
1. Food and air inlet.
2. Play an important role in speech through vocal
resonance and articulation.
3.The protective function of Waldeyer's ring.
4. Deglutition: it's divided into 3 stages:
a. Oral stage (voluntary).
b. Pharyngeal stage (involuntary).
c. Oesophageal stage (involuntary).

1- Sore throat (pain)
a. Inflammatory: aphthus, tonsillitis and
pharyngitits.
b. Neoplastic: malignancy of oropharynx
or hypopharynx.
c. Neurological: IX neuralgia.
d. Blood dyscrasia: agranulocytosis and
leukaemia.
2- Dysphagia:
is difficulty in swallowing whereas
odynophagia is painful swallowing.
Dysphagia: Intraluminal: FB in the pharynx.
Luminal:
pyriform
and
post-
cricoid carcinoma.
Extraluminal:
retropharyngeal
abscess
3-
Sensation
of
a
lump
in
throat
:
Cricopharyngeal spasm, GERD, compression
from goitre, globus pharyngeus or malignancy.
4- Difficulty in breathing
: any pharyngeal
infection is likely to impede the airway leading
to stridor e.g. retropharyngeal abscess and
Ludwig's angina.
5- Difficulty in speech
: Paralysis of the soft
palate can lead to abnormal speech called
rhinolalia aperta (hypernasalily). This is in
contrary to rhinolalia clausa when there is
nasal obstruction by anything like common
cold or nasal polyps

Is a general term used to describe an
inflammation of the whole lining of the
mouth.
-Viral infection: Herpes simplex
-Bacterial:
Gingivitis,
periodontitis
and
actinomycosis.
-Fungal: candidiasis (thrush).
-Spirochaetes: Vincent's angina.
-Miscellaneous: Aphthus, Behcets syndrome,
pemphigus and pemphigoid.
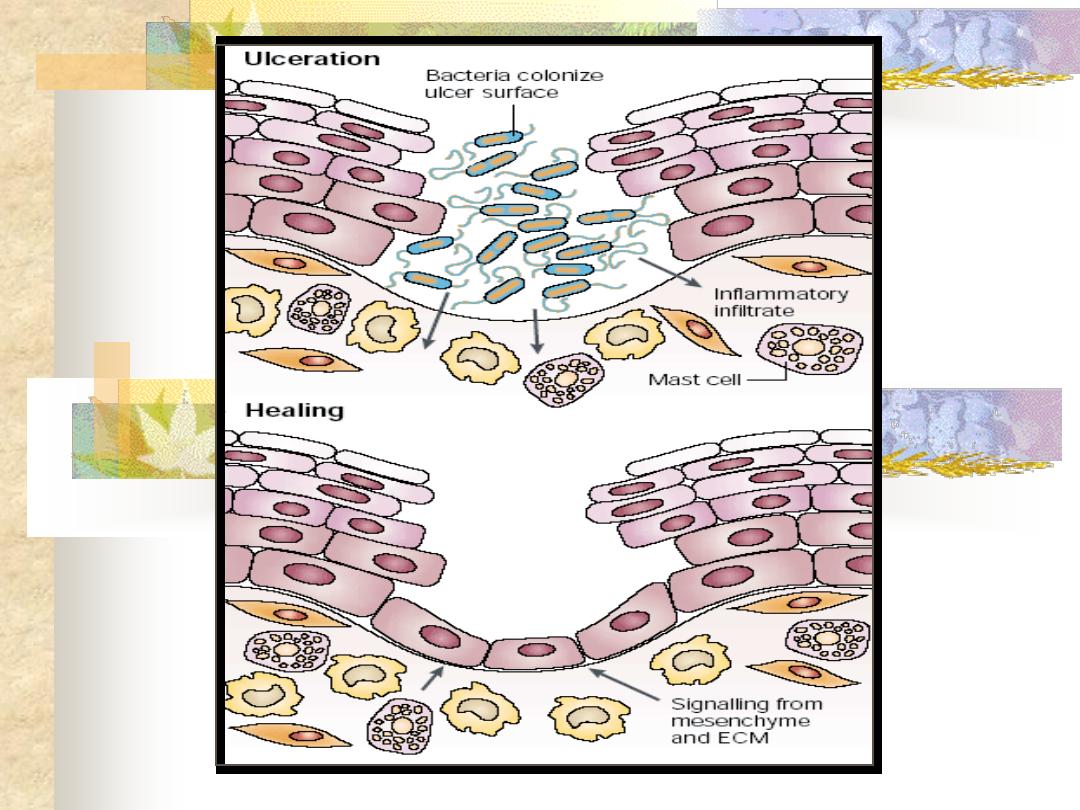
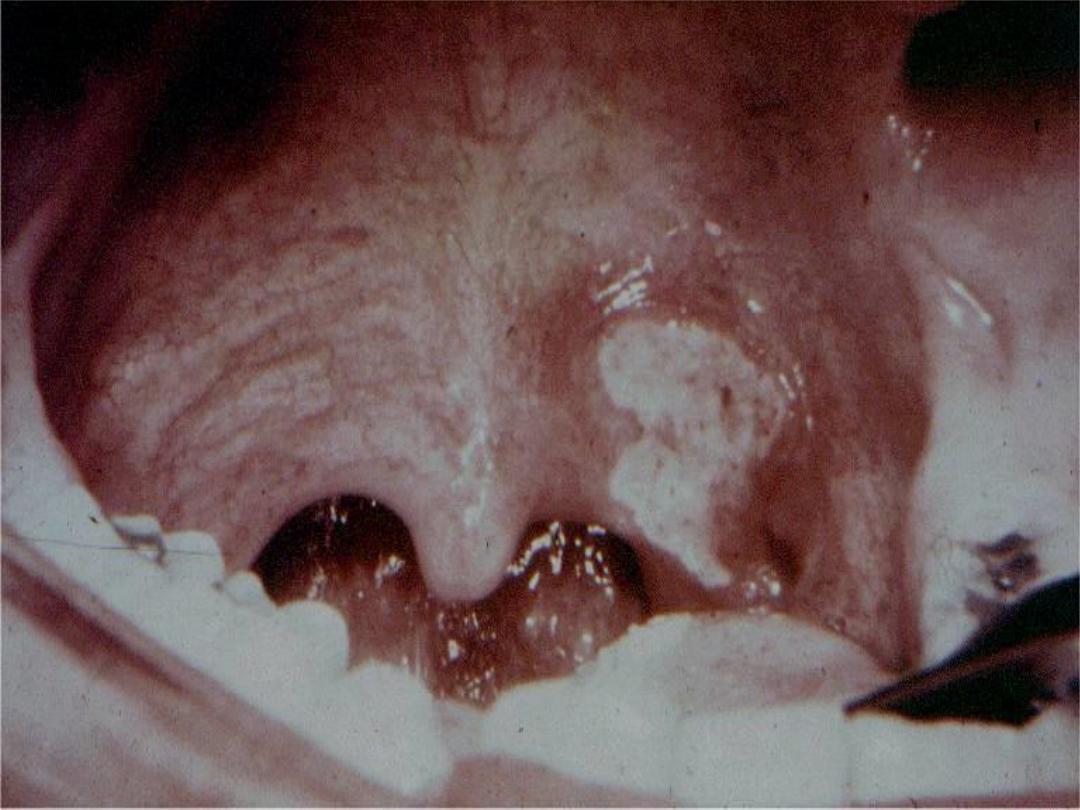
Recurrent ulceration of the oral mucosa
of unknown aetiology, viral, psychogenic,
endocrinal and autoimmune factors have
been
suggested.
