RED EYE
Dr. Anmar AldewachiAss. Prof. Of Family Medicine
M.B.Ch.B, MD,MPH,JHSFM
Red Eye
Red eye is one of the most common ophthalmologic conditions in primary care.It can be caused by inflammation of almost any part of the eye, including the lacrimal glands and eyelids.
Diagnosis can be reached with detailed history and careful eye exam.
Treatment of red eye is based on the underlying etiology
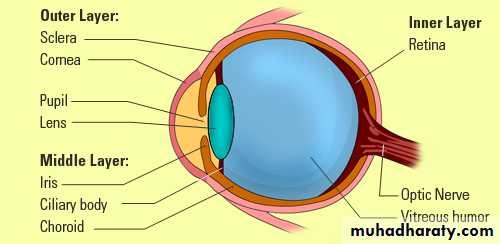
Layer of eye
Differential diagnosis
Differential diagnosis of red eye
• Conjunctivitis
• Subconjunctival hemorrhage.
• Blepharitis.
• Corneal abrasions and foreign body.
• Keratitis
• Uveitis
• Acute glaucoma.
• Chemical burn.
• Scleritis
CONJUNCTIVITIS
The most common cause of red eyeThe cause of conjunctivitis may be
• Infectious (e.g., viral, bacterial, chlamydial)
• Noninfectious (e.g., allergies, non-allergic (irritant)).
Bacterial Conjunctivitis
PresentationRed eye.
Mild to moderate pain with stinging sensation.
Mild to moderate purulent discharge, mucopurulent Secretions with bilateral glued eyes upon awakening (best predictor)
Examination
Purulent discharge at the
lid margins and in the
corners of the eye
Conjunctival redness
Normal pupil size& reaction
Normal visual acuity
• Causes
Staphylococcus aureus in adultsStreptococcus pneumoniae, Hemophilus influenzae, and Moraxella catarrhalis more common in children
Highly contagious, spread by direct contact with the patient secretions or with contaminated objects and surfaces.
Treatment of Bacterial Conjunctivitis
Antibiotics: Studies did not show the superiority of one antibiotic over another.
The choice of antibiotic should be based on cost-effectiveness and local bacterial resistance patterns
Erythromycine ,Trimethoprim-polymyxin B ,Azithromycine, Ciprofloxacine
Bacterial Conjunctivitis
Patients should respond to treatment within 1-2 dayPatients who do not respond should be referred to an ophthalmologist.
Immediate Use of Antibiotics in Bacterial Conjunctivitis is indicated for:
Health care workers
Patients who are in a hospital or other health care facility
Patients with risk factors: immunocompromised, uncontrolled diabetes mellitus, contact lens use, dry eye, or recent ocular surgery
Children going to schools or day care centers.
Viral Conjunctivitis
PresentationMild to no pain.
Diffuse hyperemia.
Burning, sandy feeling in one eye.
Occasional discomfort with mild
itching.
Watery to serous discharge
Photophobia (uncommon),
Often unilateral at onset with second eye involved
within one or two days.
Viral symptoms at the same time: runny nose, low grade fever…
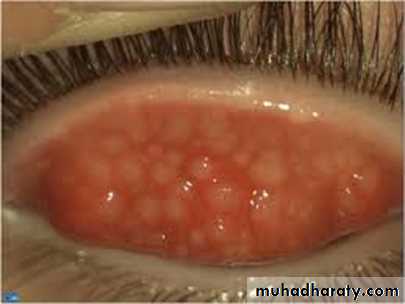
Viral Conjunctivitis
• ExaminationNormal vision.
Normal pupil size and reaction to light.
Diffuse conjunctival injections (redness)
Tarsal conjunctiva with follicular appearance
Enlarged and tender pre-auricular node may be present
• Causative agent:
Typically caused by adenovirusHighly contagious: it is spread by direct contact with the patient secretions or with contaminated objects and surfaces.
Management of Viral Conjunctivitis
Self-limited process
Symptomatic relief from topical antihistamine/decongestants
Warm or cool compresses may provide additional symptomatic relief
Recovery can begin within days, but symptoms may persist 2-3 weeks
Allergic Conjunctivitis
• Presentations
Bilateral redness
Watery discharge
Itching (cardinal symptom of allergy)
Often history of atopy, seasonal allergy, or specific allergy
Allergic Conjunctivitis
• ExaminationDiffuse injection (redness) with a follicular appearance of the tarsal conjunctiva
Profuse watery or mucoserous discharge.
May be morning crusting
In some cases, marked chemosis (conjunctival edema)
It is caused by airborne allergens
Non-infectious Non-allergic Conjunctivitis
The discharge is more likely mucus.Caused by: a transient mechanical or chemical insult.
Patients with dry eyes may report chronic or intermittent redness & discharge
Patients whose eyes are irrigated after a chemical splash may have redness and discharge
A patient with an ocular foreign body that was spontaneously expelled may have redness and discharge for 12 to 24 hours.
