1
) ﻋﺪد اﻻوراق
16
(
ﻋﯿﻮن
17
/
1
1
/
2019
.د
ﻋﺰام
Lec: 6
Cornea- II
Objectives:
1 To discuss herpetic eye diseases and sketch a differential
diagrams.
2 To discuss Acanthamoeba and fungal keratitis.
3 To diagnose keratoconus case and role-play lines of
management.
4 To define corneal injury and establish lines of management.
Out-lines:
1- Acanthamoeba keratitis
2-Herpetic eye diseases:
A – Herpes simplex
B – Herpes zoster
3 Acanthamoeba and fungal keratitis
4 Keratoconus.
5 Corneal injuries.
Acanthamoeba keratitis:
• History:
Contact lens use or agricultural
trauma.
• Exam:
The ulcer appears very similar to
Herpes simplex keratitis with
epithelial irregularity as well as ring-
shaped and perineural infiltrates. But
2
,in contrast to herpes simplex, the pain level is out of proportion to
the physical exam findings.
Those patients are exquisitely light sensitive.
• Diagnosis:
1 Culture.
2 Confocal microscopy.
3 Direct smears.
4 Polymerase chain reaction.
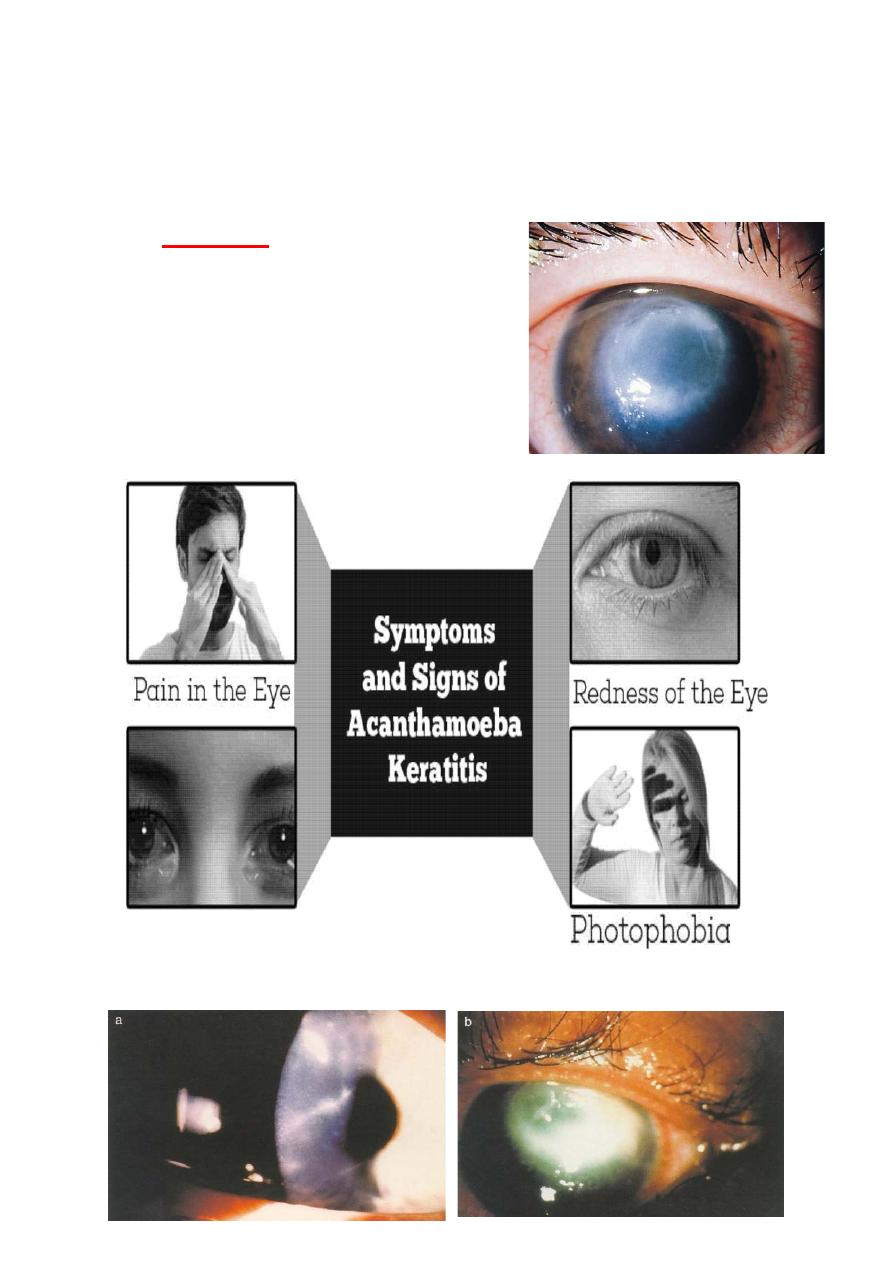
Acanthamoeba keratitis
Watering of Eyes
3
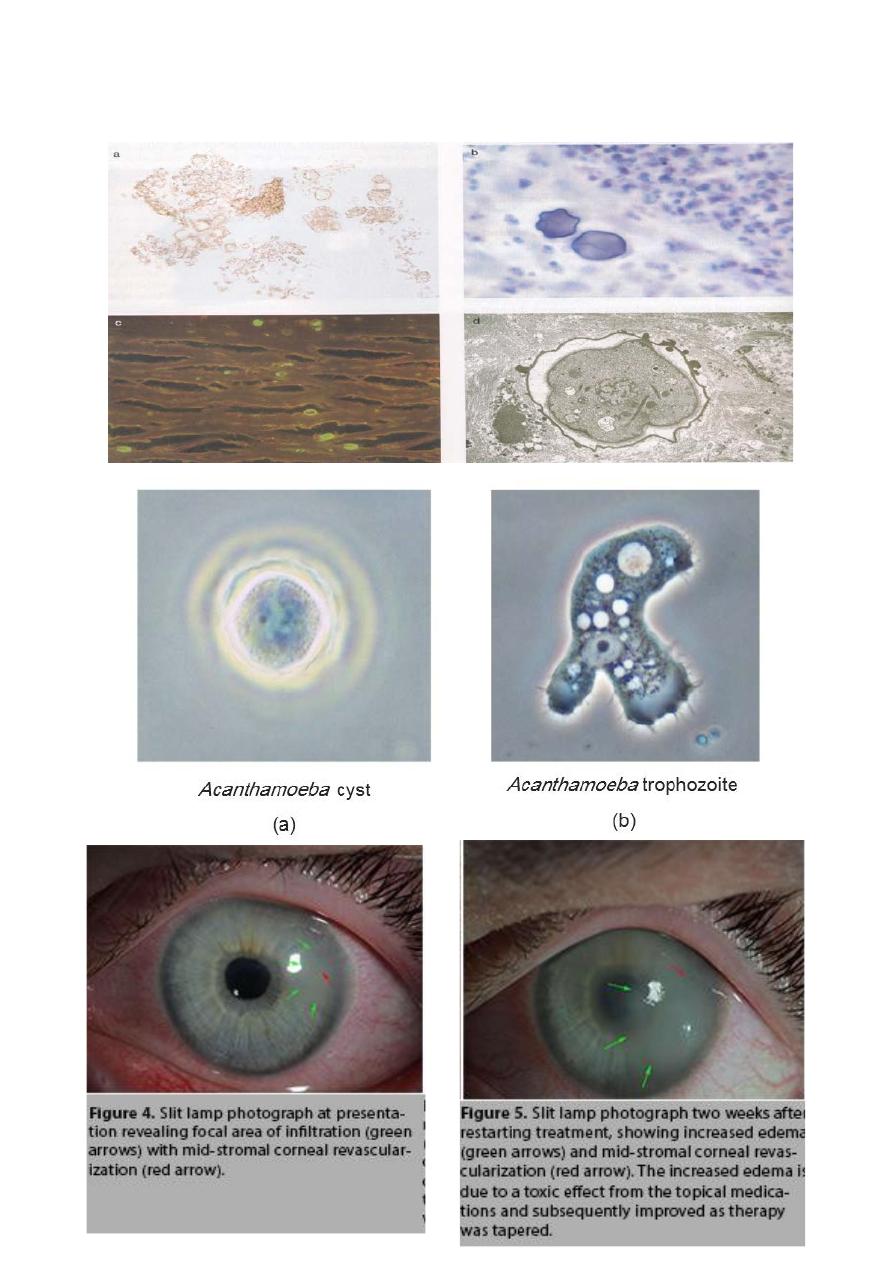
Pathology:
4
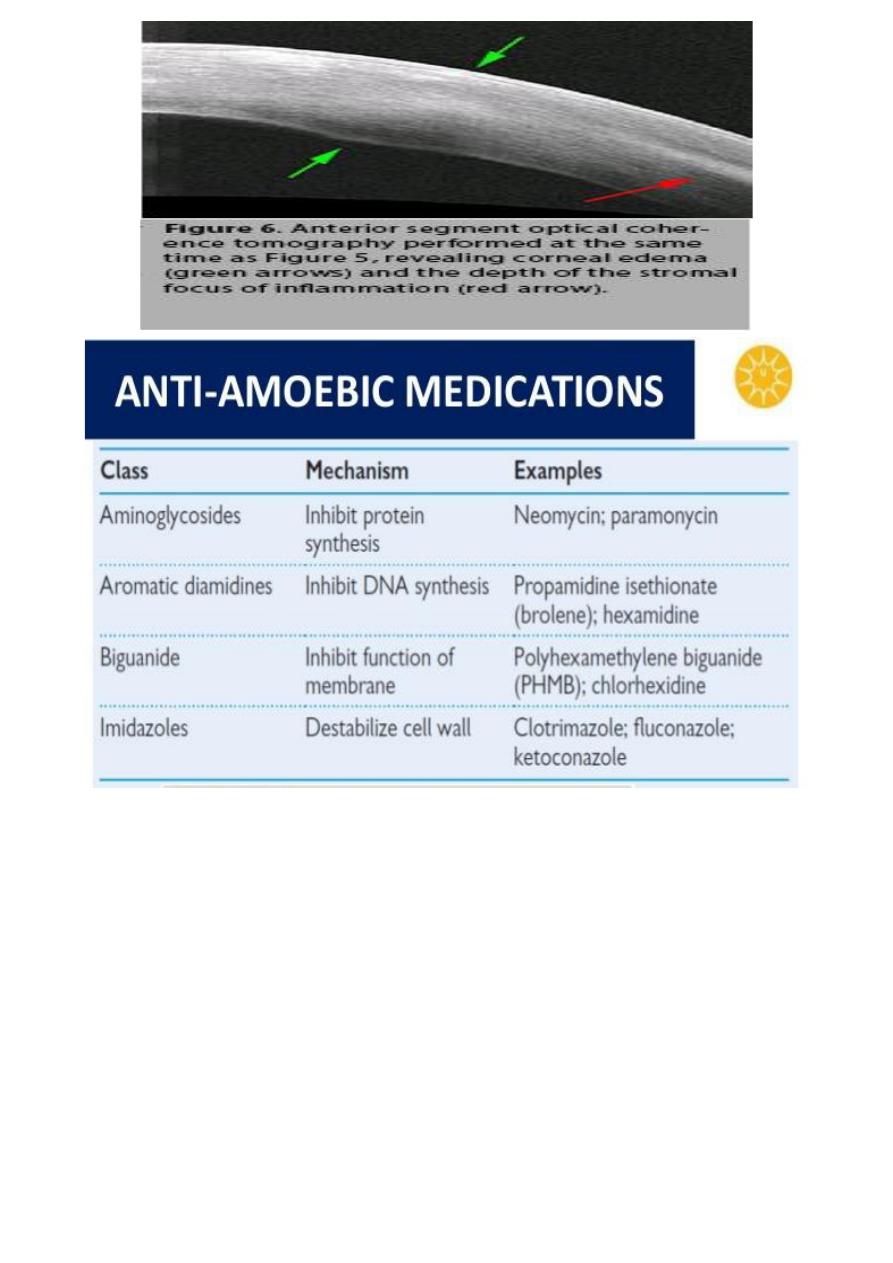
Treatment:
• The organisms are difficult to eradicate, requiring
medication anywhere from three months to a year.
