Treatment of abnormal uterine bleeding
Treatment of abnormal bleeding requires an accurate diagnosis. A definitive diagnosis is required before instituting long-term treatment, and should be made on the basis of hysteroscopy, sonohysterography, or directed endometrial biopsies, if indicated.Polyp
Endocervical polyps can be avulsed in the outpatient setting. Endometrial polyps can be removed blindly under general anaesthetic, or by hysteroscopic resection either under general anaesthetic or in the outpatient setting.Adenomyosis, malignancy are treated accordingly.
Leiomyoma :Myomectomy (abdominal, laparoscopic or hysteroscopic) is the surgical removal of fibroids from the uterine wall with conservation of the uterus. If the fibroid protrudes into the uterine cavity, it may be removed hysteroscopically.
GnRH analogues, and more recently SPRMs, are often used for up to 3 months prior to surgical intervention in an attempt to reduce the size and vascularity of the fibroids.
Immediate complications of myomectomy usually relate to excessive blood loss and a blood transfusion may be required intraoperatively or postoperatively. Patients should therefore be carefully counselled preoperatively about this risk, including hysterectomy. Intermediate postoperative risks include infection and further bleeding.
Uterine artery embolization is an alternative option in fibroid.
Coagulopathy
In adolescents ruling out coagulation disorders is important and if this is the case hematological management is offered accordingly.
Ovulatory disfunction
In adolescents after ruling out coagulation disorders, the main direction of therapy is to temporize because with time and maturity of the HPO axis, the problem will be corrected. A cyclic progestogen for example, medroxyprogesterone acetate, 10 mg for 10 days each month for a few months is all that is needed to produce reliable and controlled menstrual cycles. This may be continued for up to 6 months. If the problem persists beyond 6 months, OCs become an option in that the condition may be more chronic.In the perimenopausal woman who has dysregulation of the HPO axis, there is much variability and unpredictability of cycles because the HPO axis is in flux, moving toward ovarian failure. Although most of the bleeding in this setting is caused by anovulation, occasional ovulation can occur, with or without a normal luteal phase, which is highly variable and erratic. Here, it is more efficient to use a low-dose (20-μg) OC in a nonsmoking woman. Progestogens used cyclically, although preventing endometrial tissue from building up because of anovulation, will help the endometrium but will not reliably control bleeding, because of the unpredictability of the hormonal situation.
During reproductive life, chronic anovulatory bleeding is primarily caused by hypothalamic dysfunction or PCOS. OCs work well in this setting, although an alternative is cyclic progestogens, as noted previously. Some of these women may also wish to conceive, in which case ovulation induction is indicated.
Iatrogenic : stop or manipulate the cause (medication)
HMB :
For women with heavy menstrual bleeding, for whom there is no known cause and anatomic lesions have been ruled out, the aim of therapy is to reduce the amount of excessive bleeding. As noted, some women have abnormal prostaglandin production and some have alterations of endometrial blood flow.Medical treatment :
Nonsteroidal Anti-Inflammatory DrugsNSAIDs are prostaglandin synthetase inhibitors that inhibit the biosynthesis of the cyclic endoperoxides, which convert arachidonic acid to prostaglandins. In addition, these agents block the action of prostaglandins by interfering directly at their receptor sites. Several NSAIDs have been administered during menses to groups of women with menorrhagia and ovulatory DUB and have been found to reduce the mean MBL by approximately 20% to 50%.
Drugs used included:
mefenamic acid (500 mg, three times daily)
ibuprofen (400 mg, three times daily)
naproxen sodium (275 mg, every 6 hours after a loading dose of 550 mg)
These drugs are usually given for the first 3 days of menses or throughout the bleeding episode. All appear to have similar levels of effectiveness.
