Rickets
Dr.Noor Sameer Yahya9/10/2019
Cow milk and soy protein intolerance (allergic colitis)
Symptoms can appear from 1 to 2 weeks of age to 12 months.Most infants appear healthy despite the presence of streaks of bloody mucus in their stools.
intestinal protein loss produces edema and a protein-losing enteropathy.
Diarrhoea and/or vomiting with failure to thrive
Acute colitis
Iron-deficiency anemia (secondary to GI blood loss)
Eczema
Occasionally, an acute anaphylactic reaction with urticaria, stridor, bronchospasm and shock.
Although no single laboratory test is diagnostic, affected children may have:
EosinophiliaA high IgE concentration in plasma.
Those children who present with failure to thrive and protracted diarrhoea may require a jejunal biopsy to establish the diagnosis, there is a patchy enteropathy usually with prominent eosinophils in the lamina propria.
Most children are diagnosed clinically and treated empirically .Elimination of the offending antigen results in rapid resolution of symptoms and this, together with their return upon challenge, is the only diagnostic test.
For children with persistent symptoms or other concerns, the diagnosis can be confirmed safely and easily by rectal mucosal biopsy; this shows eosinophilic inflammation of the mucosa. Visual findings at proctoscopy usually include mucosal friability and lymphoid hyperplasia, giving a lumpy, "mosquito-bitten" appearance to the rectal mucosa
Treatment:
At least 30% of infants with cow's milk allergy also demonstrate sensitivity to soy protein.
Infants who are bottle-fed should be switched to a hydrolyzed protein formula (e.g., Nutramigen, Pregestamil).
Less than 5% have persistent symptoms and these cases resolve with the use of amino acid–based formulas.
Breast fed infants may continue breast feeding, but the mother should restrict soy and dairy products from her diet.