• Even many patients go on to need a corneal transplant
either to control the infection or for visual recovery.
5
Herpes simplex keratitis:
Virology:
Pathogenesis:
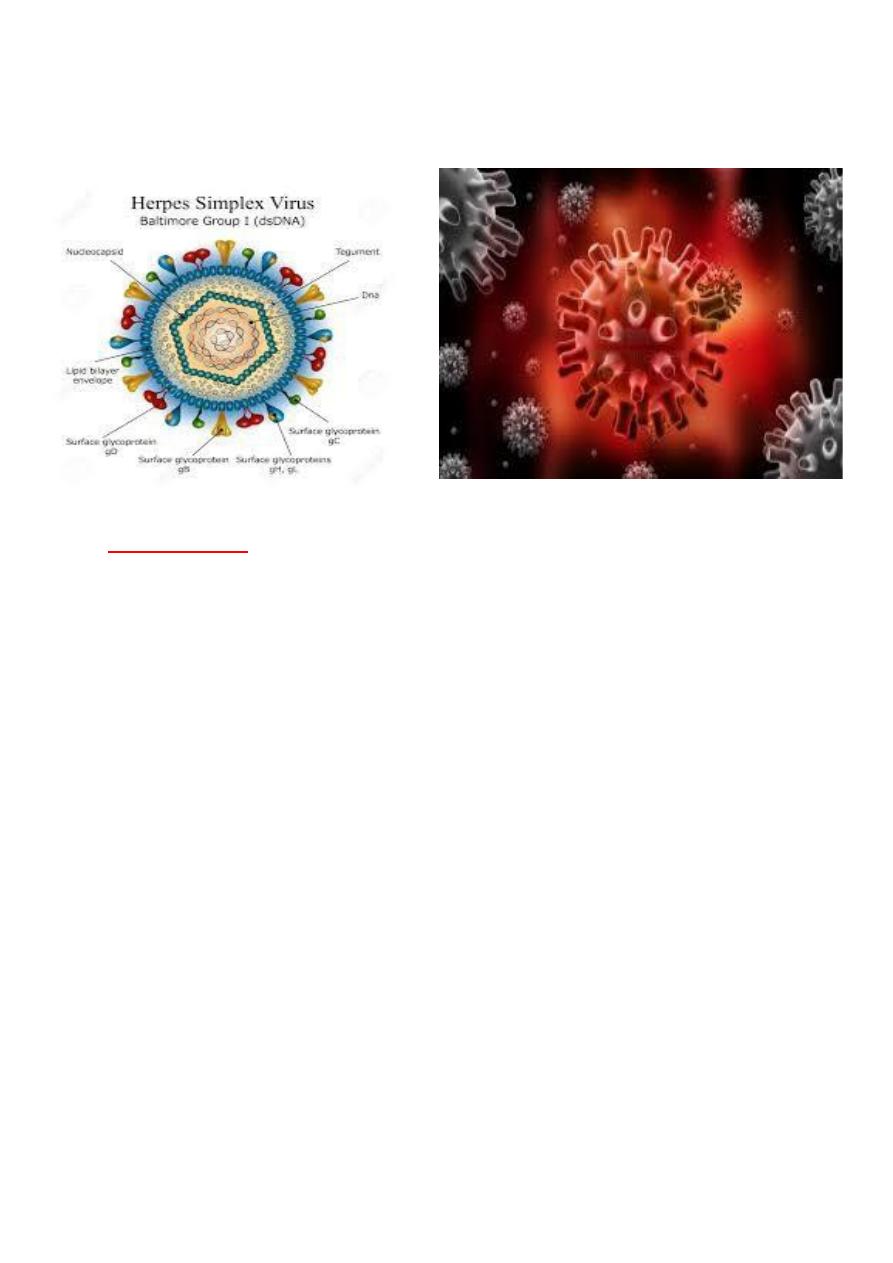
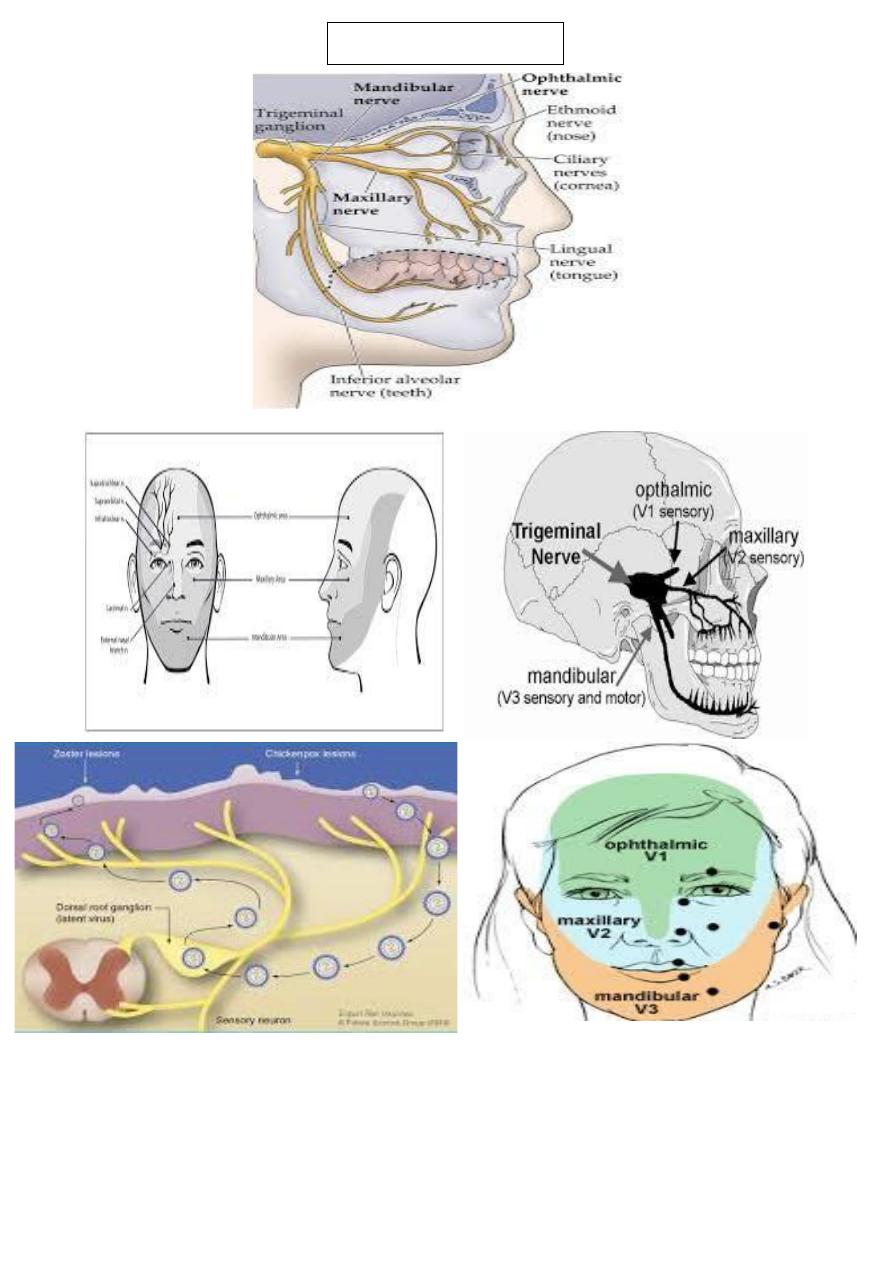
Herpes Simplex Virus (HSV) is an enveloped virus with a cuboidal
capsule and double-stranded DNA genome. HSV-1 primarily causes
infections above the waist that may affect the face, lips, and eyes
whereas HSV-2 causes venereally acquired infection (genital herpes).