Persistent
aphthus
ulceration especially in young males, must
bring to mind the possibility of AIDS.
Clinical picture
It's started as a small vesicle, which soon
ulcerates leaving an ulcer which varies in size.
This ulcer is typically quite sensitive and
painful, have a central necrotic base with a
surrounding red circumference. It disappears
after a few days.
Aphthus ulceration is of two types. In
the minor form, which is more common,
ulcers are 3-6 mm in size and multiple..
They heal within 7-10 days without leaving
a scar. Whereas, in the major form, ulcers
are 1-2 cm in size, less common, long
lasting and heal with a scar.

Treatment
Is symptomatic:
-Oral antiseptic: like chlorhexidine gurgle.
-Topical application of local analgesic like
xylocaine.
-Topical steroids e.g. Kenalog in orabase.
Systemic steroids should be used only in
major aphthus ulceration.
A condition of unknown aetiology comprising
both oral and genital ulceration with uveitis.
Clinical picture
Painful ulcers appear in the mouth and
anogenital region which are very similar to
aphthus ulcers, but of larger type.

These ulcers are punched out with a
sloughing
base
and
are
usually
surrounded by a red areola. These ulcers
heal within days or weeks, but
recurrence is usual. Blindness may result
from ocular lesions.
Treatment
Is non-specific, but steroids e.g. 20 mg
prednisolon /day
,
colchicin and azathioprin
have produced relief.

It's a gingivitis affecting the interdental
papillae producing ulceration and necrotic
membrane. This entity used to be called
"Trench Mouth" because of its prevalence
in soldiers fighting in the trenches during
world war I.
Aetiology
Infection with spirochaete Borrelia
vincenti and an anaerobic organism
Bacillus fusiformis.
Clinical picture
This condition occurs in debilitated patients
who have poor dental hygiene. The patient
feels ill, pyrexial complaint from sore throat
with tender lymphadenopathy.
Examination
The lesions originate around the interdental
papillae and gums and may spread to involve
the tonsil and oropharyx. The ulcers are
painful, associated with foeter (fishy odor),
whitish grey in colour and covered by a
slough.

ِAcute Necrotizing Ulcerative Gingivitis
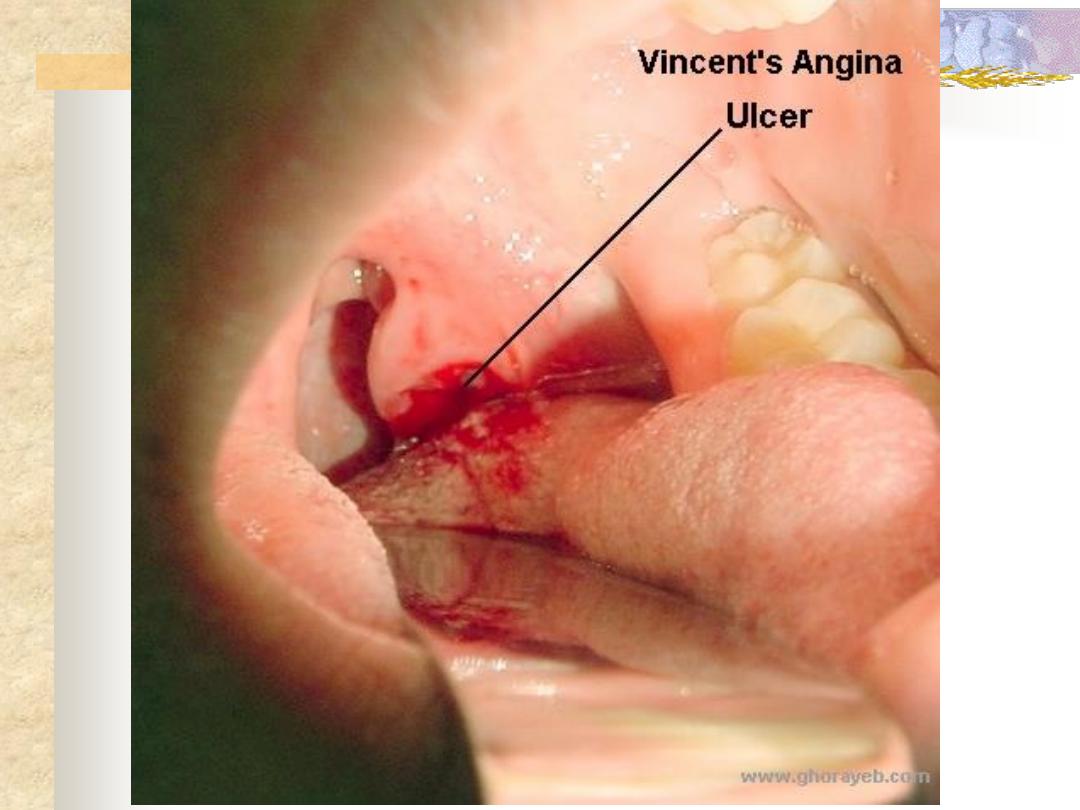
Diagnosis
Smear stained with gention violet.