Spontaneous improvement in 24 hours
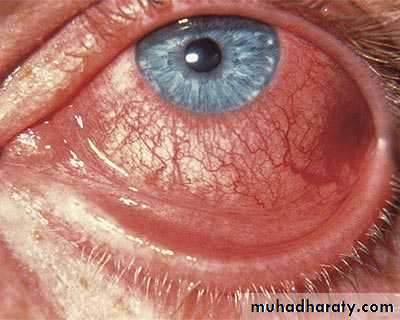
SUBCONJUNCTIVAL HEMORRHAGE
Presentation :Mild to no pain
No vision disturbances.
No discharge
O/E
Normal vision
Pupils equal and reactive to light.
Well demarcated, bright red patch on white sclera;
No corneal involvement.
Causes
• Spontaneous causes:Hypertension.
Severe coughing, straining and Valsalva maneuver
Atherosclerotic vessels.
Bleeding disorders.
Use of antiplatelet agents
Use of high doses vitamin E (> 1,000 mg/d)
• Traumatic causes:
Blunt eye trauma
Foreign body
Penetrating injury
Management
Reassure patient that it will resolve spontaneously.Measure Blood Pressure.
In case of recurrence, check for bleeding problems.
Eyes with subconjunctival hemorrhage in the setting of blunt trauma must be evaluated for the possibility of ruptured globe or retrobulbar hemorrhage.
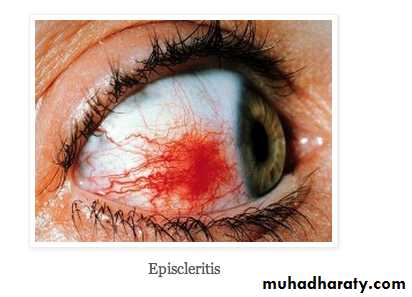
EPISCLERITIS
Benign cause of red eye caused by inflammation of episcleral tissue.It is usually self-limiting (lasting up to three weeks)
The patient present with mild to no pain; limited, isolated
patches of injection; mild watering.
O/E:
Normal visual acuity.
Pupils equal and reactive to light.
Dilated episcleral blood vessels
Edema of episclera.
Tenderness over the area of injection
Confined red patch
EPISCLERITIS
• Management• Symptomatic relief should be the goal of therapy and can be achieved with:
Topical lubricants to be used 4-6 times daily
Topical NSAIDs not as primary therapy
Topical glucocorticoids only when the patient remains highly symptomatic despite optimal use of other treatments and is directed by an ophthalmologist
Oral NSAIDs for patients who do not respond to the above topical therapies
EPISCLERITIS
Investigation is indicated for recurrent episodes and for symptoms suggestive of associated systemic diseases, such as rheumatoid arthritis.Ophthalmology referral is required for recurrent episodes, an unclear diagnosis (early scleritis), and worsening symptoms.
• Scleritis
Inflammatory condition involving the outer white coating of the eye (sclera).Associated with systemic diseases such as rheumatoid arthritis, reactive arthritis, sarcoidosis, inflammatory bowel disease, syphilis, T.B.
• Presentation:
• Severe, boring pain radiating to
periorbital area increases with eye
movements.
• Ocular redness.
• Watery discharge.
• Photophobia.
• Intense nighttime pain; pain upon
awakening
Scleritis
O/EDiffuse redness.
Diminished vision,
Tenderness, scleral edema.
Corneal ulceration.
Scleritis needs referral to ophthalmologist.
UVEITIS
Uveitis is inflammation of the uvea— the middle layer of the eye that consists of the iris, ciliary body and choroid.Presentation:
Acute onset
Constant eye pain
Photophobia
blurred vision
Examination
Ciliary flush: is a ring of red or violet
spreading out from around
the cornea of the eye
Pupil : irregular shape, constricted and poorly reacting to light.
• Causes
Most commonly idiopathicCo-morbidities can be present: sarcoidosis, connective tissue, infectious tuberculosis, herpes simplex virus and others.
• Management
Refer patients to an ophthalmologist to help avoid visual consequences.
Treatment
Start with topical corticosteroid
Oral corticosteroids
Long-term immune suppression.
• Keratitis
Inflammation of corneaPresentation
Painful red eye
Diminished vision.
Photophobia.
Mucopurulent discharge.
Examination
Diminished vision.
Corneal opacities/white spot.
Fluorescein staining under
Wood lamp shows corneal ulcers.
Eyelid edema.
Hypopyon
• Causes
Bacteria (staphylococcus aureus, pseudomonas aeroginosa, streptococcus pneumonia….)Viruses (herpes simplex virus)
Fungi, or parasites
Improper contact lens wear is the largest risk factor for bacterial keratitis
• Management of Keratitis
Bacterial keratitis : requires urgent ophthalmological referral and rapid initiation of topical bactericidal antibiotics (ideally after obtaining cultures).
Viral keratitis : although typically a self-limited process, duration of symptoms is reduced with treatment with topical or oral antiviral agents.