Visible blood in the stools typically resolves within a few days, although occult blood persists for several weeks.
Rickets, a disease of growing bone, occurs in children only before fusion of the epiphyses, and is due to unmineralized matrix at the growth plates
Etiology
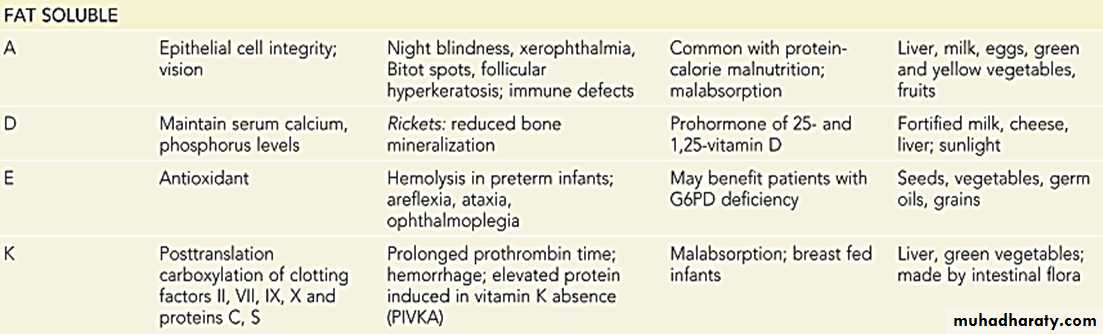
• 1.VITAMIN D DISORDERSNutritional vitamin D deficiency
Secondary vitamin D deficiency
1. Malabsorption
2. Increased degradation
3. Decreased liver 25-hydroxylase
Vitamin D-dependent rickets type 1
Vitamin D-dependent rickets type 2
Chronic renal failure
• 2.CALCIUM DEFICIENCY
Low intake : Diet , Premature infants
Malabsorption :
• 3.PHOSPHORUS DEFICIENCY
Inadequate intake
Premature infants (rickets of prematurity)
Aluminum-containing antacids
• 4.RENAL LOSSES
X-linked hypophosphatemic rickets*
Autosomal dominant hypophosphatemic rickets*
Hereditary hypophosphatemic rickets with hypercalciuria
Fanconi syndrome
• 5.DISTAL RENAL TUBULAR ACIDOSIS
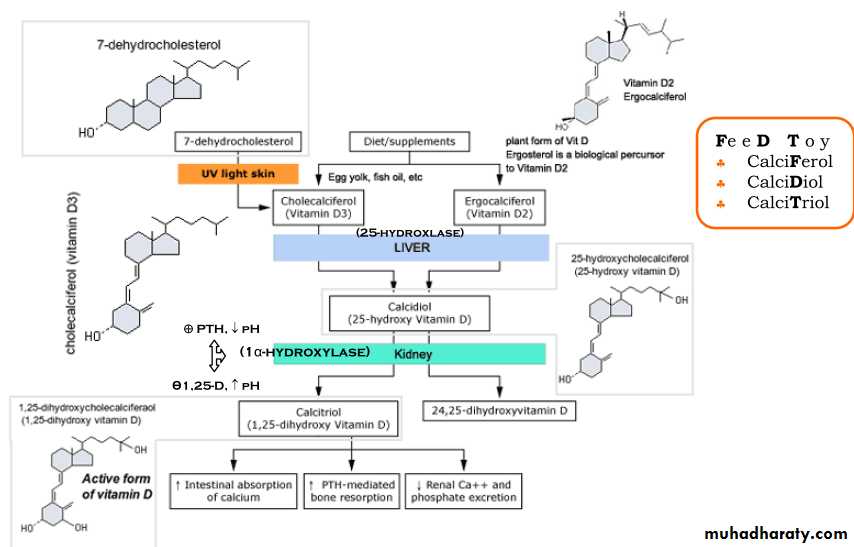
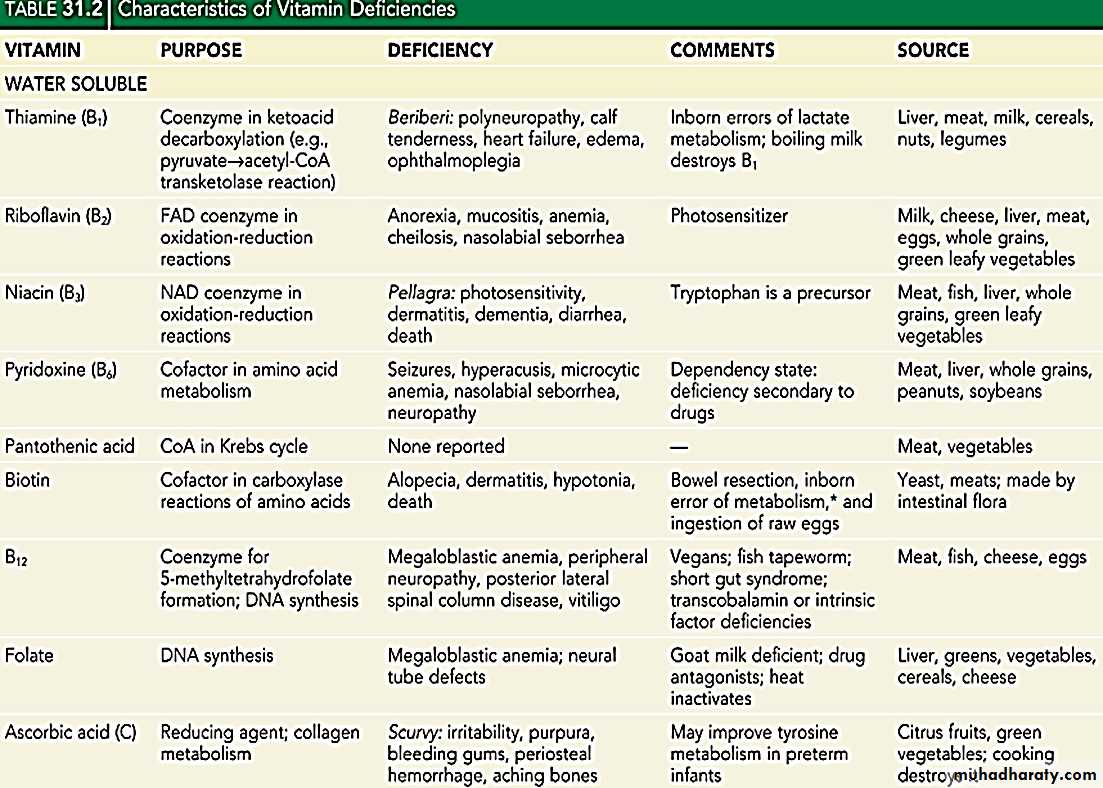
VITAMIN D DISORDERS Vitamin D can be synthesized in skin epithelial cells and therefore technically is not a vitamin. 7-dehydrochlesterol converted to vitamin D 3 (3-cholecalciferol) by effect of Ultraviolet B radiation
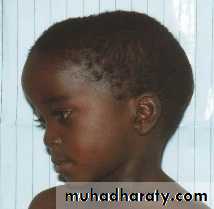
The efficiency of this process is ↓ by melanin so more sun exposure is necessary for vitamin D synthesis in people with increased skin pigmentation.
• Covering the skin with clothing or applying sunscreen lead to↓ vitamin D synthesis
• • Supplemental vitamin D may be vitamin D 2 (plants or yeast) or vitamin D 3(Fish liver oils have a high vitamin D content. Also, fatty fish and egg yolks) ; they are biologically equivalent.
• Breast milk has a low vitamin D content, approximately 12-60 IU/L.
.