Differential diagnosis
Diphtheria, IMN, tertiary syphilis and AIDS.
Treatment
-Oral hygiene by mouth wash and dental surgeon
if necessary.
-Paranteral benzyl penicillin + metronidazole.

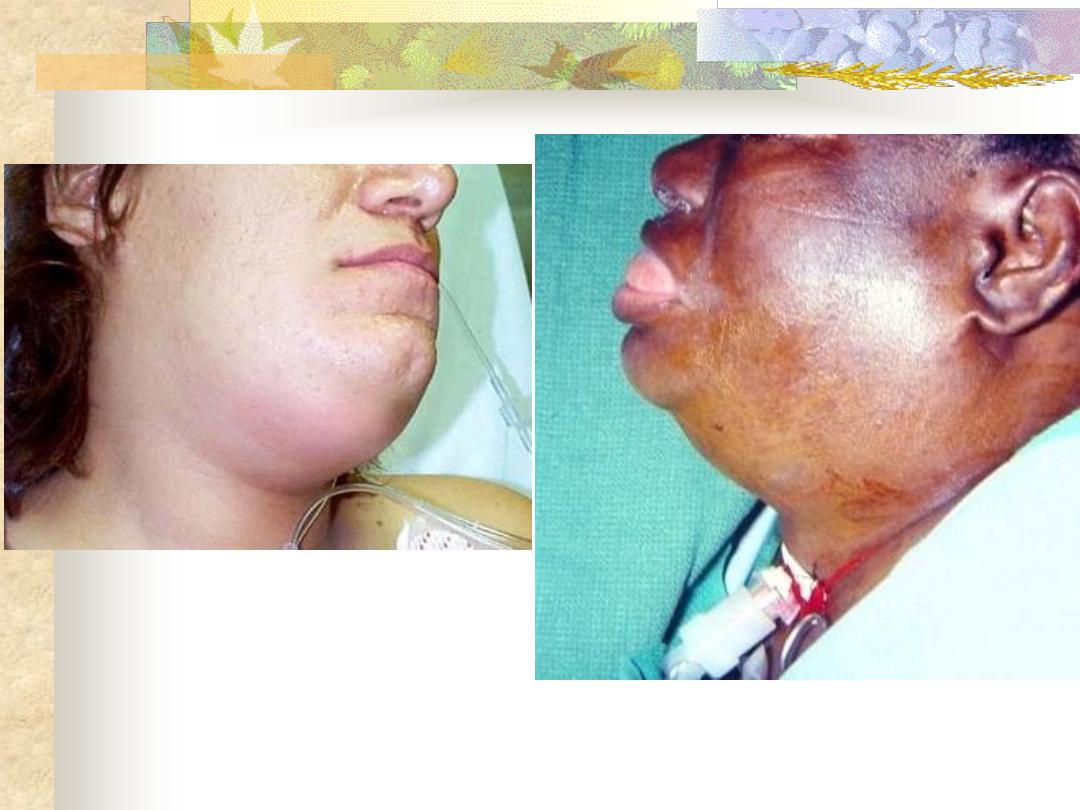
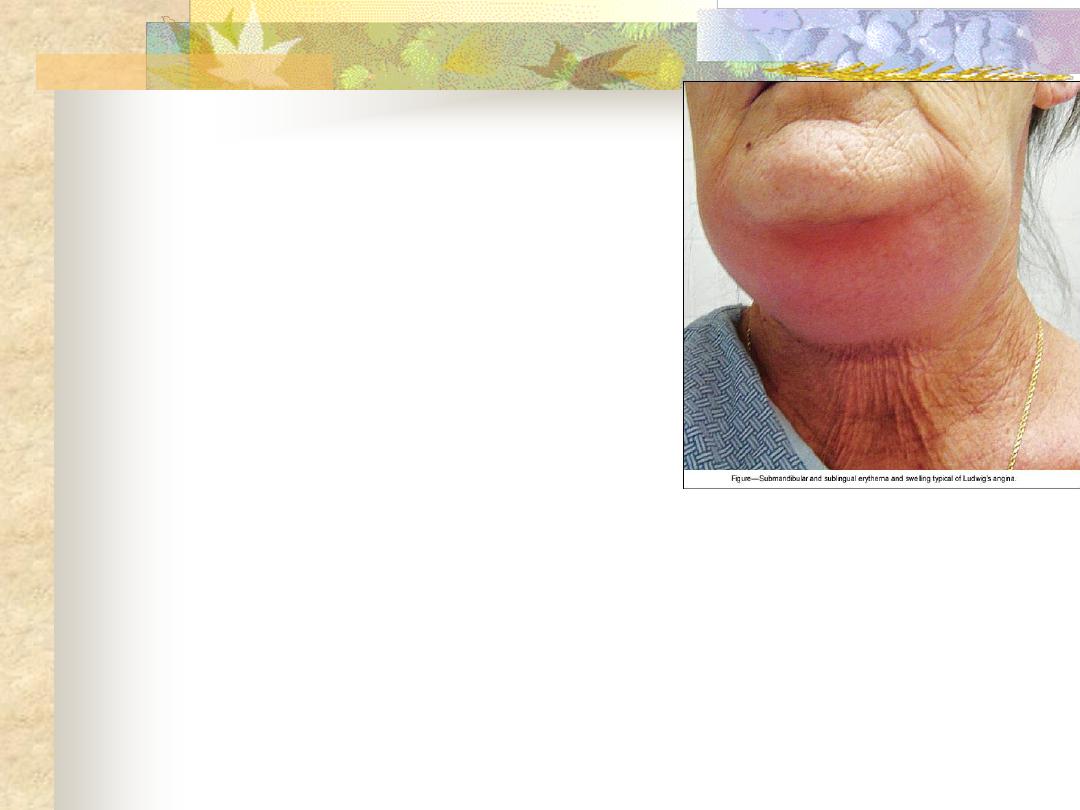
An acute cellulitis of the floor of the
mouth and submandibular space secondary
to soft tissue infection. The infection is
limited by the attachment of the fascial
spaces, so that tension rises rapidly and
laryngeal oedema occasionally occurs.
Aetiology
-Root abscess of the lower premolar and molar
teeth (80%).The most usual organisms are
strepto. viridans and E. coli.
-Tonsillar infection.
-Submandibular sialadenitis.
Clinical picture
The patient is ill, toxic > 38
o
C with
odynophagia and salivation.
