polycystic ovary syndrome (PCOS)
Dr Hiba Ahmed SuhailM.B. Ch. B./F.I.B.O.G.College of medicineUniversity of Mosulpolycystic ovary syndrome (PCOS)
First defined in 1935, Stein and Leventhal described condition of obesity ,amenorrhea or oligomenorrhea , bilateral polycystic ovaries.Many decade pass and it now known as polycystic ovary syndrome (PCOS)
Incidence
PCOS is the most common endocrine abnormality of reproductive-aged women. The prevalence of PCOS is between 4% -10% of reproductive-aged women.Definition of PCOS
Rotterdam criteria In 2003, American and European reproductive societies met in Rotterdam todetermine a consensus about the diagnostic criteria for PCOS. The following criteria were put:
These criteria require two out of three of the following to make a diagnosis :
(#Ovulatory dysfunction( oligomenorrhea or amenorrhea
#Hyper androgenism, or hyper androgenemia .
#Polycystic ovaries (PCO)by US (unilateral or bilateral ).
# Inaddition to exclusion of other causes of hyper androgenism and oligomenorrhea
1-Ovulatory dysfunction
Most patients with PCOS have ovulatory dysfunction which is manifested as :
a. Oligomenorrhea is defined as 35 or more days between menses, or less than ten menses per year or amenorrhea (no menses).
b. A total of 60% to 85% of patients with PCOS will have oligomenorrhea, but the remainder may have normal menses.
c. As a result of irregular ovulation, these women lack adequate progesterone and experience chronic estrogen exposure to the endometrium. this can result in breakthrough or irregular
uterine bleeding and can put these patients at increased risk for endometrial hyperplasia and endometrial carcinoma .
2- Hyper androgenism
Patients may either have clinical or biochemical hyperandrogenism.a. Clinical hyperandrogenism Women with PCOS may exhibit hirsutism, acne, or male pattern hair loss while hyperandrogenemia means elevated tertosterone in blood
(1) Hirsutism is defined as excess pigmented hair in a male pattern distribution, most commonly found in midline areas of the body such as on the upper lip, chin, neck, chest, lower abdomen, and inner thighs. Male pattern baldness is also associated with hyper androgenism.
The Ferriman–Gallwey score, can be used to clinically estimate the extent of hirsutism and a score greater than or equal to 8 is considered abnormal.
(2) Acne may be a more sensitive clinical sign of hyperandrogenism, especially in adolescents
(3) The rate of hair growth is also clinically important. PCOS is associated with slow but progressive hair growth.
b. Biochemical hyperandrogenia
Up to 90% of women with PCOS have elevated serum androgen levels. the androgen levels may be normal even in the presence of clinical hyperandrogenism due to increased end organ sensitivity.3-Polycystic ovaries by pelvic ultrasound
PCO by ultrasound criteria is defined as(1) Twelve or more antral follicles between 2 and 9 mm in size , classically referred to as the “string of pearls sign” when follicles located peripherally in the ovary.
(2) Increased ovarian volume ( 10 mL) in one or both ovaries.
Transvaginal ultrasound is more sensitive than a transabdominal one particularly in obese patients, but may not be appropriate to perform in a unmarried female.
4. Exclusion of other causes of hyper androgenism and menstrual irregularities
((Differential diagnosisDifferential Diagnosis for Polycystic Ovary Syndrome
(Non classical congenital adrenal hyperplasia(CAH#Cushing’s syndrome
#Androgen-producing tumor: adrenal, ovary
#Thyroid disease
#Hyper prolactinemia
#Ovarian failure
#Drug exposure
#Hypothalamic amenorrhea
GENETICS AND ETIOLOGY OF PCOS
PCOS is thought to have a multifactorial etiologya genetic component in addition to environmental factors
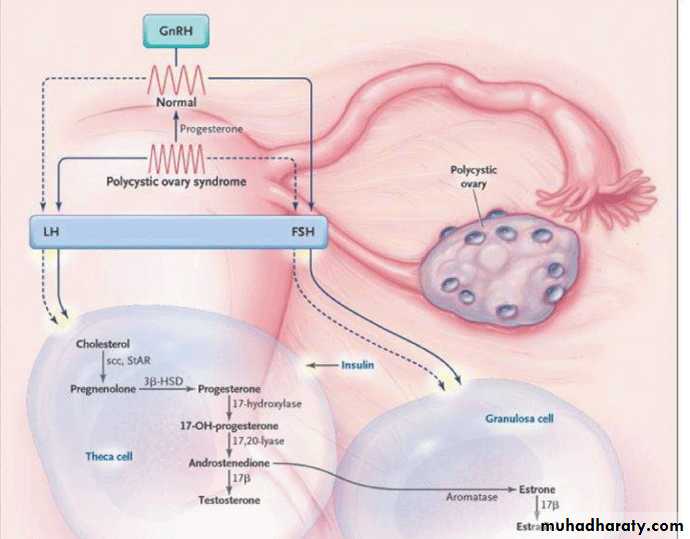
PATHOPHYSIOLOGY
The development of the symptoms and signs of PCOS may result from one or more of several abnormalities ultimately leading to a state of hyperandrogenism.