Immunocompromised patients may require topical and systemic treatment, and longer duration of therapy.
Acute Glaucoma
PresentationPatient appears to be in general distress
Headache unilateral dull and malaise
Nausea and in some cases vomiting
Photophobia sometimes
Examination
Red eye with ciliary flush
Reduced visual acuity (worsening with the duration of attack)
Pupil fixed in mid-dilation and the anterior chamber is shallow.
Within hours of symptom onset the cornea becomes hazy
Management of Angle-Closure Glaucoma
Diagnosis is confirmed with measurement of intraocular pressure :
Normal is 8 to 22 mm Hg
In acute angle closure > 45 mm Hg
Acute glaucoma is a sight-threatening emergency that must be treated within hours to avoid irreversible damage to the optic nerve.
Immediate referral to ophthalmologist once diagnosed.
Evaluation of red eye
Medical historyUnilateral or bilateral involvement.
Pain.
Discharge (type and amount of discharge)
Itching
Photophobia
Visual changes (decreased visual acuity).
Associated symptoms: headache, nausea, vomiting
Foreign body sensation :Evidence of foreign body sensation, in which the patient is unable to spontaneously open the eye or keep it open, suggests corneal involvement.
Hx of trauma.
Contact lens use :A history of contact lens wear in the setting of discharge and a red eye should increase the suspicion of keratitis.
History taking
Medical problems :Hypertension, diabetes mellitus.
Symptoms and signs potentially related to systemic diseases.
Physical Exam
Assess the pattern and location of the redness
Check pupil size and reaction to light
Check the color and type of discharge
Examine the cornea and anterior segment (with pen light) for Corneal opacities, hypopyon and hyphema.
Check visual acuity (Snellen chart or near vision).
Check for pre auricular lymph nodes
Indications for Immediate Referral to Ophthalmologist Based on History
Severe painVisual loss
Marked pain or decreased vision with the use of contact lenses
Trauma
Chemical injury
Recent eye surgery
Indications for Immediate Referral to Ophthalmologist Based on Physical Exam
Decreased visual acuityPupil irregularity
Slow pupillary reaction to light
Corneal opacification
Hyphema or hypopyon
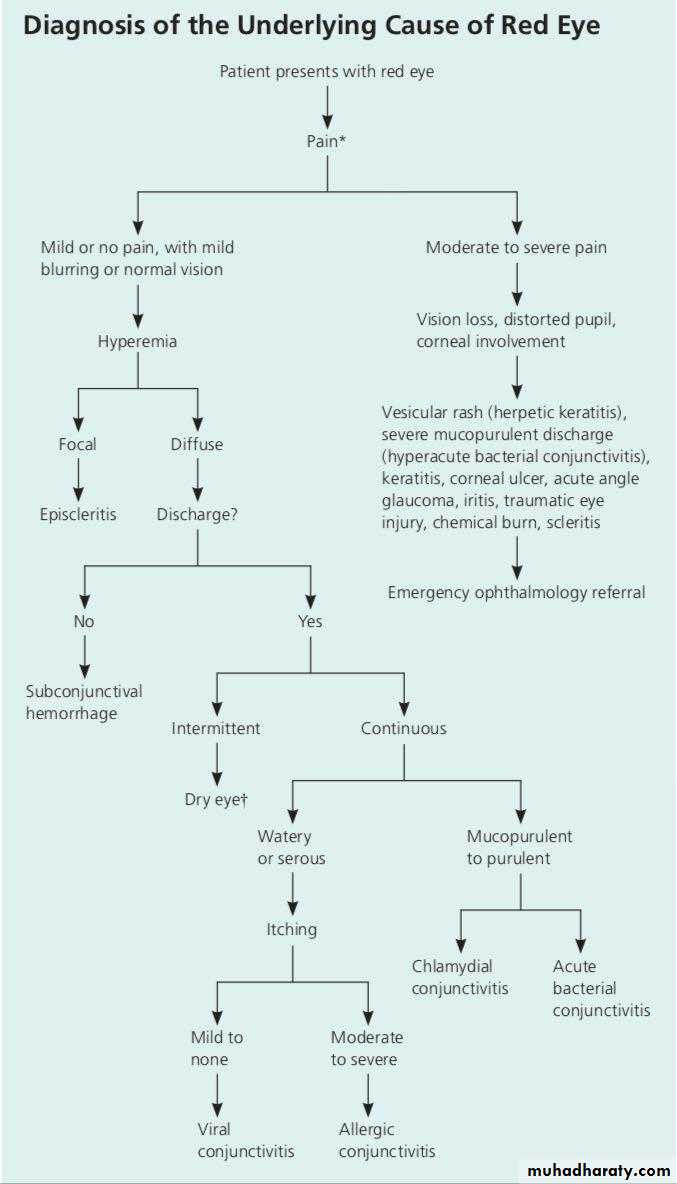
Algorithm for Dx of red eye