Rarely, HSV-2 may be transmitted to the eye through infected
secretions, either venereally or at birth (ophthalmia neonatorum).
HSV transmission facilitated in conditions of crowding and poor
hygiene.
Primary infection usually occurs by droplet transmission, or by direct
inoculation. Due to protection bestowed by maternal antibodies, it is
uncommon during the first six months of life. Children may develop
blepharoconjunctivitis, which is usually benign and self-limited.
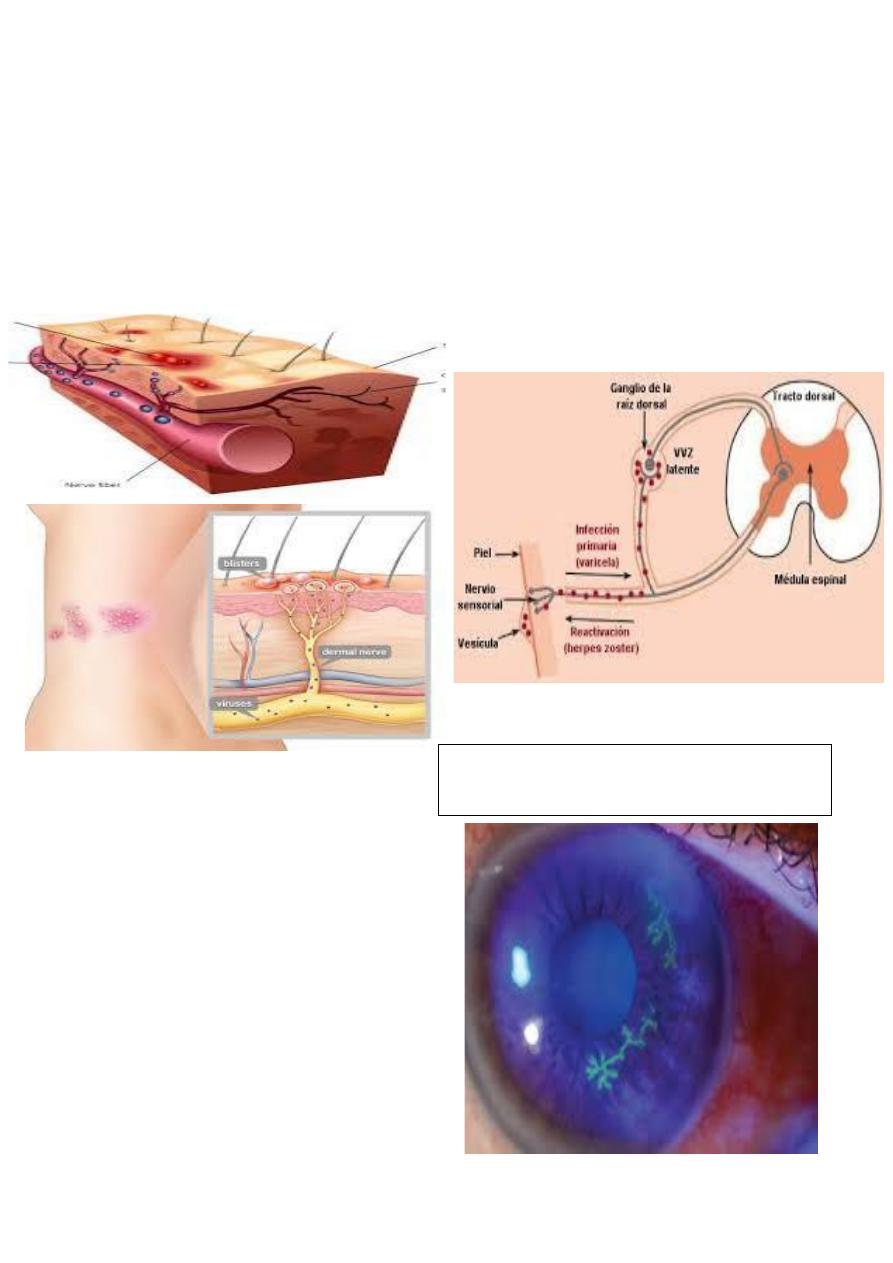
After primary infection, the virus is carried to the sensory ganglia for
that dermatome (e.g. trigeminal ganglion), where a latent infection is
established. Stimuli such as fever, hormonal changes, ultraviolet
radiation, trauma and trigeminal injury may cause a clinical
reactivation, when the virus replicates and is transported in the
sensory axons to the periphery, where there is recurrent disease.
6
After primary infection, the virus is carried to the sensory ganglia for
that dermatome (e.g. trigeminal ganglion), where a latent infection is
established. Stimuli such as fever, hormonal changes, ultraviolet
radiation, trauma and trigeminal injury may cause a clinical
reactivation, when the virus replicates and is transported in the
sensory axons to the periphery, where there is recurrent disease.
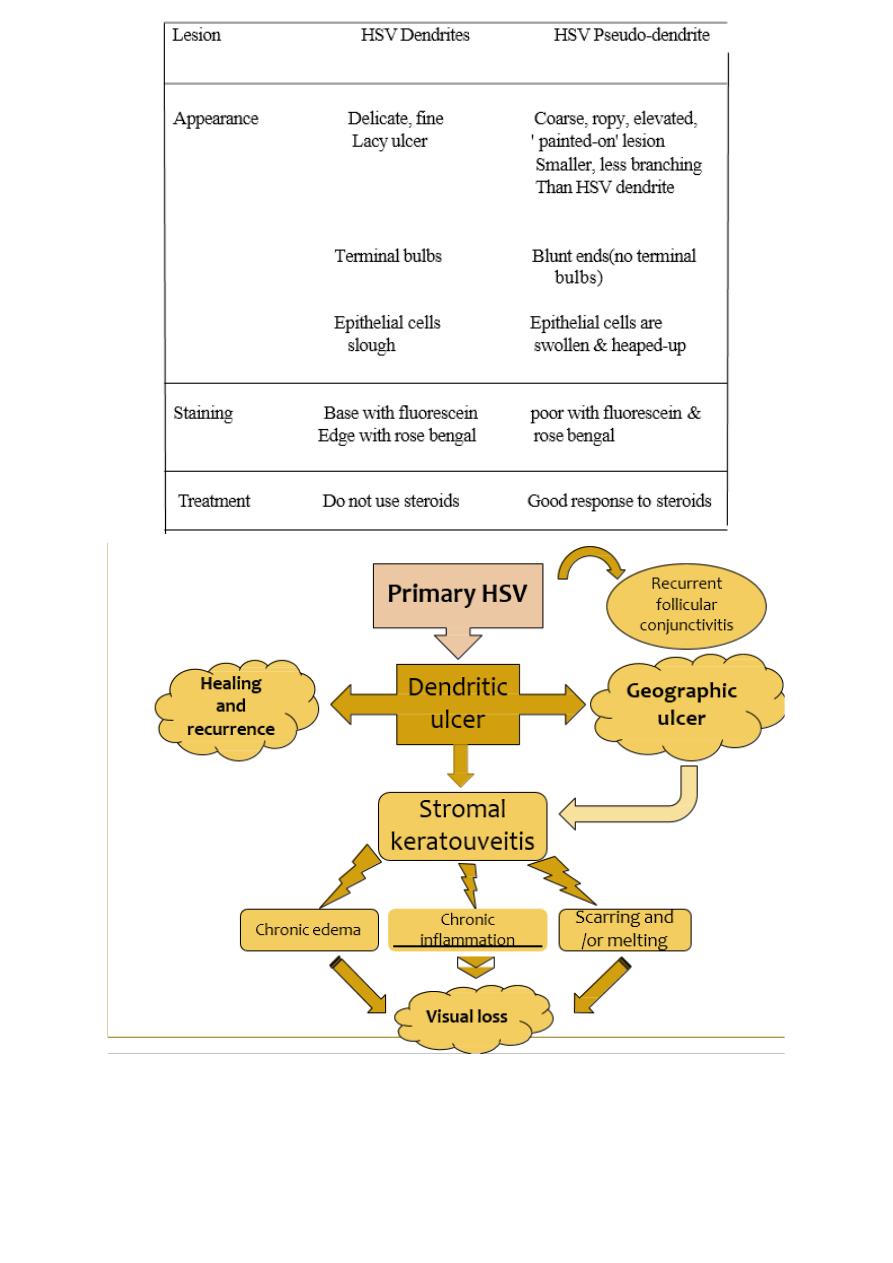
Herpetic epithelial keratitis:
Presentation: may be at any age,
with
mild discomfort, watering and
blurred vision.
Signs:
Opaque epithelial cells arranged in
a
course punctuate or stellate pattern.
