Approach to Chest Pain
Dr. Zaid M. YassenAsst. Prof. Family Medicine
Chest pain or discomfort is one of the most common complaints in both the outpatient and emergency setting.
Assessing the cause of such symptoms in a rapid fashion is of utmost importance.
If the patient is experiencing
myocardial ischemiaor infarction, time is
myocardium.
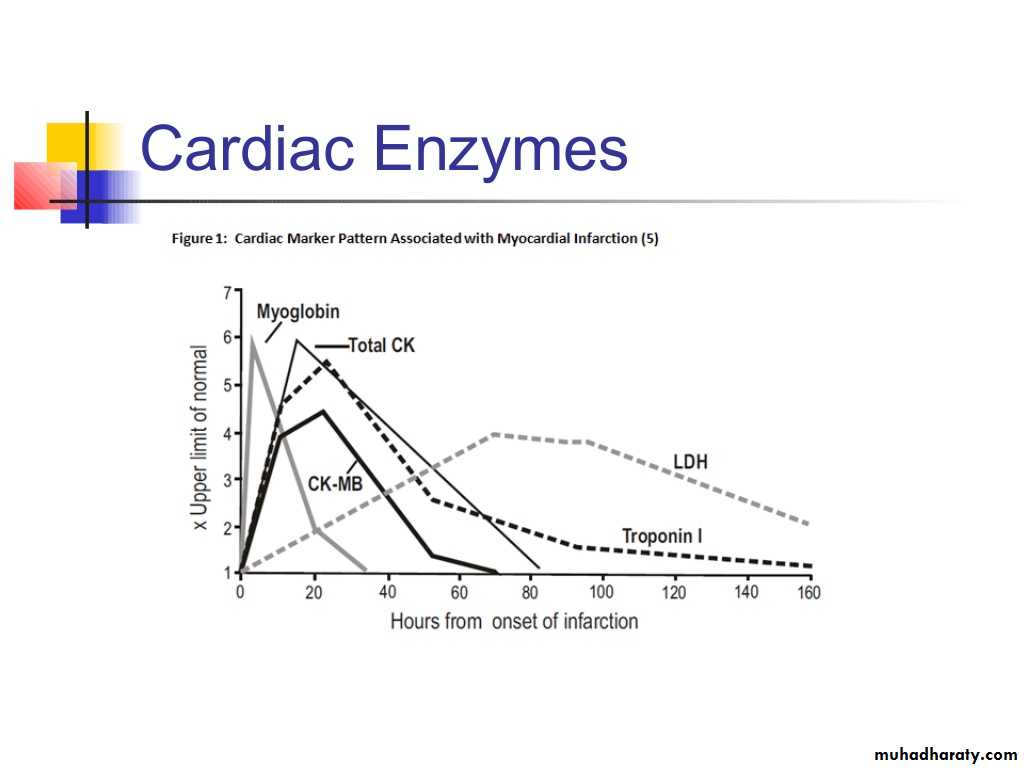
Initial evaluation should be done within 10 minutes of presentation and the goal of this evaluation should be to determine the need for further testing such as cardiac enzymes, stress test, or angiography.
Ischemic heart disease
remains the leading cause
of morbidity and mortality.
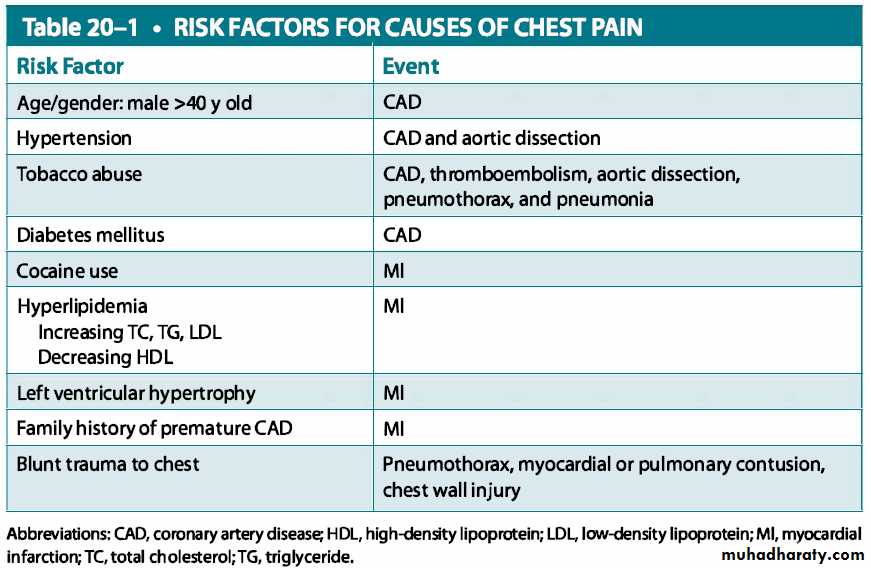
It is important to identify risk factors for coronary artery disease in patients, the presence of which would indicate an increased suspicion for an acute MI.