On examination
There is an indurated and usually non-
fluctuant swelling below the angle of the jaw.
The floor of the mouth becomes very
oedematous with the tongue pushed upwards.
Potential complications
-Airway compromise due to laryngeal oedema.
-Spread
into
the
parapharyngeal
and
retropharyngeal spaces.
-Septicaemia.
-Aspiration pneumonia.
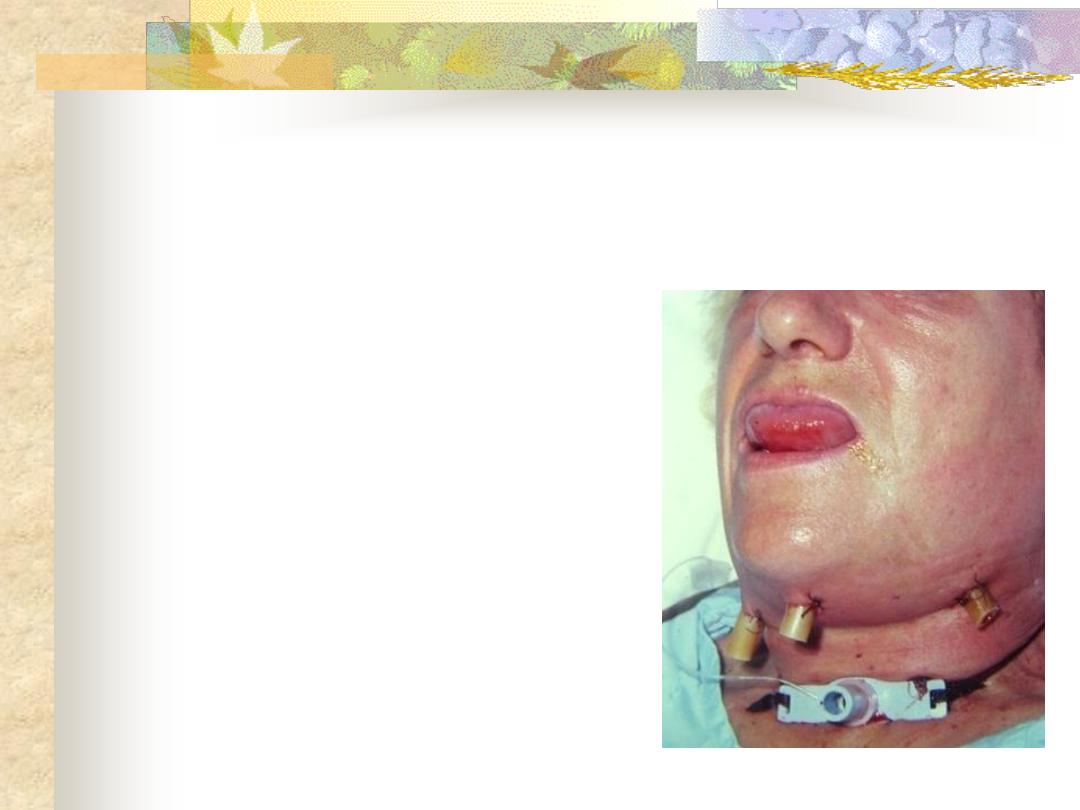
Ludwigs Angina
Treatment
-Early stages (early cellulitis): heavy antibiotics
covering aerobes and anaerobes.
-Drainage: if the state progress and the swelling
increases. Fluctuation should on no account
be awaited because it seldom occurs. Draining
is by a curved incision 2 cm below the angle
of the jaw using endotracheal tube.
-Endotracheal intubation and tracheostomy may
be required if laryngeal oedema supervenes.

Specific: Acute (diphtheria), chronic (T.B.).
Non specific: Acute , chronic.
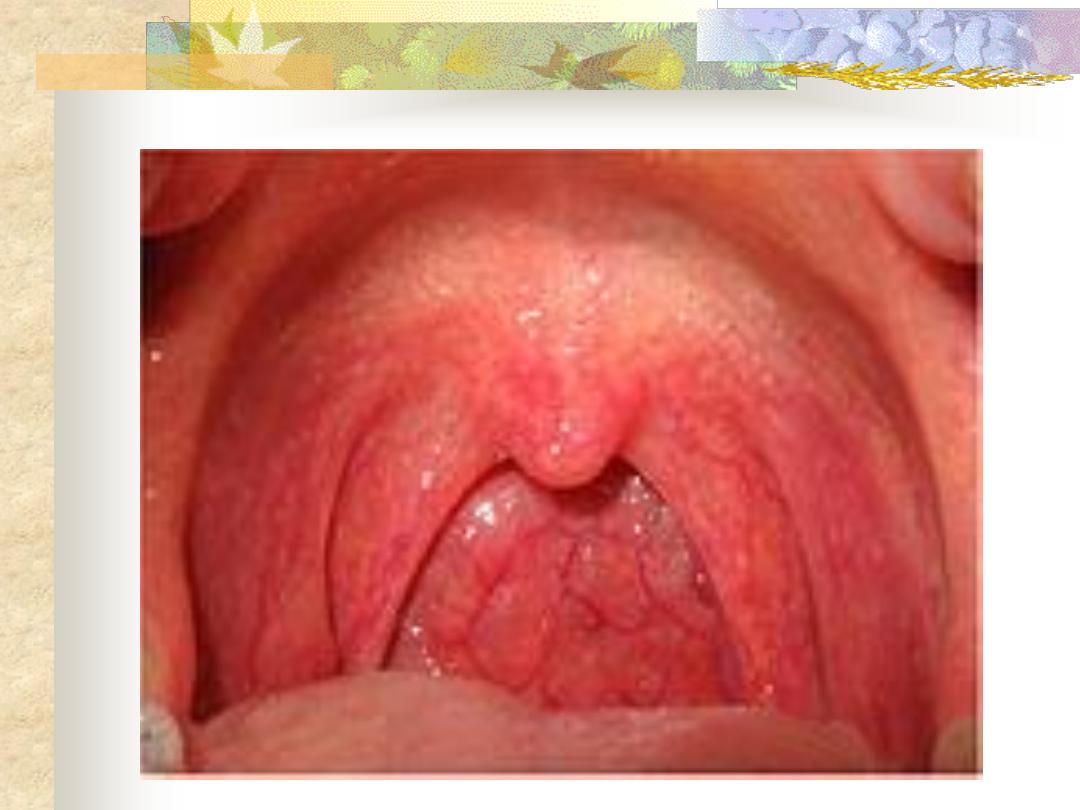
Acute
inflammation of the mucous
membrane of the pharynx occurring primarily
in winter months. Most of acute pharyngitis
are primary of the oropharynx, although the
nasopharynx and hypopharynx may become
involved secondarily.