HSV dendrites with fluorescein stain
7
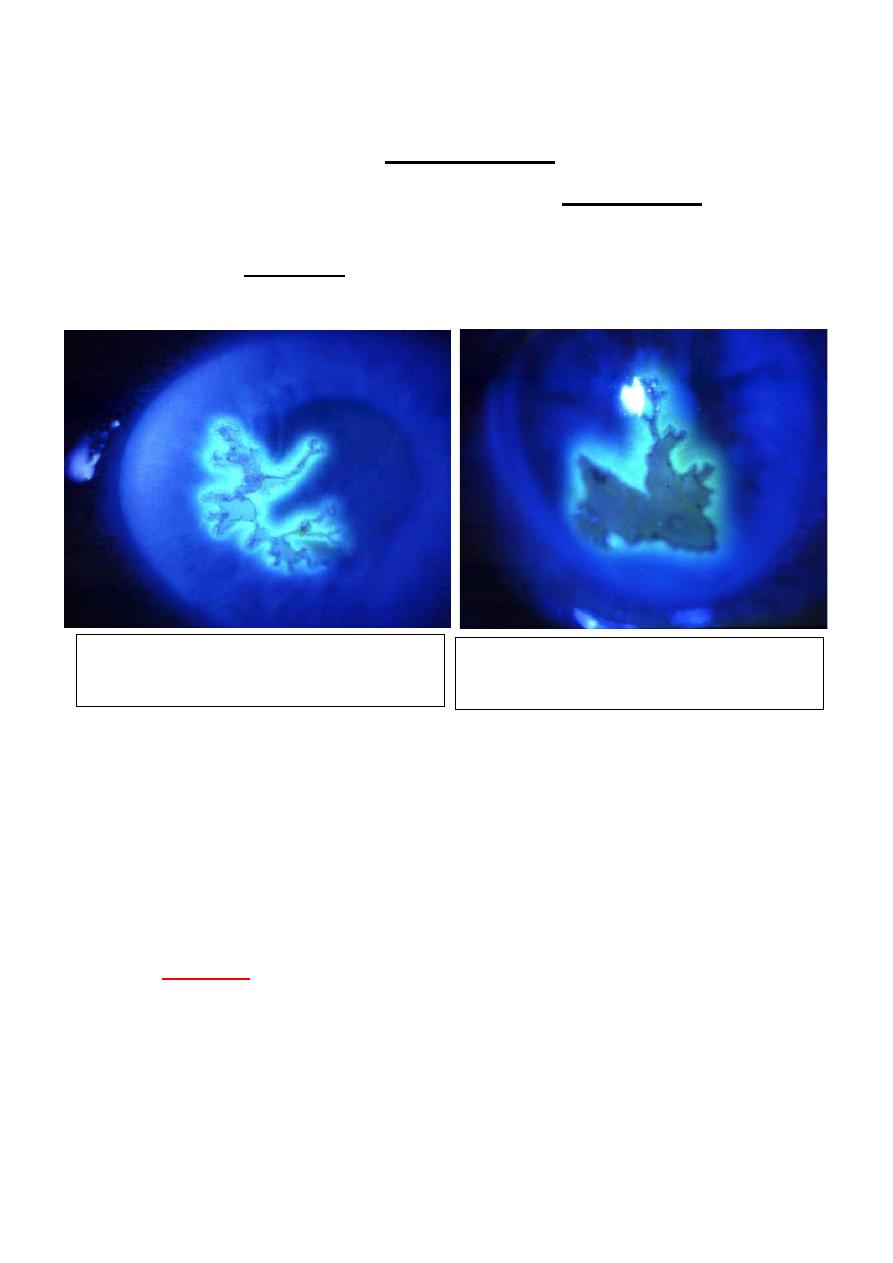
1 Central desquamation results in a linear-branching (dendritic)
ulcer, most frequently located centrally.
2 The ends of the ulcer have characteristic terminal bud and the
bed of the ulcer stains well with fluorescein.
3 Corneal sensation is reduced.
Herpes simplex epithelial keratitis:
Treatment:
• Acyclovir 3% ointment x 5 daily
• Trifluorothymidine 1% drops 2-hourly
• Debridement if non-compliant
Topical steroid treatment may allow progressive enlargement of the
ulcer to geographic or “amoeboid" configuration.
•
Culture:
can be taken by debridement of the ulcer. This relies
on cytopathic effect in tissue culture, which can be used to
distinguish HSV-1 from HSV-2
• PCR is also available.
• Topical antiviral agents most frequently used are
trifluorothymidine, acyclovir and vidarabine. Acyclovir 3%
Dendritic ulcer with terminal bulb Stains
with fluorescein
Mayenlargetobecome geographic

8
ointment is used five times daily, it acts preferentially on virus
laden epithelial cells.
• Acyclovir penetrates intact corneal epithelium and stroma,
achieving therapeutic level in the aqueous humor. Therefore, be
used to treat stromal herpetic keratitis.
• Debridement may be used for dendritic but not geographic
ulcers. The corneal surface is wiped with sterile cellulose
sponge. An antiviral agent must be used in conjunction to
prevent recurrence.
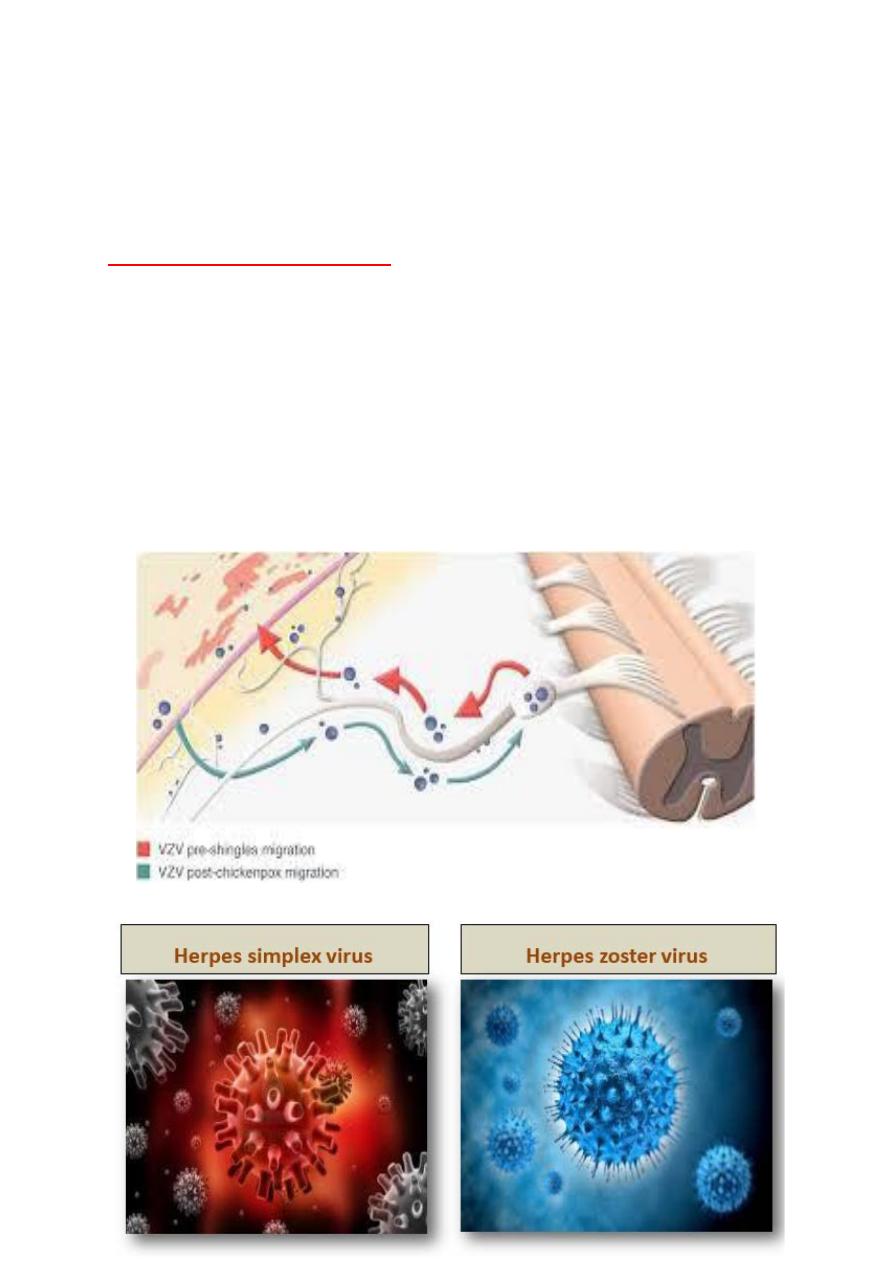
Herpes zoster Ophthalmicus:
Pathogenesis:
• The varicella-zoster virus ( VZV) causes chickenpox (varicella)
and shingle
herpes zoster).
• VZV and HSV belong to the same subfamily of herpes virus
group and are
morphologically identical but antigenically different.
9
After the initial attack of chickenpox, the virus travels in a retrograde
manner to the dorsal root and cranial nerve sensory ganglia, where it
can remain dormant for decades. From there, it can reactivate after
VZV-specific cellular immunity has faded, to cause shingles.