Male gender, age older than 60 years, diaphoresis, radiation of pain to neck, arm, shoulder, or jaw, and a past history of angina or acute MI are all considered risk factors.
Obtain an abbreviated chest pain history and determine early on if pain is emergent or nonemergent
If severe chest pain with shortness of breath or diaphoresis presents, then evaluate for cardiac cause.
Determine the severity (0 to 10), character, onset, duration, location, radiation, and alleviating and exacerbating factors of the chest pain.
Does the pt complain of chest pain that suggests cardiac origin?
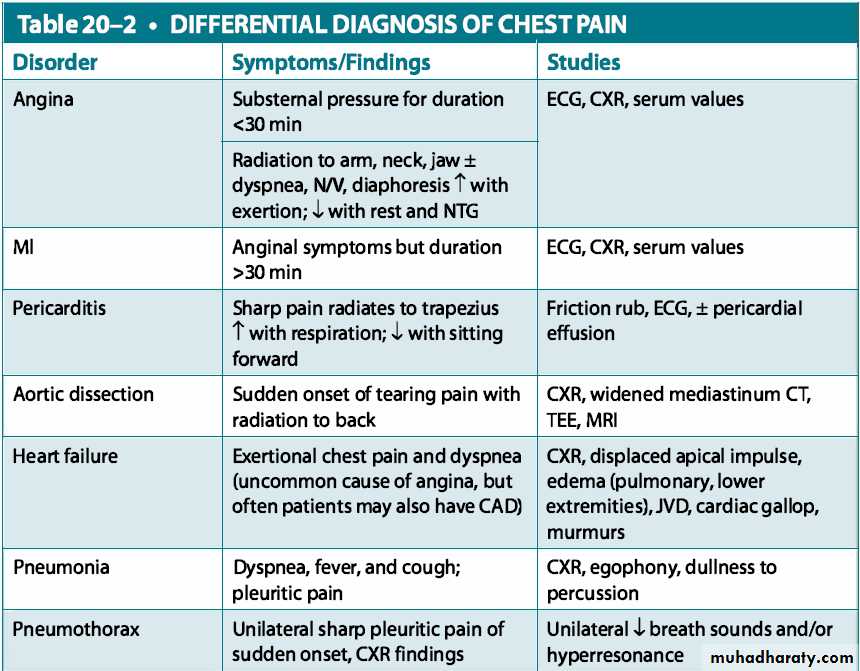
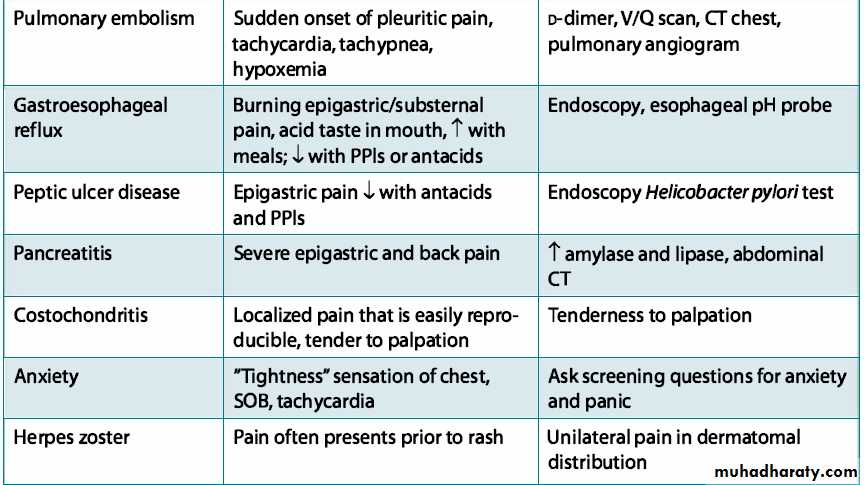
Typical cardiac pain is described as a substernal pressure-like sensation or tightness with associated radiation to the left arm, neck, jaw, or back.Chest pain in diabetics may be mild or nonexistent.
Ascertain if there are risk factors for chest pain (e.g., age, male sex, smoker, hypertension, hyperlipidemia, or family history of heart disease).