Aetiology
40-60 % are viral in origin( mostly adenovirus
and rhinovirus).
20 % are bacterial: mostly Pneumococci,
Haemophilus influenza and group A beta-
hemolytic streptococci (S. Pyogens).
30 % No pathogen is isolated. This may be
due to post-nasal drip, smoking or gastro-
esophageal reflux disease (GERD) and these
are the three common causes of recurrent
pharyngitis !
Remember that pharyngitis may be part of the
clinical picture of measles, scarlet fever,
infectious mononucleosis and typhoid fever !
Symptoms
-Sore throat accompanied by a feeling of
coldness.
-Pyrexia, headache and joint pain.
Sings
-Redness and injection the mucous membrane of
the pharynx.
-Hypertrophic and proliferation of lymphoid
tissue on the posterior pharyngeal wall with
particular aggregates in the lateral pharyngeal
bands. In children Kopliks spots of measles
should be excluded.
- Oedema of uvula
-Tender and palpable cervical lymphadenopathy.
Acute pharyngitis
Treatment
-Symptomatic: bed rest, analgesics and fluid by
mouth.
-Antibiotics: if bacterial infection is suspected.

-Viral infection: infectious mononucleosis.
-Bacterial: diphtheria and scarlet fever.
-Fungal: candidiasis.
-Spirochaetes: Vincent's angina.
-Blood
dyscrasia:
agranulocytosis
and
leukaemia.
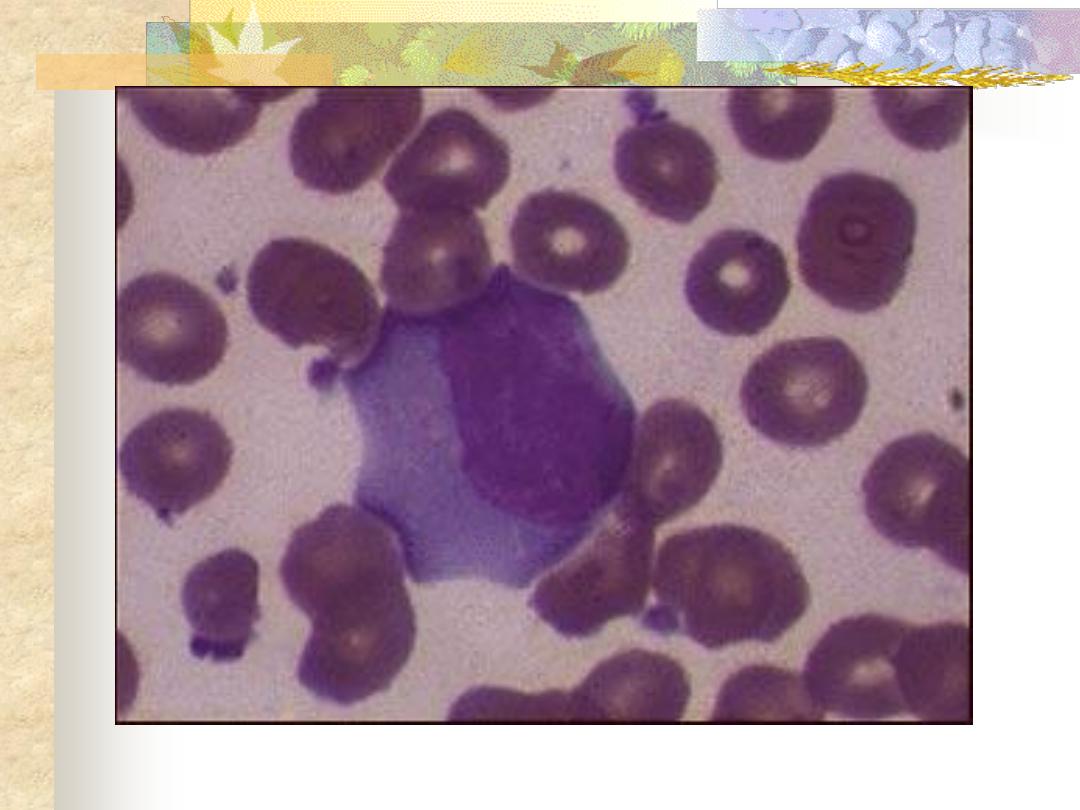
Is a systemic infection by Epestein Barr
virus which spread by droplets transmission.
It is a disease of young adults and
characterized by an increase in atypical
lymphocytes.
Clinical picture
-Prodromal period of 4-14 days
-Anorexia and low grade fever.
-Sore throat associated with odynophagia.
-Transient maculopapular rash.