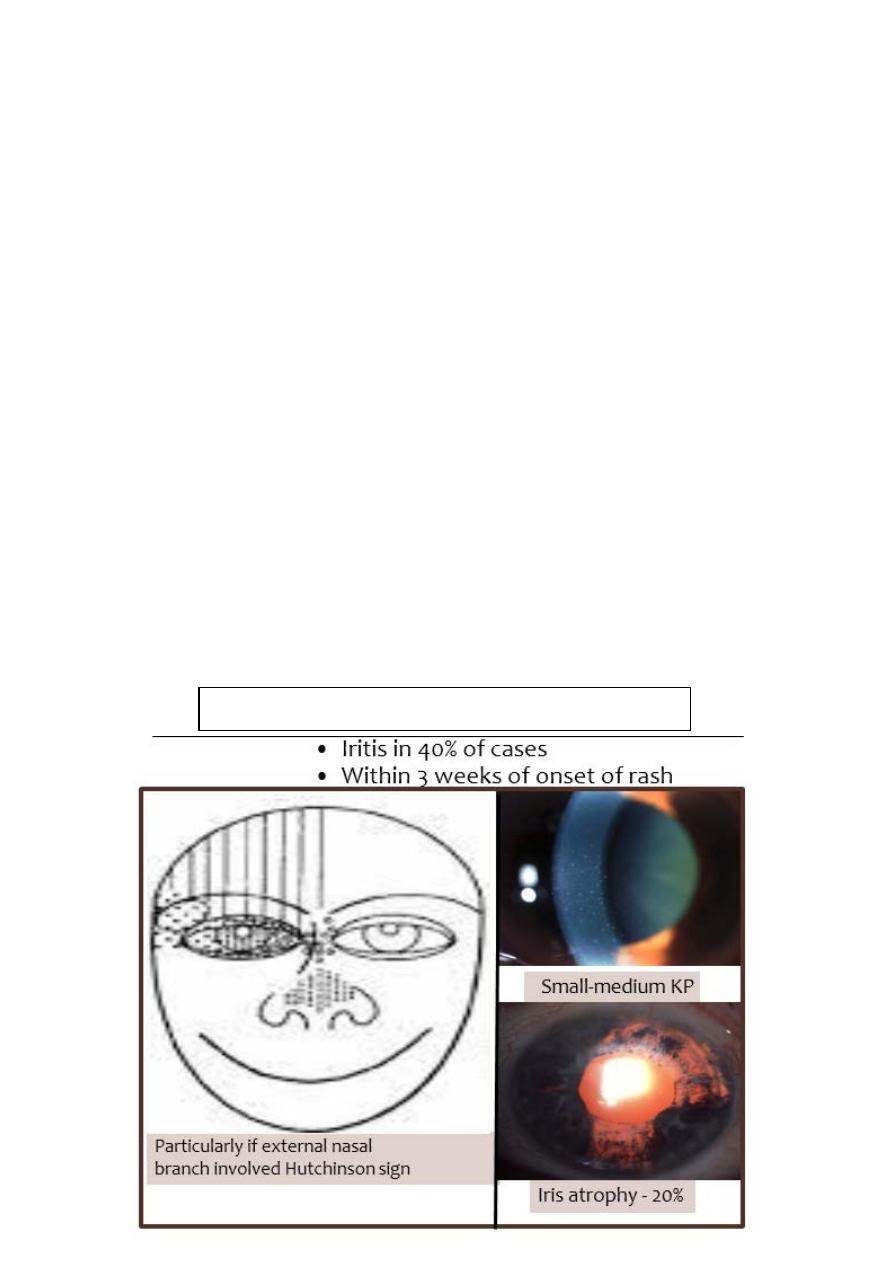
Risk of ocular involvement:
Involvement of the external nasal nerve (Hutchinson Sign), which
supplies the side of the tip, the side and root of the nose correlate
significantly with subsequent development of ocular inflammation
and corneal denervation because it is the terminal branch of the
nasociliary nerve.
Herpes Zoster Ophthalmicus (HZO) occur most frequently in the
sixth and seventh decades. In the elderly, the signs and symptoms are
more sever and lasts longer. Patients with AIDS also tend to have
more sever disease.
Morphology:
10
Pathogenesis
11
Herpes zoster Ophthalmicus
Acute Systemic Disease:
Clinical Features
• A prodromal phase: lasting 3-5 days with tiredness, fever,
malaise and headache precedes the appearance of the rash.
• Skin lesions appears initially as a painful erythema with a
maculo-papular rash. Within 24 hours, groups of vesicles
appears and those become confluent over two-four days.
• The vesicle often pass through a pastular phase before they crust
and dry after 2-3 weeks. New crops of vesicles may appear in
immunodeficient patients.
• The rash has a dermatomal distribution and respect the midline,
although inflammatory edema may cross the midline and give
rise to the impression of bilateral involvement. Skin lesion may
leave extensive tissue destruction and depigmented scar. The
development of shingles in children or young adults (<50 years)
should prompt a search for immunodeficiency or malignancy.
HIV infection should excluded.
12
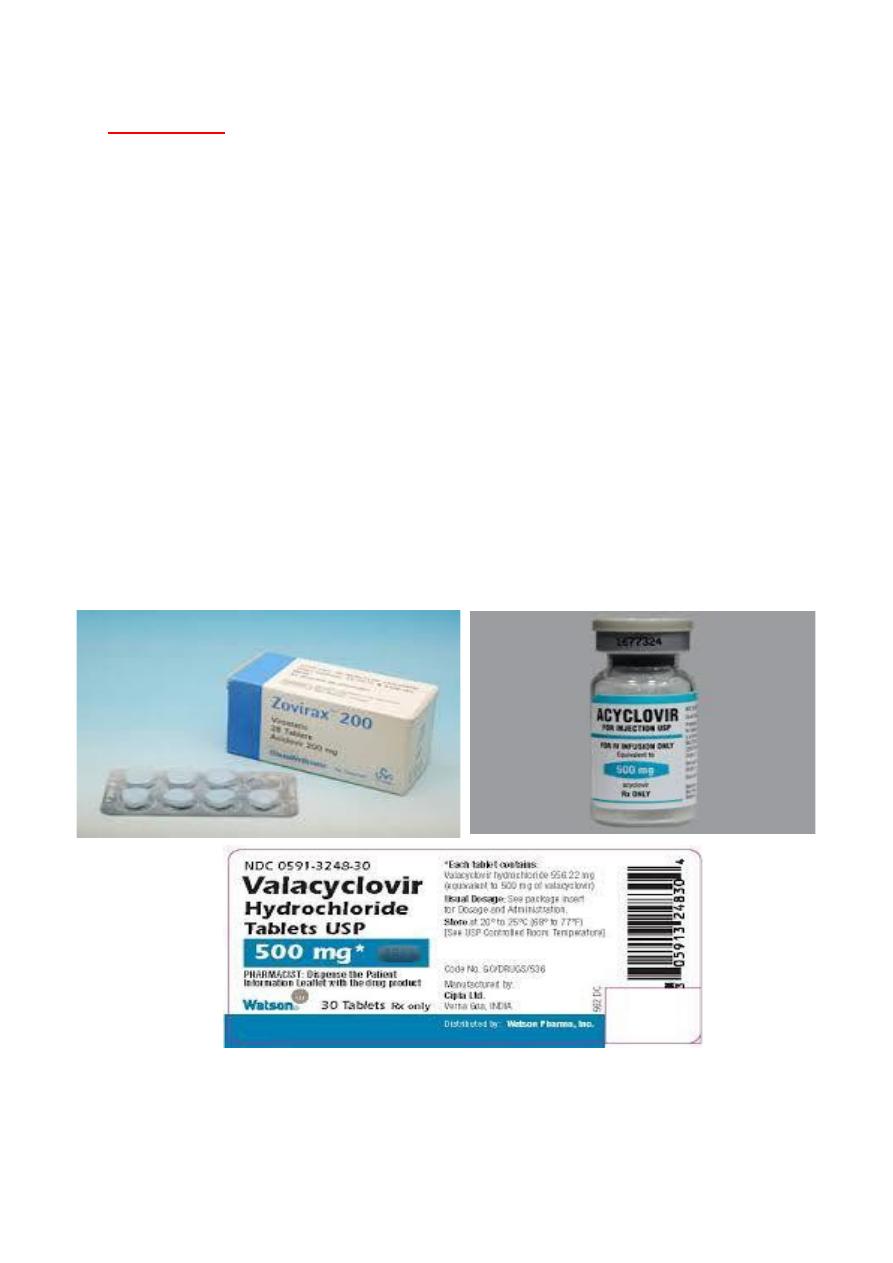
Treatment:
Oral Acyclovir (800 mg five times daily for 3-7 days given within 72
hours of onset) is the treatment of choice.
Patients presenting with new vesicles after 72 hours should also be
treated to reduce the severity of acute HZO and the risk of post-
herpetic neuralgia at six months. Intravenous Acyclovir (5-10 mg/kg
tid.) is only indicated for encephalitis. The duration of treatment
should be extended for the elderly or immunosuppressed patient.
Foscarnet is the drug of choice in acyclovir resistant patients.
Other oral antiviral agents: Valciclovir 1 g tid, and famciclovir 750
mg daily.
Systemic steroids (prednisolone 40-60 mg per day) should be used in
conjunction with systemic antiviral. They have a moderate effect at
reducing acute pain and accelerating skin healing. Symptomatic
treatment of skin lesions is by drying, antisepsis and cold compresses.