Does the pt complain of chest pain that suggests cardiac origin?
Pain can be present at rest (unstable angina) or with exertion (stable angina).
Typical cardiac chest pain may resolve or improve with nitrates.
Any gastrointestinal symptoms associated with the chest pain?Epigastric or burning pain associated with gastritis or ulcers may be mistaken for cardiac pain.
Determine if the pain is related to or relieved by meals, anorexia, or antacids.
Sharp pain localized over the sternum may indicate esophageal spasms.
Dysphagia or odynophagia may cause chest pain.
Is the chest pain reproducible or exacerbated by movement?
Determine if there is repetitive activity, trauma, or injury to the chest wall.Pain with movement of arms, shoulders, or chest wall may indicate musculoskeletal injury.
Musculoskeletal injuries such as rib fractures can cause chest wall pain with inspiration, at rest, or with movement.Does the pt have a history of psychological illness?
Panic attacks can present with chest pain along with associated symptoms of shortness of breath, palpitations, dizziness, tremors, tingling, sweating,depersonalization, or feelings of imminent death.
A history of anxiety, depression, or nervousness can point to a psychological cause.
Has the pt had any history of pulmonary problems?
Pulmonary illnesses can present with cough, wheezing, or shortness of breath.
Fever and chills may indicate an infection.Check vital signs
Determine hemodynamic stability.Check blood pressure in bilateral arms.
Perform physical exam
General: Observe for signs of anxiety or nervousness.Examine neck for jugular venous distention, carotid pulses, and bruits.
Chest: Perform a complete chest exam; palpate for reproducibility of pain.
Heart: Check rate, rhythm, and auscultate for abnormal heart sounds.
Abdomen: Check for abdominal pain or bruits.
Musculoskeletal: Examine arms, shoulders, and chest wall for tenderness.Perform the following tests or labs if indicated by history and physical exam
ECG to rule out cardiac origin of chest painPulse oximetry if shortness of breath
CXR
If epigastric pain is present, consider ultrasound, upper endoscopy, upper gastrointestinal series, or barium swallow if indicated.
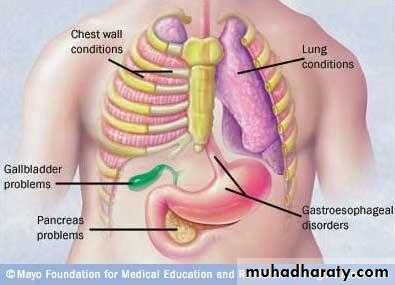
Common etiologies include:
Cardiac causes:(Cardiac ischemia, Congestive heart failure, Valvular disease, Pericarditis, Dysrhythmias)
Gastrointestinal causes:
(Gastritis, gastroesophageal reflux disease, Peptic ulcer disease, Esophageal spasms, Dyspepsia or flatus)
Musculoskeletal causes:
(Chest wall muscle strain, Costochondritis, Upper body trauma or rib fractures)
Psychological causes:
( Panic attacks, Generalized anxiety disorder, Stress, Somatization, Depression)Pulmonary causes:
(Pneumonia, Bronchitis, Pleurisy, Pulmonary embolism, Pneumothrorax)Admit pt to hospital if emergent
If cardiac ischemia is suspected, give pt aspirin, oxygen, sublingual nitroglycerin, and check ECG.If nonemergent, focus treatment on specific cause determined by history and physical
Refer to cardiology for a stress test, echocardiogram, or cardiac catheterization.Remember that myocardial infarction should be ruled out in the hospital.
Appropriate therapy can be started when the diagnosis is made.
CLINICAL PEARLS
Angina pectoris is the most frequent symptom of intermittent ischemia.Targeted history and physical examinations of patients with angina are vital to expedite proper diagnosis and treatment of patients.
CLINICAL PEARLS
The patient's description of their discomfort is key; history must be given attention because it is the most important diagnostic factor.
Physical examination may be normal in many patients with angina.
CLINICAL PEARLS
Aspirin, nitrates, adrenergic antagonists, and statins are the backbone in treatment and prevention of myocardial pathology, having proven benefit for both primary and secondary treatment.CLINICAL PEARLS
Time is myocardium. Initial diagnosis and treatment must be done as soon as possible.Be mindful of polypharmacy, as many drugs have side effects that can exacerbate myocardial damage.
CLINICAL PEARLS
The most common etiology of chest pain in the primary care setting is musculoskeletal. However, it is imperative to rule out cardiac cause of chest pain before making a musculoskeletal-related diagnosis.