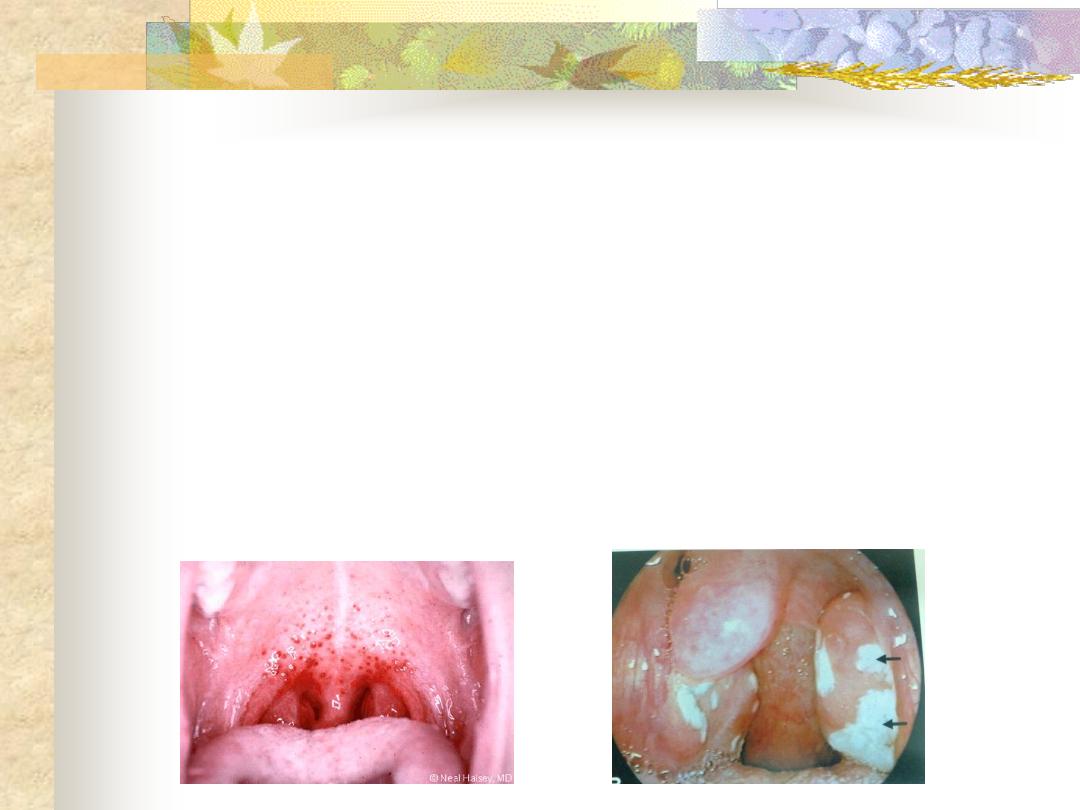
Examination
1. Pharyngeal congestion with superficial
ulceration of the tonsils. Red spots (patichae)
may appear on the soft palate.
2.
Enlargement of all lymphoid tissue within
Waldeyer
,
s ring unlike acute tonsillitis.
3. S
pleenomegaly in 50% of cases.
Investigation
1. CBP increase in atypical lymphocytes
(mononuclear cells).
2. Positive Paul-Bunnell and monospot tests.
Treatment
Is non specific
1. Antipyretics & analgesics.
2. Antibiotics play no role in treatment and
ampicillin based antibiotics should be avoided
as it will cause a skin rash.
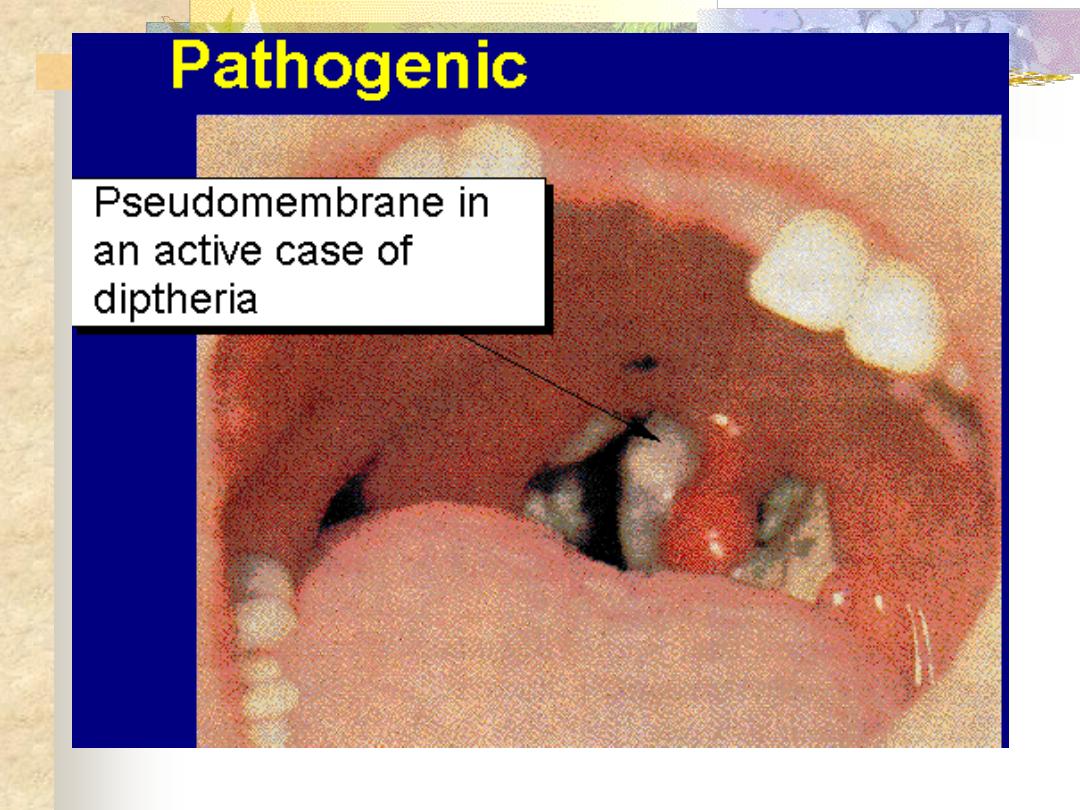
Is
a
specific
infection
by
Corynebacterium diphtheriae which is
disseminated by droplets and coughing.
Children are mostly affected with a
mortality of 10%.