Both vitamin D2 and vitamin D3 are hydroxylated in the liver to 25-hydroxyvitamin D (calcidiol), which is further hydroxylated in the kidney to 1,25-dihydroxyvitamin D (calcitriol),, which acts as a hormone and the most biologically active form of the vitamin
• measurement of 25-D is the standard method for patient's vitamin D status
\
FUNCTION:
Marked ↑ calcium absorption, which is highly dependent on 1,25-D.↑ Phosphorus absorption, less significant because most dietary phosphorus absorption is vitamin D-independent.
1-,25 D also has direct effects on bone, including mediating resorption.
1-,25 D directly suppresses PTH secretion by the parathyroid gland also suppressed by the increase in serum calcium
Clinical Evaluation
majority of children with rickets have a nutritional deficiency, initial evaluation is dietary history ( intake of vitamin D and calcium)
Cutaneous synthesis mediated by sunlight exposure is an important source of vitamin D. Children with ↑ skin pigmentation has ↓cutaneous synthesis& ↑ vitamin D deficiency
The presence of maternal risk factors for nutritional vitamin D deficiency is an important consideration when a neonate or young infant has rachitic findings
The child's medication use is relevant because :
anticonvulsants phenobarbital and phenytoin, increase degradation of vitamin D
aluminum-containing antacids interfere with the absorption of phosphate.
the antituberculosis medications isoniazid and rifampin inducing the P450 system which ↑ the degradation of vitamin D
5) Malabsorption of vitamin D : history of liver or intestinal disease. ,rickets may be the presenting complaint. .
• 6) renal disease (proteinuria, hematuria, urinary tract infections) is an additional significant consideration, given the importance of chronic renal failure as a cause of rickets.
• 7) Children with rickets may have a history of dental caries, poor growth, delayed walking, waddling gait, pneumonia, and hypocalcemic symptoms.
• 8) The family history, large number of genetic causes of rickets, most is rare. inquire about leg deformities, difficulties with walking, or unexplained short stature
• 9) A history of a unexplained sibling death during infancy may be present in the child with cystinosis is the most common cause of Fanconi syndrome in children
Clinical Manifestations
GENERAL: Failure to thrive ,Listlessness ,Protruding abdomen ,Muscle weakness (proximal) ,FracturesHEAD :Craniotabes( softening of the cranial bone detected by applying pressure at the occiput or over the parietal bone similar to the feel of pressing into a Ping-Pong ball and then releasing, Caput quadratum). Boxlike), Frontal bossing ,Delayed fontanelle closure ,Delayed dentition; caries ,Craniosynostosis
CHEST :Rachitic rosary ,Harrison groove , pigeon chest deformity ,Respiratory infections & atelectasis*
BACK :Scoliosis, Kyphosis ,Lordosis
EXTREMITIES :Enlargement of wrists and ankles ,Valgus or varus deformiti]es ,Windswept deformity (combination of valgus deformity of 1 leg with varus deformity of the other leg) , Anterior bowing of the tibia and femur ,Coxa vara: angle between femur shaft and ball is <120, Leg painHYPOCALCEMIC SYMPTOMS :Tetany ,Seizures ,Stridor due to laryngeal
• spasm
The initial laboratory tests in a child with rickets should include:
Laboratory investigationsThe serum calcium usually is normal but may be low,
The serum phosphorus level usually is reduced, due to PTH-induced renal losses of phosphate, combined with a decrease in intestinal absorption
The serum alkaline phosphatase activity is elevated.