These include:
1-hyperinsulinemia This due to genetic defect in beta cell of pancreases gene , leading to continueous stimulatation of ovarian steroidogenesis (estrogen and testosterone).
2-Abnormal LH pulsatility causing increases production of androgens , LH stimulates production of androgens from the theca cells in the ovary. Normally, androgens in the ovary are converted to estrogens in the granulosa cells.
In women with PCOS, increased LH stimulation results in hyperandrogenism
EVALUATION
The diagnosis of PCOS can often be suspected by history and physical examination alone. However, laboratory evaluation is important to exclude other causes of the symptoms prior to confirming the diagnosis of PCOS.A -History
• Menstrual cycle frequency and duration:
• Menstrual irregularity (oligomenorrhea or amenorrhea) is indicative of oligo-ovulation or anovulation.
2. Onset and duration of hirsutism and acne
With PCOS, symptoms start with the onset of puberty and are slowly progressive. The rate and degree of hirsutism is variable among individuals. (PCOS associated with excessive hair growth but no virilization ).
3. Family history of diabetes and cardiovascular disease
B-Physical findings
1. Hirsutism
Excess male pattern hair growth seen primarily in areas such as the face, jaw, chin, neck, midline on chest and abdomen, and inner thighs and no sign of virilization(breast atrophy , increase muscular built ,glitoromegally )2. Acne
Usually involves the face, chest, and back.
3. Signs of insulin resistance acanthosis nigricans: Raised, velvety, hyperpigmentation of skin, typically seen on the axilla, neck.
4- Hypertension: BP must be checked at every visit.
5. Obesity
a. Defined as a body mass index (BMI) greater than or equal to 30 kg/m 2
b. Incidence of obesity in women with PCOS is as high
c. Central obesity with an increased waist-to-hip ratio
C-Laboratory testing
1. Making the diagnosis:# Hyperandrogenemia may be documented via elevation in either total or free testosterone usually total testosterone less than 200 ng/dL ( if its more so suggestive of an androgen-producing tumor).
# LH :FSH ratio it is >2 in 40% of patient with PCOS.
2. exclusion of other causes of hyper androgenism or Anovulation
IF THE DIAGNOSIS UN CERTAIN
@Thyroid-stimulating hormone (TSH to exclude thyroid dysfunction )
@ Prolactin hyperprolactinemia. Prolactin may be elevated in up to 40% of patients with PCOS, but this is likely secondary to stimulation of the prolactin-producing cells by chronic estrogen and not related to the cause of the disease state.
@FSH and estradiol to exclude the possibility of premature ovarian failure in those women with oligomenorrhea or amenorrhea.
@17-Hydroxyprogesterone to rule out CAH.
@Increased production of cortisol is associated with Cushing’s syndrome.
3. Other testing that should be done once the diagnosis of PCOS is established
• Diabetes• it is important to screen for these conditions as treatment can prevent significant health problems. and therefore need to be rescreened every other year.
• Fasting lipid and lipoprotein levels
Although not involved in the clinical diagnosis of PCOS, abnormal lipid profiles are common in PCOS patients (elevated triglycerides and low high density lipoprotein (HDL) concentrations ) predispose to vascular and cardiac disease, and therefore measurement and treatment of serum lipid levels is recommended every other year
HEALTH CONSEQUENCES of PCOS
A- Diabetes
women with PCOS, the prevalence of diabetes and Impaired glucose tolerance diagnosed is high
B -Obesity
Obesity has been reported in 30% to 70% of all patients with PCOS. The obesity is most often truncal with an android appearance and an increased waist-to-hip ratio. Obesity is related to insulin resistance.
