
11-20 kg
1,000 mL + 50 mL/kg for each kg >10 kg
>20 kg
1,500 mL + 20 mL/kg for each kg >20 kg♯
♯The maximum total fluid per day is normally 2,400 ml
3.Ongoing losses :
From diarrhea or vomiting or urine or skin & lungs should be replaced ml/ml• Sources of Water losses:
• Urine 60%
• Insensible losses (skin and lungs)35%
• Stool 5%
• Maintenance requirements of electrolytes:
• Sodium: 2 - 3 mEq/kg/day
• Potassium: 1 - 2 mEq/kg/day.
4.Select an appropriate fluid (based on total water and electrolyte needs).
For a pt with isotonic dehydration, D5 half NS with 20 mEq/L KCl) usually an appropriate fluid.
K+ usually is not included in the IV fluids until the pt voids, unless significant hypok+ is present.
5.Replace ongoing losses as they occur.
• In all children, it is critical to carefully monitor vital signs, wt, UOP, and electrolytes to identify over- or underhydration, hypona, & other electrolyte disturbances, then adjust the rate or composition of the IV solution accordingly.
• In a child with a known or probable metabolic alkalosis(e.g., child with isolated vomiting), LR should not be used because the lactate or acetate would worsen the alkalosis.
Fluid Management Of Dehydration:
Restore intravascular volume( fluid bolus or shoot):NS or Ringer's lactate : 20 mL/kg over 20 min (repeat as needed)
Calculate 24-hr fluid needs: maintenance+deficit
Subtract isotonic fluid already administerd from 24-hrs fluid needs
Administer remaining volume over 24 hr using D5 ½ NS + 20 mEq/L KCl
Replace ongoing losses as they occur
How to calculate rate of IV infusion to deliver a desired amount of fluid at a definite time period?
Rate (drop/minute) of infusion of IV fluid to be infused in 24 hours is equivalent to fluid volume to be infused in terms of mL in hundred. For example, if 500 mL (5 × 100) of fluid has to be infused over 24 hours then the rate of infusion is 5 drops/ minute.
If microdrop is used via microburette, the rate will be 20 drops/minute in microburette (one drop in normal burette = four drops in microburette).
15 drops in normal burette or 60 drops in microburette are equivalent to 1 mL.
• solution
• Glucose (g/l)• Na+
• K+
• Ca+2
• Cl-
• Lactate
• D5W
• 50
• 0
• 0
• 0
• 0
• 0
• D10w
• 100
• 0
• 0
• 0
• 0
• 0
• NS
• 0
• 154
• 0
• 0
• 154
• 0
• ½ NS
• 0
• 77
• 0
• 0
• 77
• 0
• ¼ NS
• 0
• 38.5
• 0
• 0
• 38.5
• 0
• D5NS
• 50
• 154
• 0
• 0
• 154
• 0
• D5 ½ NS
• 50
• 77
• 0
• 0
• 77
• 0
• 0.2 NS
• 0
• 31
• 0
• 0
• 31
• 0
• 3%NaCl
• 0
• 513
• 0
• 0
• 513
• 0
• LR
• 0
• 130
• 4
• 3
• 109
• 28