When serum calcium levels decline to less than 7.5 mg/dL, tetany may occur
• The level of 1,25-D is only low when there is severe vitamin D deficiency
25-D level is low
glycosuria and aminoaciduria (positive dipstick for protein) : Fanconi syndrome
urinary excretion of calcium (24 hr collection for calcium or calcium-creatinine ratio) : hereditary hypophosphatemic rickets with hypercalciuria or Fanconi syndrome)
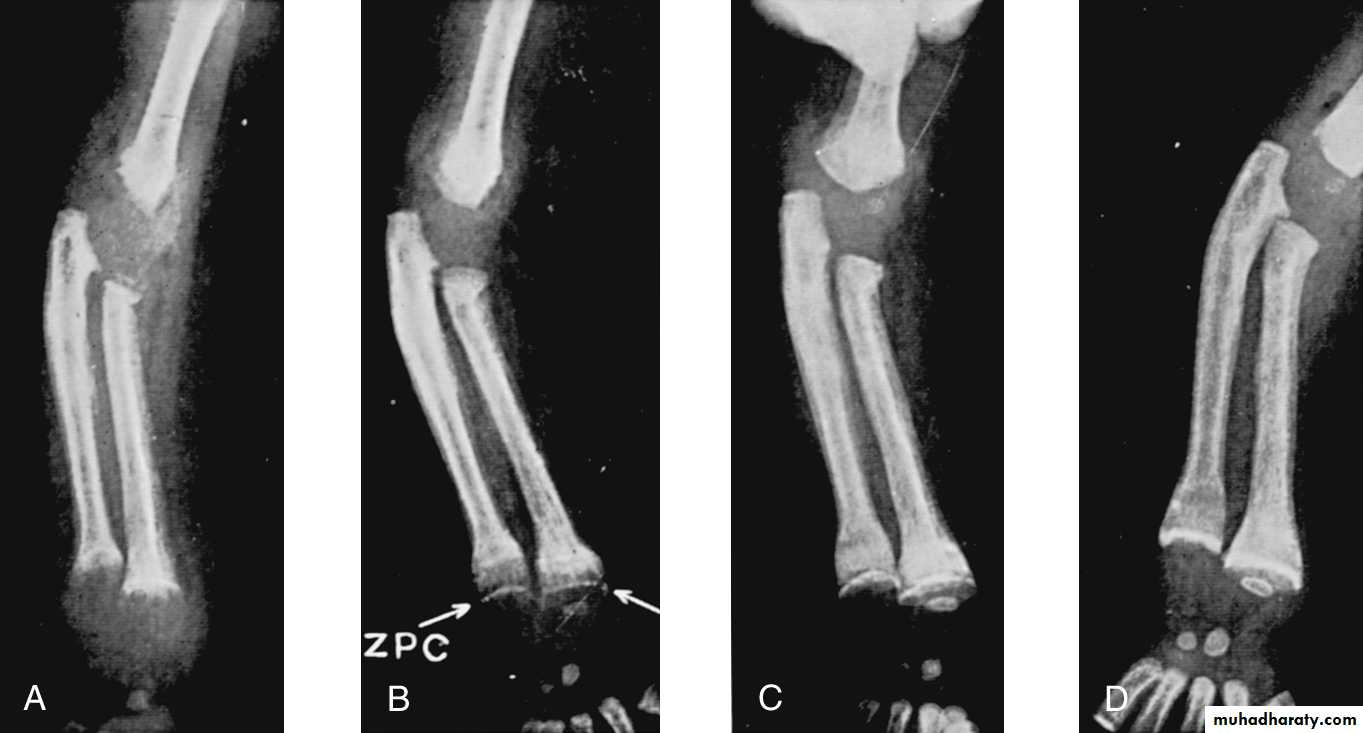
Rachitic changes are most easily visualized on posteroanterior radiographs of the wrist,
Decreased calcificationthickening of the growth plate.
fraying: The edge of the metaphysis loses its sharp border.
cupping: the edge of the metaphysis changes from a convex or flat surface to a more concave surface. most easily seen at distal ends of the radius, ulna, fibula.
widening of the distal end of the metaphysis, corresponding to the clinical observation of thickened wrists and ankles, as well as the rachitic rosary.
Coarse trabeculation of the diaphysis and generalized rarefaction.
Most cases of rickets are diagnosed based on the classic radiographic abnormalities
Treatment :
vitamin D and adequate nutritional intake of calcium and phosphorus. There are 2 strategies for administration of vitamin D:stoss therapy, 300,000-600,000 IU of vitamin D are administered orally or intramuscularly as 2-4 doses over 1 day then daily vitamin D intake of 400 IU/day
daily, high-dose vitamin D, 2,000-5,000 IU/day over 4-6 wk then daily vitamin D intake of 400 IU/day
Healing Rickets: Calcification takes place in the zone of preparatory calcification
Prevention:
Direct sun exposureVitamin D The American Academy of Pediatrics recommends vitamin D supplementation of
All breastfed infants in the amount of 400 IU/day, started soon after birth and given until the infant is taking more than 1000 mL/day of vitamin D-fortified milk (for age >1 year).
Older children should receive 600 IU/day
VITAMIN D-DEPENDENT RICKETS, TYPE 1
• autosomal recessive disorder, have mutations in the gene encoding renal 1α-hydroxylase, preventing conversion of 25-D into 1,25-D.• They have normal levels of 25-D, but low levels of 1,25-D
• Long-term treatment with 1,25-D (calcitriol(.
• excessive dosing of calcitriol lead to hypercalciuria and nephrocalcinosisurinary calcium excretion( target of <4 mg/kg/day)
VITAMIN D-DEPENDENT RICKETS, TYPE 2
• autosomal recessive disorder of the vitamin D receptor, preventing a normal physiologic response to 1,25-D. So Levels of 1,25-D are extremely elevated
•50-70% of children have alopecia.
• Epidermal cysts are a less common manifestation.
• Treatment: extremely high doses of vitamin D 2 , 25-D, or 1,25-D. ,Patients who do not respond need long-term intravenous calcium