Antifibrinolytic Agents
ε-Aminocaproic acid (EACA), tranexamic acid (AMCA), and para-aminomethyl benzoic acid (PAMBA) are potent inhibitors of fibrinolysis and have therefore been used in the treatment of various hemorrhagic conditions. They clearly produce a reduction in blood loss and may be used as therapy for women with menorrhagia who ovulate. The side effects of this class of drugs, are nausea, dizziness, diarrhea, headaches, abdominal pain, and allergic manifestations. Renal failure, pregnancy, and history of thrombosis are contraindications to the use of antifibrinolytic agents.Combined oral contraceptive pill
COCPs is generally considered to be effective in the management of HMB. It reduces bleeding by around 50% and has the additional benefit of reducing dysmenorrhea. Furthermore, as amenorrhoea has become more acceptable (and indeed for some women even desirable), many women use the COCP continuously for periods of 3–6 months to avoid menstruation altogether. Risks of COCP treatment include breast cancer, thromboembolic and cardiovascular disease and migraine (increased in the older woman, particularly if she is a smoker)Oral progestogens
Oral progestogens are helpful in the management of women with irregular (anovulatory) HMB, particularly common at the extremes of reproductive life. Cyclical administration of progestogens for less than 21 days each cycle in ovulatory women is of no benefit. Only norethisterone acetate (5 mg three times daily), if prescribed cyclically for 21 days, is effective treatment for ovulatory HMB. Shorter courses of oral progestogens (14 days) are appropriate for women with definite anovulatory cycles (e.g. PCOS) and at risk of endometrial hyperplasia.
The levonorgestrel-releasing intrauterine system (LNG-IUS)
has an effective duration of action of more than 5 years. At the end of 3 months, it caused an average 80% reduction in MBL, which increased to 100% at the end of 1 year. This reduction in MBL was significantly greater than that achieved with an antifibrinolytic agent or a prostaglandin synthetase inhibitors. It is also effective in increasing hemoglobin levels, decreasing dysmenorrhea, and reducing blood loss caused by fibroids and adenomyosis.Patients with AUB due to coagulopathy, especially secondary to anticoagulation therapy, also can be managed successfully with the LNG-IUS. Similar results have been demonstrated in patients with von Willebrand disease.
Gonadotropin-Releasing Hormone Agonists
GnRH agonists (goserelin) may be used to inhibit ovarian steroid production, as estrogen production is necessary for endometrial proliferation. daily administration of a GnRH agonist for 3 months markedly reduced MBL to 30 mL or less per cycle. Because of the expense and side effects of these agents, their use for heavy menstrual bleeding is limited to women with severe MBL who fail to respond to other methods of medical management and wish to retain their childbearing capacity. More commonly, GnRH agonists are an effective means of bridging patients to surgical treatment, allowing for correction of anemia. Use of an estrogen or progestogen (add-back therapy) together with the agonist will help prevent bone loss.Surgical treatment :
Surgical treatment is normally restricted to women for whom medical treatments have failed or where there are associated symptoms such as pressure symptoms from fibroids or prolapse.Women contemplating surgical treatment for HMB must be certain that their family is complete. While this caveat is obvious for women contemplating hysterectomy, in which the uterus will be removed, it also applies to women contemplating endometrial ablation. Therefore, women wishing to preserve their fertility for future attempts at childbearing should be advised to use medical methods of treatment. The risks of a pregnancy after an ablation procedure theoretically include prematurity and morbidly adherent placenta.
Endometrial ablation
All endometrial destructive procedures employ the principle that ablation of the endometrial lining of the uterus to sufficient depth prevents regeneration of the endometrium.
Ablation is suitable for women with a uterus no bigger than 10 weeks’ size and with fibroids less than 3 cm.
The first-generation techniques including transcervical resection of the endometrium with electrical diathermy or rollerball ablation have largely been replaced by newer second-generation techniques including:
• Impedance controlled endometrial ablation (Novosure™).
• Thermal uterine balloon therapy.
• Microwave ablation (Microsulis™)
As a general rule, all women undergoing endometrial ablation should have access to a secondgeneration technique. After treatment, 40% will become amenorrhoeic, 40% will have markedly reduced menstrual loss and 20% will have no difference in their bleeding. Some authorities have suggested that endometrial ablation is so successful that all women with HMB should be encouraged to consider it before opting for hysterectomy. While there are merits to this argument, some women, after informed discussion, will still prefer hysterectomy and they should therefore be considered for this procedure instead.
All can be performed as day‐case procedures, either under general anaesthetic (with analgesia) or under local anaesthetic in the outpatient setting. Postoperatively, patients may complain of transient crampy abdominal pain and a watery brown discharge for 3–4 weeks. Prophylactic antibiotic therapy is often used to reduce the risk of endometritis.