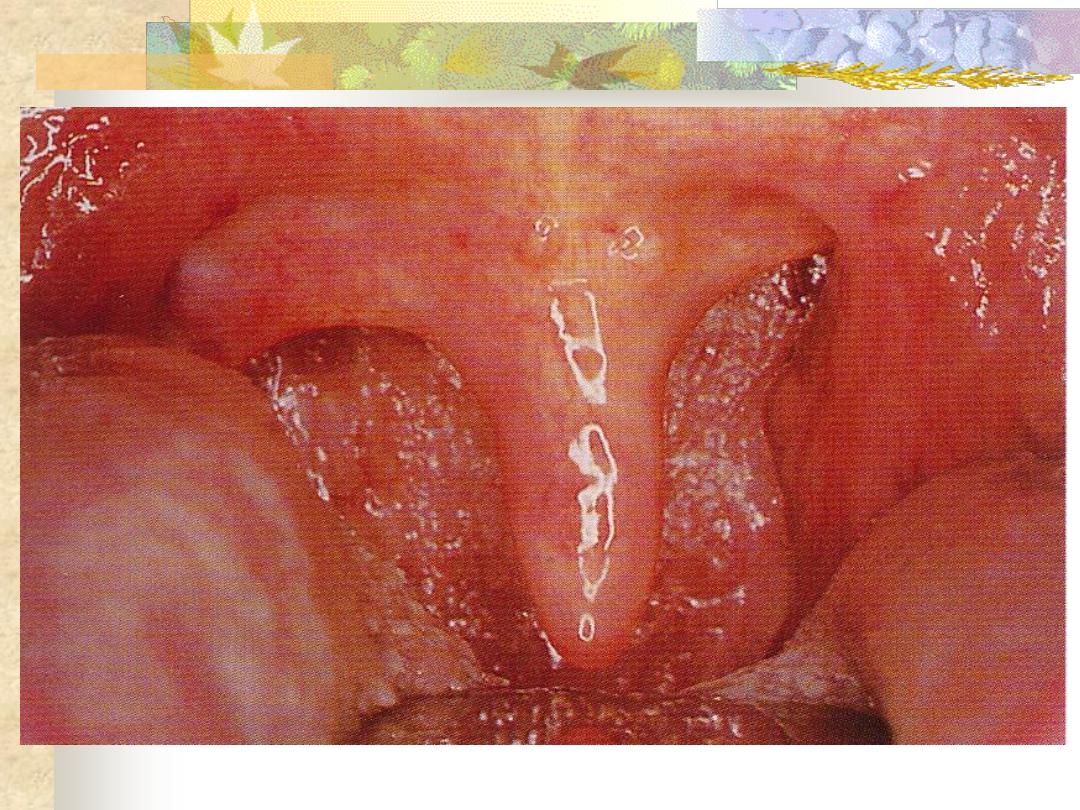
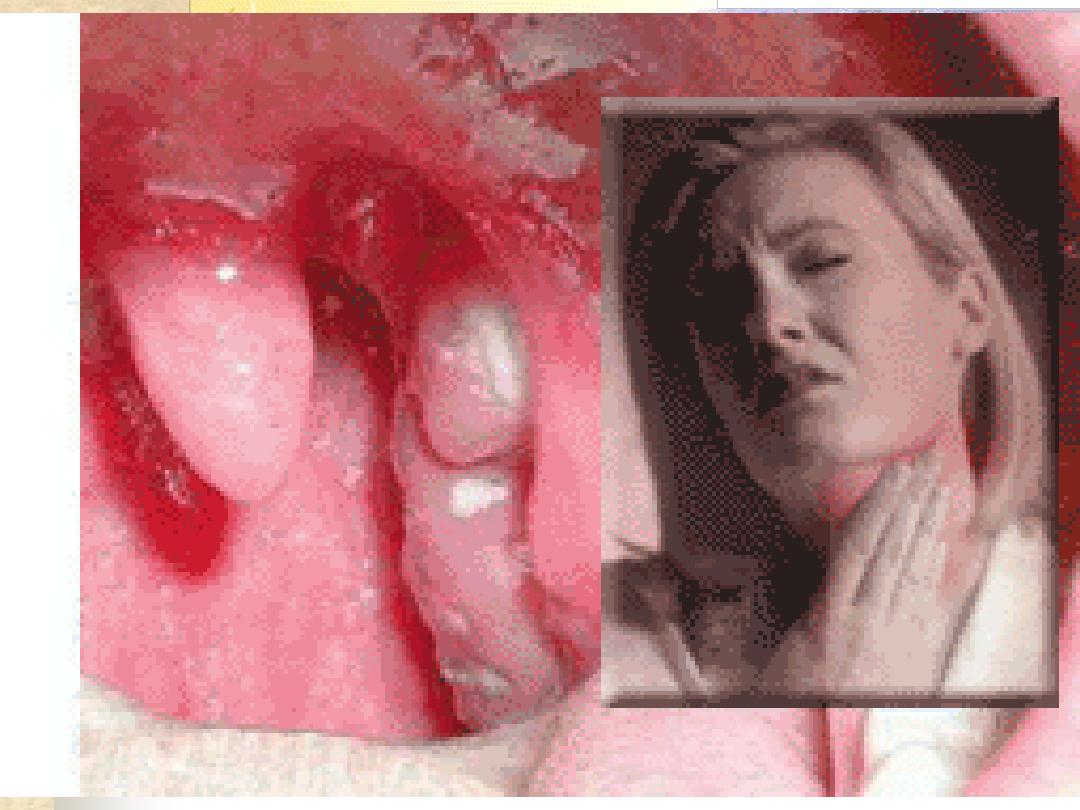
Clinical picture
The disease has incubation period of 4
days. The patient is severely ill, although
the temperature seldom rises above 38
o
C.
The presenting symptoms are sore throat,
odynophagia, dysphonia and breathing
difficulty.
On examination
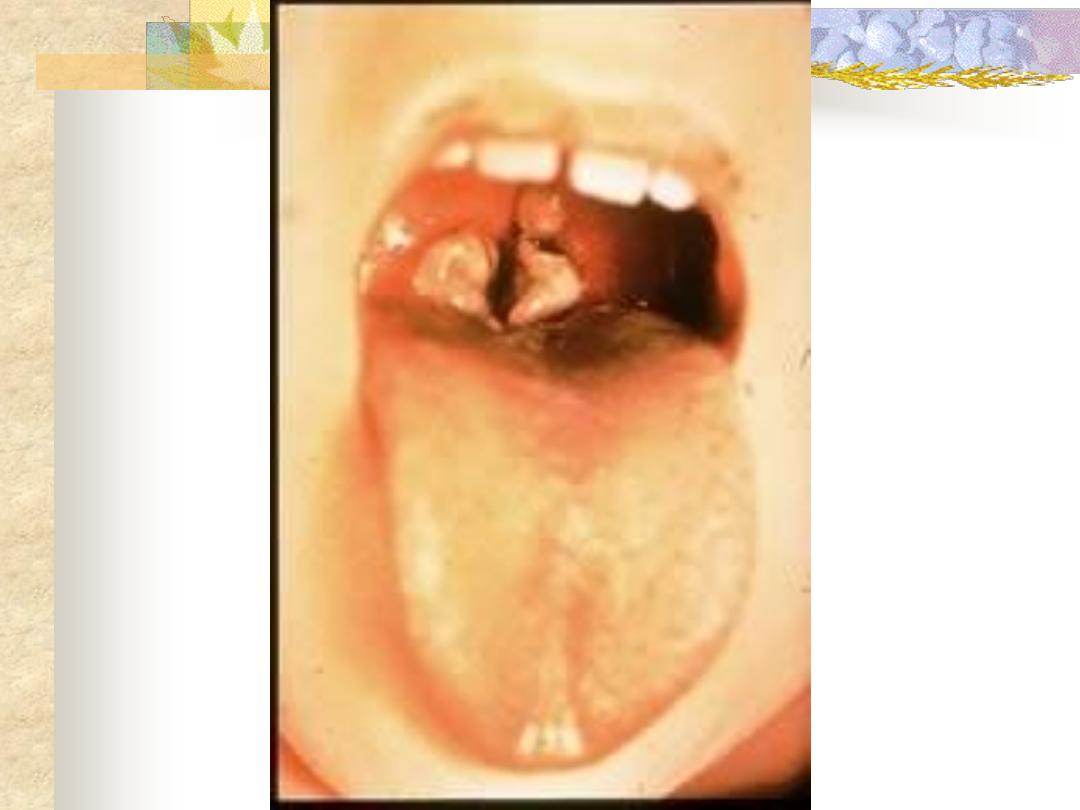
-The disease is characterized by the appearance
of a false membrane on the tonsils, soft palate
and posterior pharyngeal wall. The disease
may spread to affect the nasal cavities and
nasopharynx. The membrane is usually grey
in colour, firmly attached to the mucosa and
leaves a bleeding surface when it's removed.