13
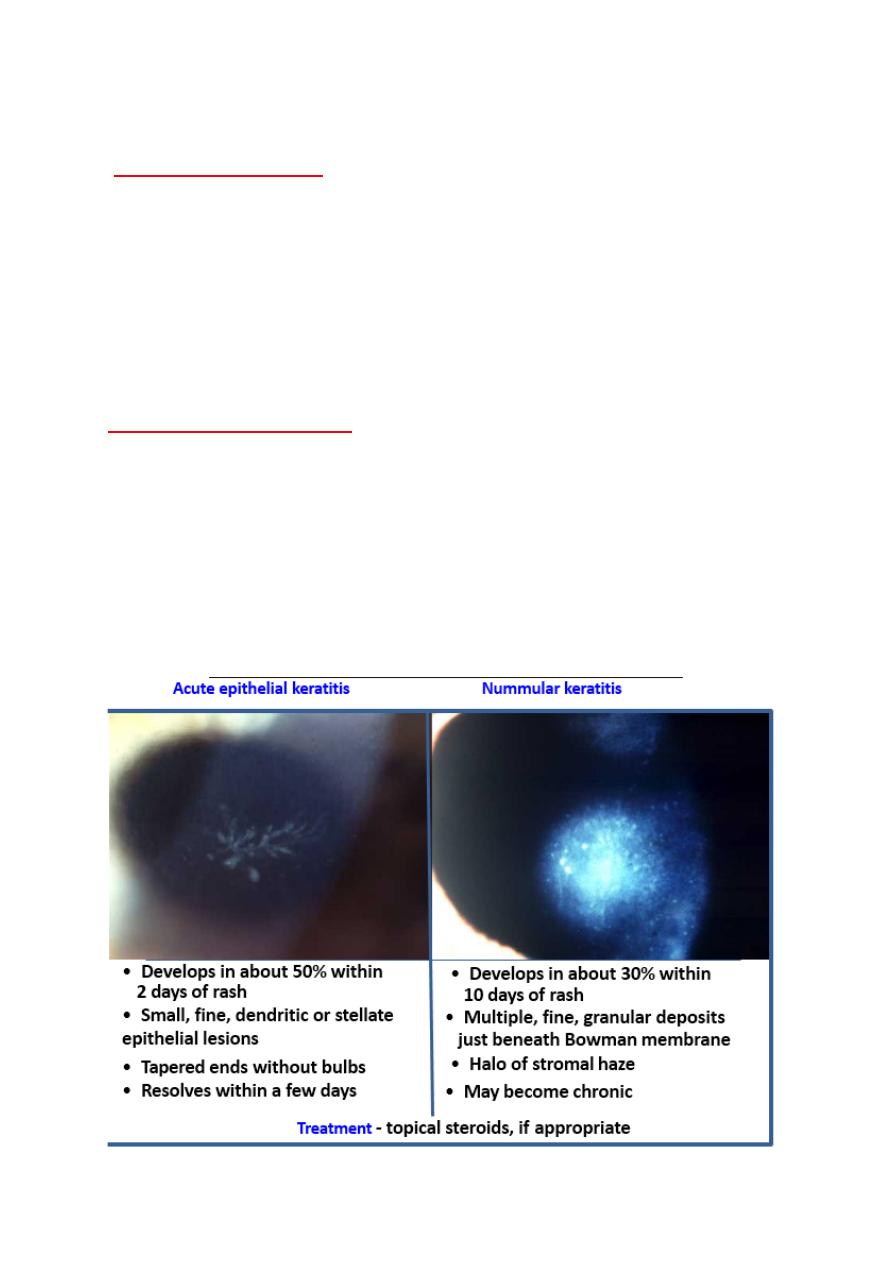
Herpes zoster keratitis:
Acute ocular disease
Acute epithelial keratitis: develops in about 50% of patients within 2
days of onset of rash and resolve spontaneously a few days later. It is
characterized by small, fine dendritic lesions, which in contrast to
herpes simplex dendrites, have tapered ends without terminal buds.
The lesion stain with fluorescein and rose Bengal.
Treatment is with a topical antiviral.
Chronic Ocular Disease
Clinical features
Lid scarring may result in Ptosis, cicatricial entropion, Trichiasis,
madarosis and notching of the lid margin.
Scleritis may become chronic and lead to patchy scleral atrophy.
Neurotrophic keratitis with reduced sensation. It may lead to sever
ulceration, secondary bacterial infection and even perforation.
14
15
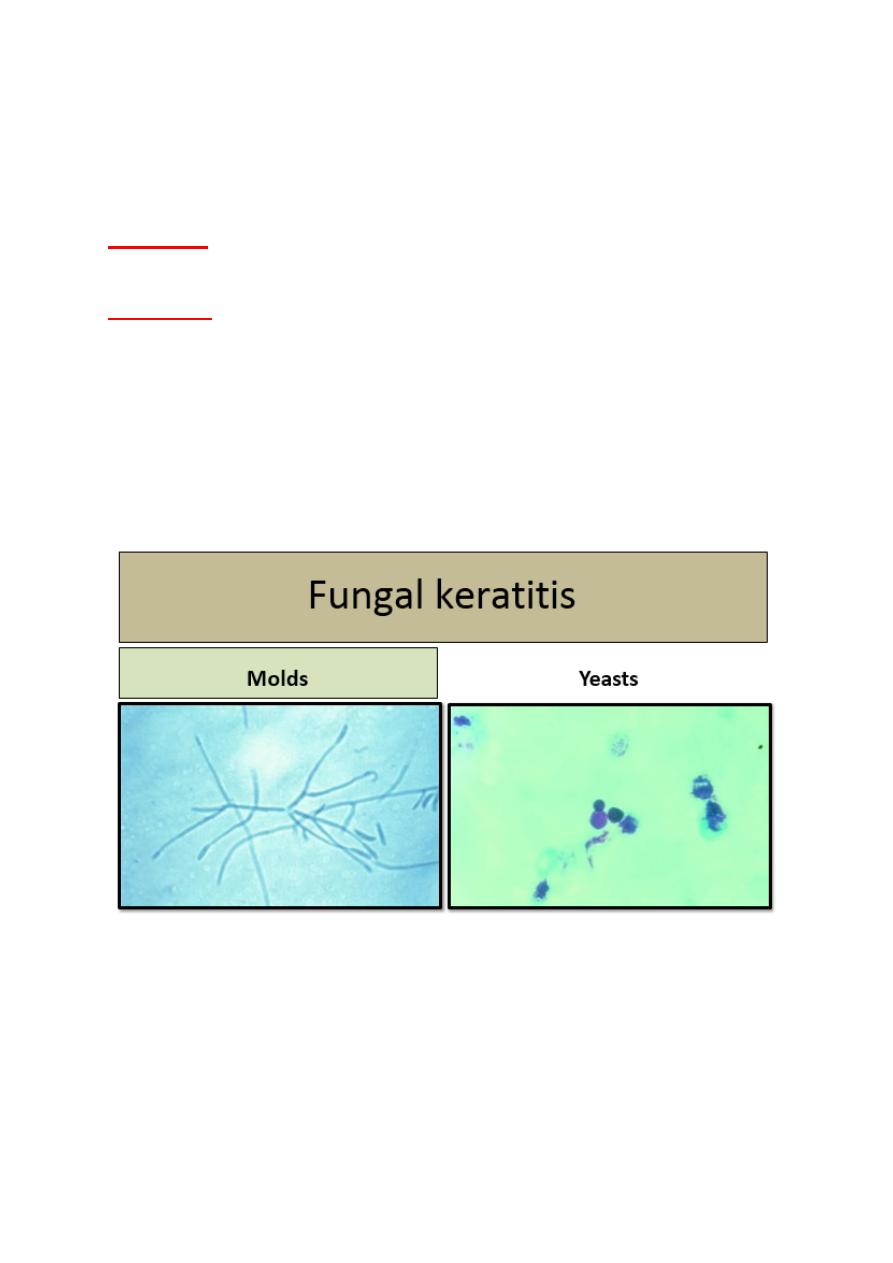
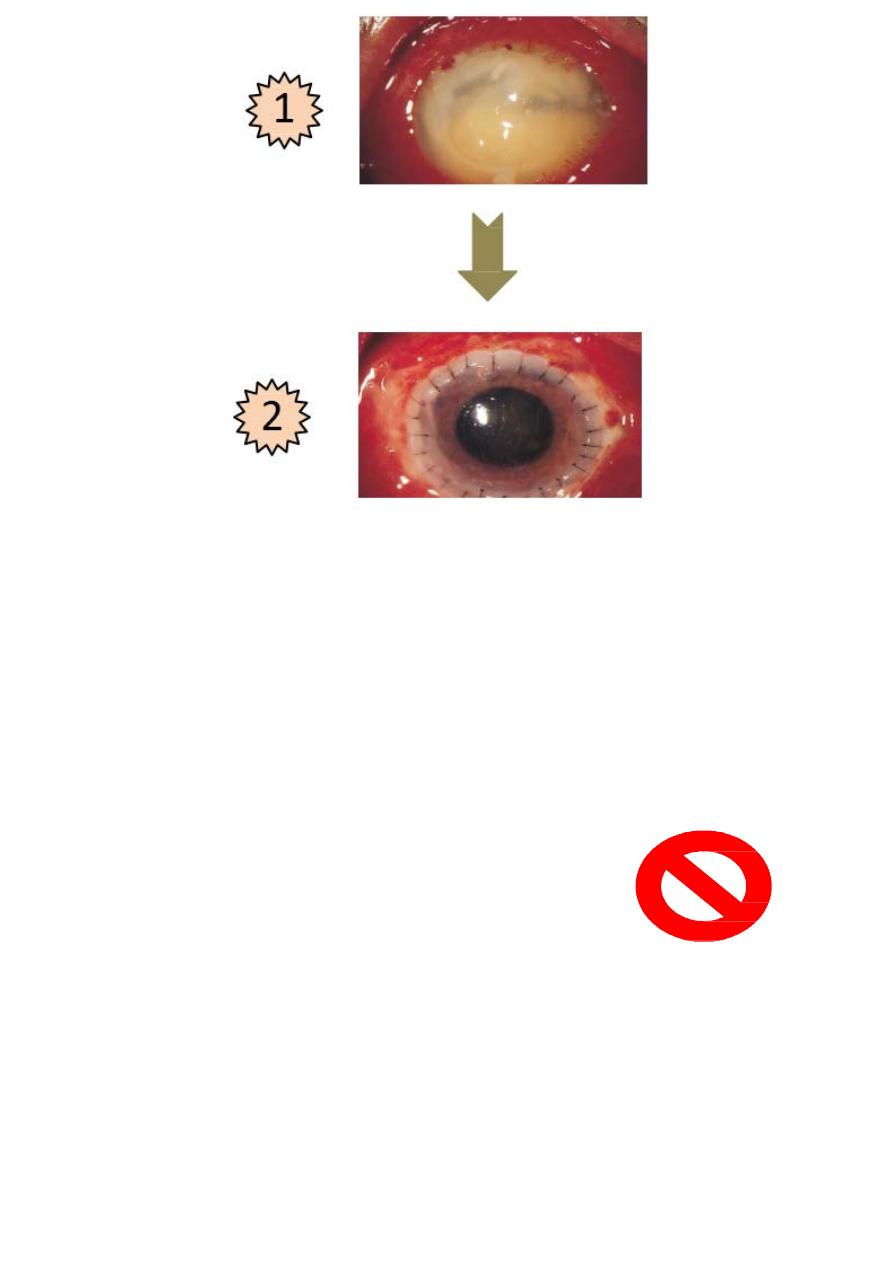
Fungal keratitis:
Fungi are eukaryotes that develop branching filaments. Fungi are
classically divided into 2 groups:
1- Yeasts:
are round or oval fungi that reproduce by budding and
sometimes from pseudohyphae by elongation during budding.