Patients must be counselled before the procedure about complications, which may include device failures at the time of the procedure, endometritis, haematometra, fluid overload due to absorption of distension medium (resection only), perforation and intra‐abdominal injury (including visceral burns).
Uterine artery embolization
Uterine artery embolization (UAE) is a well‐established technique for treatment of fibroids.The procedure is usually carried out by an interventional radiologist, usually under local anaesthetic with or without sedation. The femoral artery is canalized on one or both sides and fed into the iliac and then uterine artery. Angiography is carried out to confirm the correct position before introduction of the embolic agent. Blockage of both uterine arteries results in fibroids becoming avascular and shrinking. Because the normal myometrium subsequently derives its blood supply from the vaginal and ovarian vasculature, UAE is thought to have no permanent effect on the remainder of the uterus. The procedure requires only a short hospital stay and may be carried out as a day case in selected women. After UAE, a mean reduction in fibroid volume of 30–46% has been reported and symptomatic improvement has been reported in up to 85% of women. In the immediate postoperative period, patients may experience ischaemic pain (usually responsive to simple analgesics) and infection is not uncommon. Occasionally, following UAE the rapid change in uterine size can result in passage of the fibroid vaginally. there is a theoretical risk of premature ovarian failure after UAE.
Hysterectomy
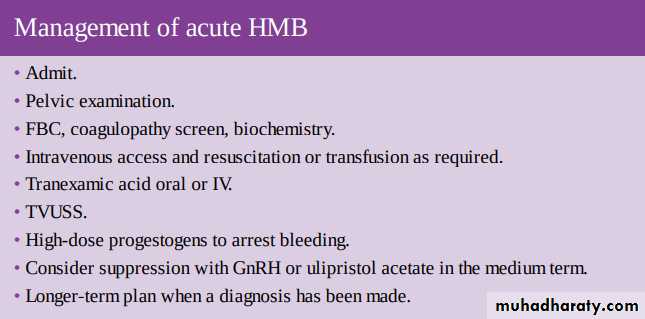
A total hysterectomy is the only guaranteed ‘no bleed’ option for HMB. However, hysterectomy should only be considered in the treatment of HMB when a woman has completed her family and when medical and less invasive surgical options have been offered, failed or are inappropriate. Hysterectomy is an established and effective treatment for HMB that induces amenorrhoea, but this must be balanced against the potential morbidity associated with the procedure and the very low risk of mortality. In young patients with HMB, the ovaries are usually conserved but a bilateral salpingectomy should be carried out simultaneously due to recent evidence suggesting that ovarian cancer may have its origins within the fallopian tube. Those younger women who wish to have their ovaries removed, either by choice or due to family history of ovarian or breast cancer, must be appropriately assessed and counselled about the need for hormone replacement until the age of normal menopause. The routes for hysterectomy include laparoscopic, abdominal and vaginal. Individual patient characteristics and surgical expertise are important determinants of the chosen approach.Severe acute heavy menstrual bleeding
Not infrequently women are admitted to hospital with AUB. They require stabilization, examination to exclude cervical abnormalities and pelvic masses, medication to arrest bleeding and correct anaemia, investigation and discharge with a long-term plan to avoid further admissions. In women who are bleeding heavily and are hemodynamically unstable, the quickest way to stop acute bleeding is with curettage. This should also be the preferred approach for older women and those with medical risk factors for whom high-dose hormonal therapy may pose a great risk.Surgical Therapy:
Dilation and CurettageThe performance of a D&C can be diagnostic and is therapeutic for the immediate management of severe bleeding. For women with markedly excessive uterine bleeding who may be hypovolemic, a D&C is the quickest way to stop acute bleeding. Therefore it is the treatment of choice in women who suffer from hypovolemia. A D&C may be preferred as an approach to stop an acute bleeding episode in women older than 35 when the incidence of pathologic findings increases
Hysterectomy
The decision to remove the uterus should be made on an individual basis and should usually be reserved for the woman with other indications for hysterectomy, such as leiomyoma or uterine prolapse. Hysterectomy should only be used to treat persistent abnormal uterine bleeding after all medical therapy has failed, medical therapy is contraindicated, and the amount of MBL has been documented to be excessive by direct measurement.