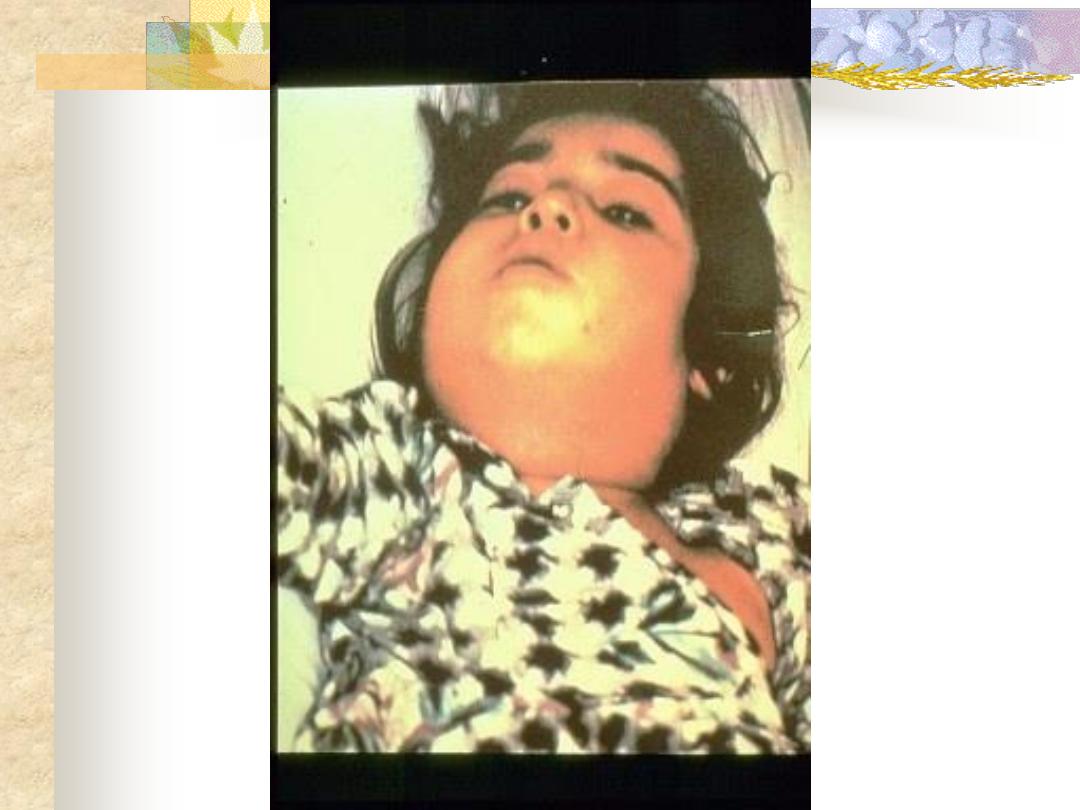
-Tender and enlarged cervical lymphnodes (Bull
neck) appearance.
Investigation
Swab for bacteriological examination including
part of the membrane.
Complications
-Laryngeal
obstruction
and
stridor
tracheostomy.
-Myocarditis
and
neuritis.
The
exotoxin
produced by the microorganism is toxic to
the heart and nerves. Neuritis is in form of
paralysis of soft palate and ocular muscles.
Treatment
-
Antitoxin: intravenous 20,000-100,000 units
depending on the severity of the infection.
-Systemic I.V. penicillin. Erythromycin is used
in penicillin sensitive individuals.
-Tracheostomy or endotracheal intubation should
be considered in the event of airway
obstruction.
- All are true in relation to mouth ulcers
except:
A/ Persistant aphthus ulceration occurs in aids.
B/ Ulcers of the mouth and genitalia with uveitis
characterize Vincents angina.
C/ Vincents angina is caused by infection with
spirochaete Borrelia vincenti and Bacillus
fusiformis.
D/ Local steroids are used in the treatment of
aphthus ulceration.
In patients with membranous pharyngitis:
a)
The appearance of cutaneous rash is
suggestive of Vincent's angina.
b)
Patechial hemorrhage in the palate is
suggestive of Vincent's angina.
c)
Diphtheria is characterized by grey membrane
that leaves bleeding points when removed.
d)
Monospot test is necessary to exclude
agranulocytosis.
e)
Erythematous rash with strawberry tongue is
caused by Epistein Barr Virus.
Characteristic cell of complete blood picture
in infectious mononucleosis is:
a. Atypical lymphocyte (Large mononuclear
cell).
b. Eosinophils.
c. Basophils.
d. Neutrophils.
e. Agranulocytois.
Ludwigs angina may be secondary to all
:
EXCEPT
a. Tonsillar infection
b. Infection of the lower molars and premolars.
c. Infection of upper molar.
d. submandibular gland infection.
MCQ
54 Y F. housewife , DM
Had dental S/ before 5 days
Presented w. fever, dysphagia,
and “ neck swelling”
1)
What is your Dx?
2)
What complication
occurred?
3)
Why?