C- Cardiovascular disease women with PCOS have an increased risk for cardiovascular disease. This is related to an increased risk for hypertension, dyslipidemia and glucose abnormalities.
D -Endometrial hyperplasia
Chronic anovulation exposes the endometrium to unopposed estrogen, which puts women with PCOS at risk for endometrial hyperplasia. If left untreated, endometrial hyperplasia may progress to endometrial cancer.
E- Infertility
Is associated with PCOS. The cause of the infertility in these women is primarily an ovulation
TREATMENT of PCOS
Treatment of PCOS involves treating each manifestations of the disorder (treat what the patient suffer from).A .Menstrual irregularity Prolonged unopposed estrogen
Treatment with progestin is important to prevent hyperplasia and regulate menstrual bleeding.
a. Combined hormonal contraception: oral contraceptive pills
b. Only progestin therapy, either cyclic oral progestin therapy, administered 12 days a month, implant, or progestin-containing intrauterine device.
B.Treatment of hirsutism
1. Mechanical removal of haira. Shaving, plucking, bleaching, depilation
b. Electrolysis achieves permanent hair removal. If done incorrectly, it may be associated with
scarring
c. Laser epilation is most effective and now available for women of most skin colors
d. Eflornithine HCl (Vaniqa) cream which inhibits enzyme ornithine decarboxylase, acts directly
at the hair follicle, and slows facial hair growth
2. Combined hormonal contraception
Combined contraception with estrogen and progestin
works to treat hyperandrogenism by the following mechanisms:
a. Decreases androgen production through suppression of LH and therefore suppresses androgen
production by the ovarian theca cells
b. Increases production of SHBG, which in turn decreases free circulating androgens
c. May decrease androgen secretion by the adrenal gland
3. Antiandrogens
work to suppress hirsutism by competitive inhibition at the level of the testosterone
receptor. these agents are used with hormonal contraceptives TO PREVENT PREGNANCY BECAUSE IT IS TERATOGINIC
a. Spironolactone aldosterone antagonist; and the clinical effect may take several months and may induce hyperkalemia
b. Flutamide androgen-receptor agonist
c. Finasteride 5 ALFA reductase inhibitor
d. Cyproterone acetate
C. Metabolic correction
since the underlying condition in PCOS is insulin resistance, treating insulin resistance via weight loss or by insulin-sensitizing agents result in improvement in PCOS symptoms
• 1.Weight loss:
• Obesity is associated with worsening of PCOS symptoms including menstrual
irregularity, insulin resistance, risk of diabetes, and hyperandrogenic symptoms , infertility.
a. Weight reduction results in improvement in all symptoms of women with PCOS.
b. Dietary modification with exercise .
c. Medication .
d. Bariatric surgery may be another modality for treatment .
2. Metformin (biguanide)
That acts by decreasing hepatic glucose production and may also increase peripheral glucose utilization. It is primarily used to prevent the progression of impaired glucose tolerance (IGT) and for the treatment of diabetes. Women with PCOS metformin can
a. Improve menstrual cyclicity and ovulation rates
b. May decrease serum androgens
c. Improve insulin resistance
d. Weight loss with metformin occurs only in conjunction with a low-calorie diet and exercise regimen
e. Side effects are primarily gastrointestinal, including nausea and diarrhea
.
D-Treatment of infertility
Women with PCOS often have difficulty conceiving because of the failure to ovulate regularly1-Drugs
1. Clomiphene citrate is an antiestrogen that has been used to induce ovulation, and is the first-line treatment for anovulatory infertility.
2. Metformin is associated with an improvement in ovulation. metformin alone or in those who do not respond to clomiphene alone then add metformin
3. Gonadotropins injectable FSH alone or in combination with LH, is successful in inducing ovulation , used for women who fail clomiphene therapy Side effect multiple gestation and ovarian hyperstimulation,.
4. Aromatase inhibitors such as letrozole is currently being studied for use to induce ovulation in women with PCOS
2- In vitro fertilization
is successful in achieving pregnancy and ovulation in women with PCOS,
but is a more aggressive therapy than the previous options.
3-Surgery
Laparoscopic ovarian drilling (with laser or diathermy) is another second-line option for fertility.
Ovarian wedge shape resection (done in the past )