2- Molds:
are multicellular fungi composed of tubular hyphae, either
septate or non-septate, that grow by branching and apical extension.
Dimorphic fungi grow in two forms due to of changes in cell wall
synthesis in different environments. Such fungi may appear as yeast
in the host and as a mold in a room-temperature laboratory.
Dimorphic fungi may be highly virulent pathogens. Fungal cell wall
stain with Gomori methenamine sliver, but except for Candida, do not
take up Gram stain.
16
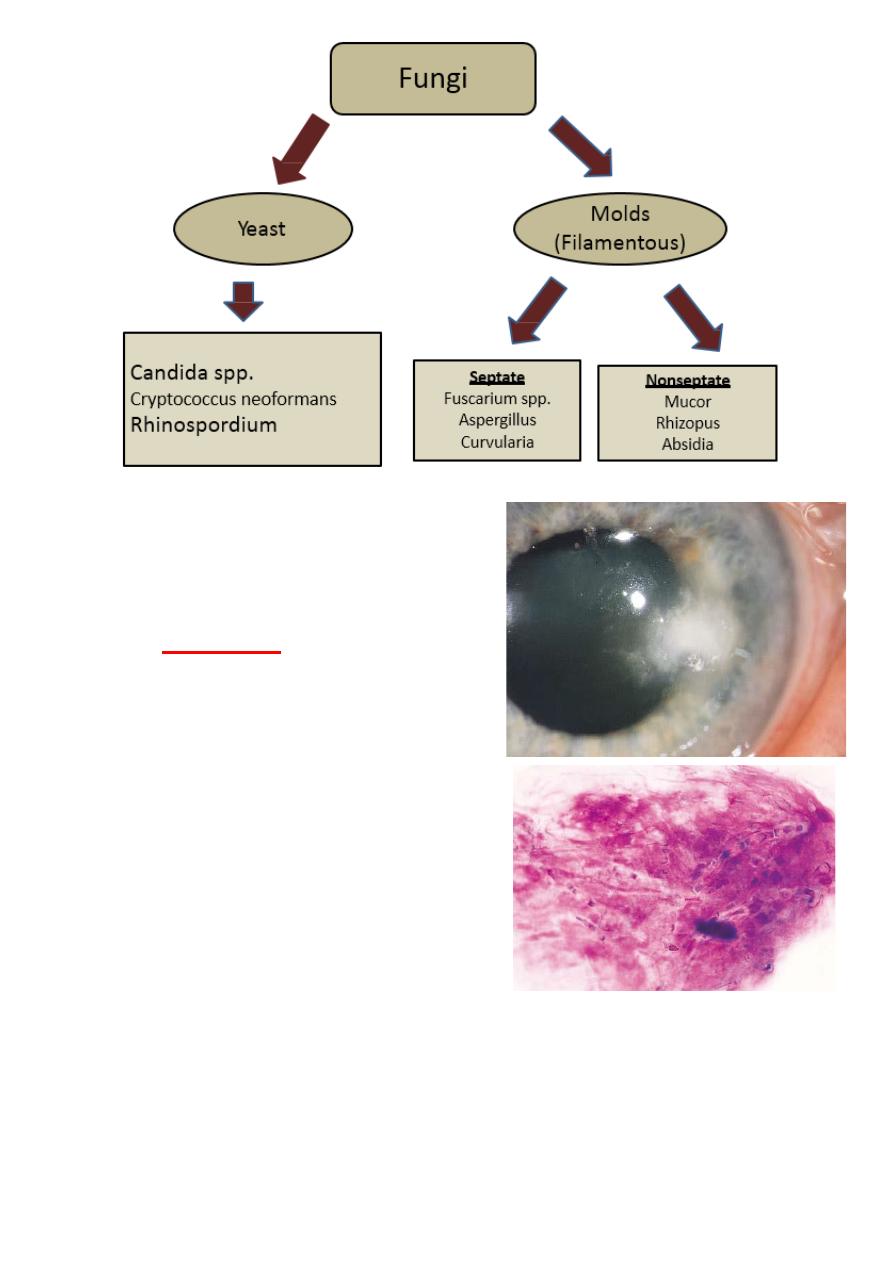
Fungal keratitis:
• It is difficult to diagnose and
needs to be cultured on special
media.
•
With molds,
the ulcer has a dull
gray infiltrate, and satellite
lesions are often present.
• Initially lesion has characteristic
feathery, branching borders in the
cornea.
• Advanced fungal infection may
resemble advanced bacterial
keratitis, which can lead to
misdiagnosis.
• Fungal corneal ulcers are caused
by a wide variety of filamentous organisms after trauma with
vegetable-contaminated matter and by Candida in eye with
preexisting ocular surface disease.
•
Fuscarium
and
Asergillus
are the most commonly isolated
filamentous organisms. Ulcers typically have feathery borders
17
and satellite lesions, and the infiltrate extends beyond the
epithelial defect. Giemsa stained smears and cultures on
appropriate media are necessary to make the diagnosis.
•
Candida
looks similar to bacterial ulcers and are usually not
suspected on the basis of the history or clinical appearance.
• Fungal ulcers are less responsive to medical therapy than
bacterial ulcers. The drug of choice for filamentous infections is
natamycin, but the drug penetration and efficacy are limited.
Amphotericin (0.15%) is the drug of choice for Candida.
• Topical steroids enhance fungal infection and therefore;
contraindicated.
• Penetrating keratoplasty indicated for infection that progress
despite maximal appropriate medical therapy.
• Yeast ulcers, have defined borders and may look similar to
bacterial infections.
• Yeast infections remain
localized, causing relatively
small epithelial ulceration.
• The patient may have both
foreign- body sensation and
light sensitivity, but the eye
won't produce a lot of
discharge because the tissue
isn′t being damaged.
18
A particularly worrisome risk in infection with fungi, particularly
molds, is deep penetration, not only into the cornea but also into the
eye itself. If the infection dose not resolve, medical options are
limited. Because the topical medications do not penetrate deeply.
Trying different delivery methods, like injecting antifungal directly
into the stroma to achieve higher concentrations, is one well-
documented option.
Corneal transplantation should be considered urgently if there is risk
of the infection moving into the eye or adjacent sclera.
The duration
of symptoms can be helpful to the
differential diagnosis.
Bacterial ulcers, for example, have a rapid onset of
symptoms compared with fungal ulcer, which may
takes days to become problematic.
Red flags:
• A major red flag for fungal infection is agricultural trauma with
vegetable matter, in addition, the clinicians maintain a high
19
index of suspicion in the setting of contact lens wear in humid
weather conditions. Usually within the first 48 hours after
initiating the antibiotic therapy.
• When to question the diagnosis?
• Day 1, you do the culture and start a fluoroquinolone.
• Day 2, you expect the patient to feel at least no worse and,
hopefully a little better.
• Day 2,3 and 4, the ulcer should start consolidating and the
appearance of the eye should be noticeably improved.
• You have to reassure the patient that the vision is the last thing
to improve.
• But if you don’t have signs of at least some overall
improvement in 4-7
days, then start considering atypical causes of the keratitis.
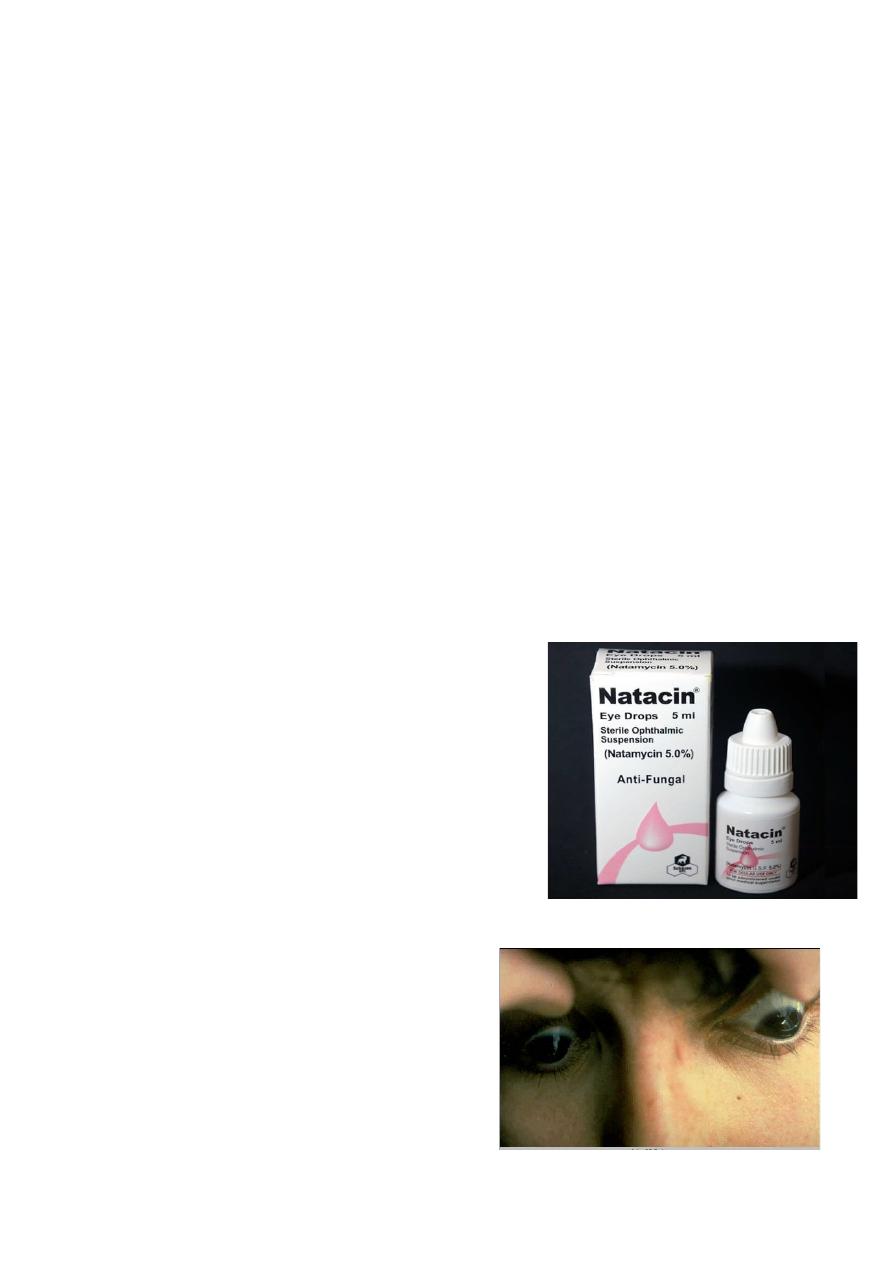
Treatment:
• Only one medication is commercially
available for fungal keratitis:
natamycin, which usually applied
hourly during the day.
•
“Natamycin′s best activity is against
Fusarium mold. It has less efficacy
against candida yeast,
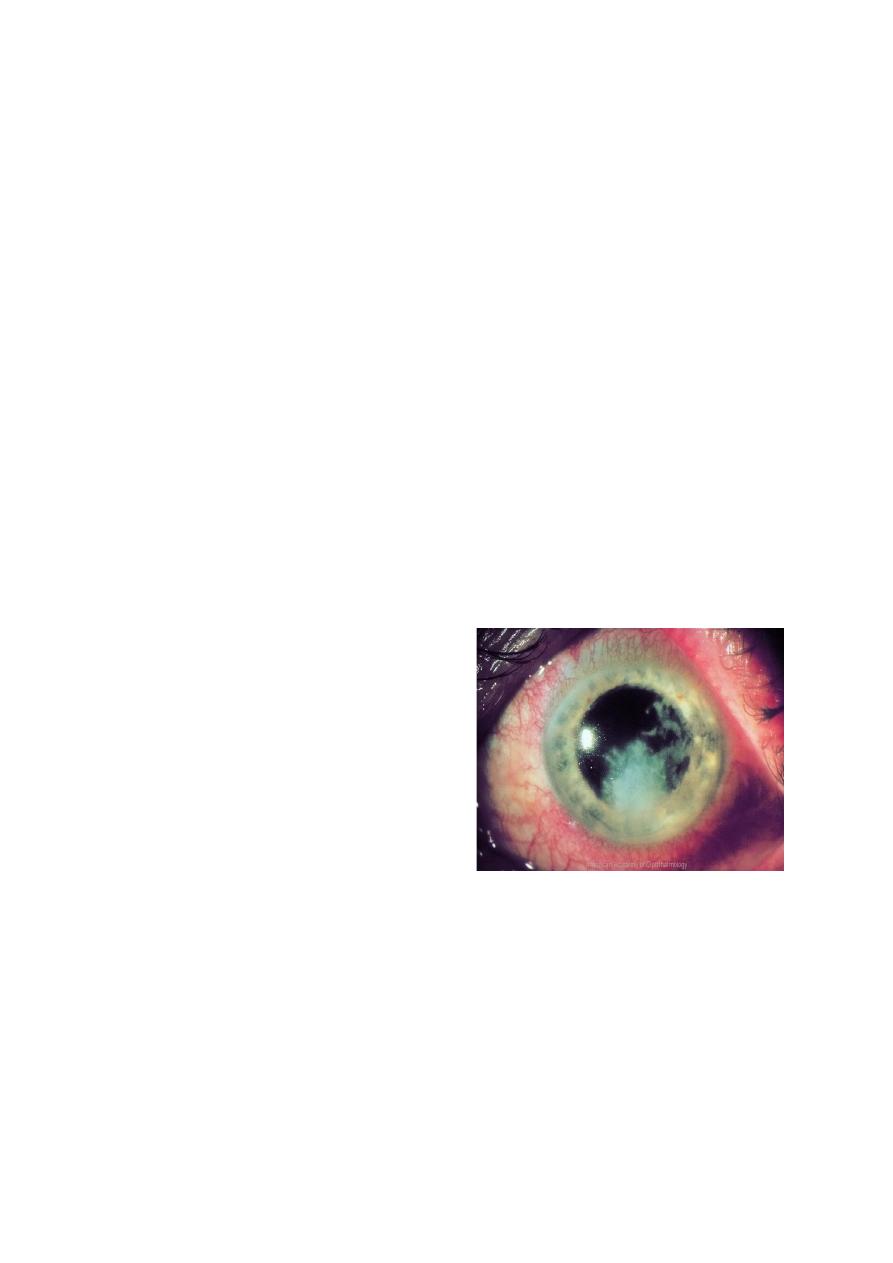
Keratoconus:
Definition
• It is ectatic progressive disorder
in which the cornea assume a
conical shape secondary to
stromal thing and protrusion.
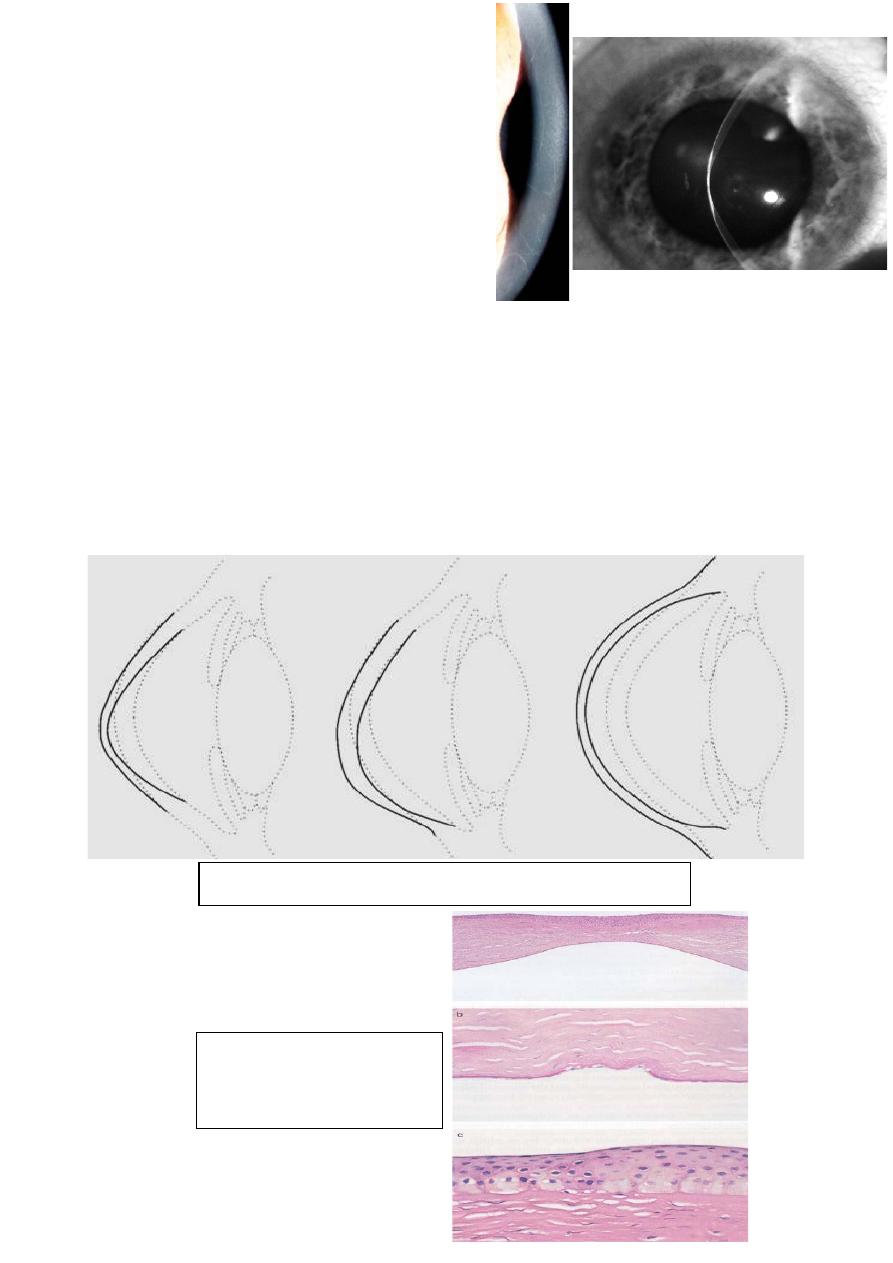
20
Progressive corneal thinning
Histology of
keratoconus
• The onset is around puberty with
slow progression thereafter until
the third or fourth decades of life,
when it usually arrest.
Presentation:
Is typically during puberty with unilateral impairment of vision due to
progressive myopia and astigmatism, which subsequently become
irregular.
The patient may report frequent changes in spectacles prescription or
decrease tolerance to contact lens wear.
Approximately 50% of normal fellow eyes will progress to
Keratoconus within 10 years.
21
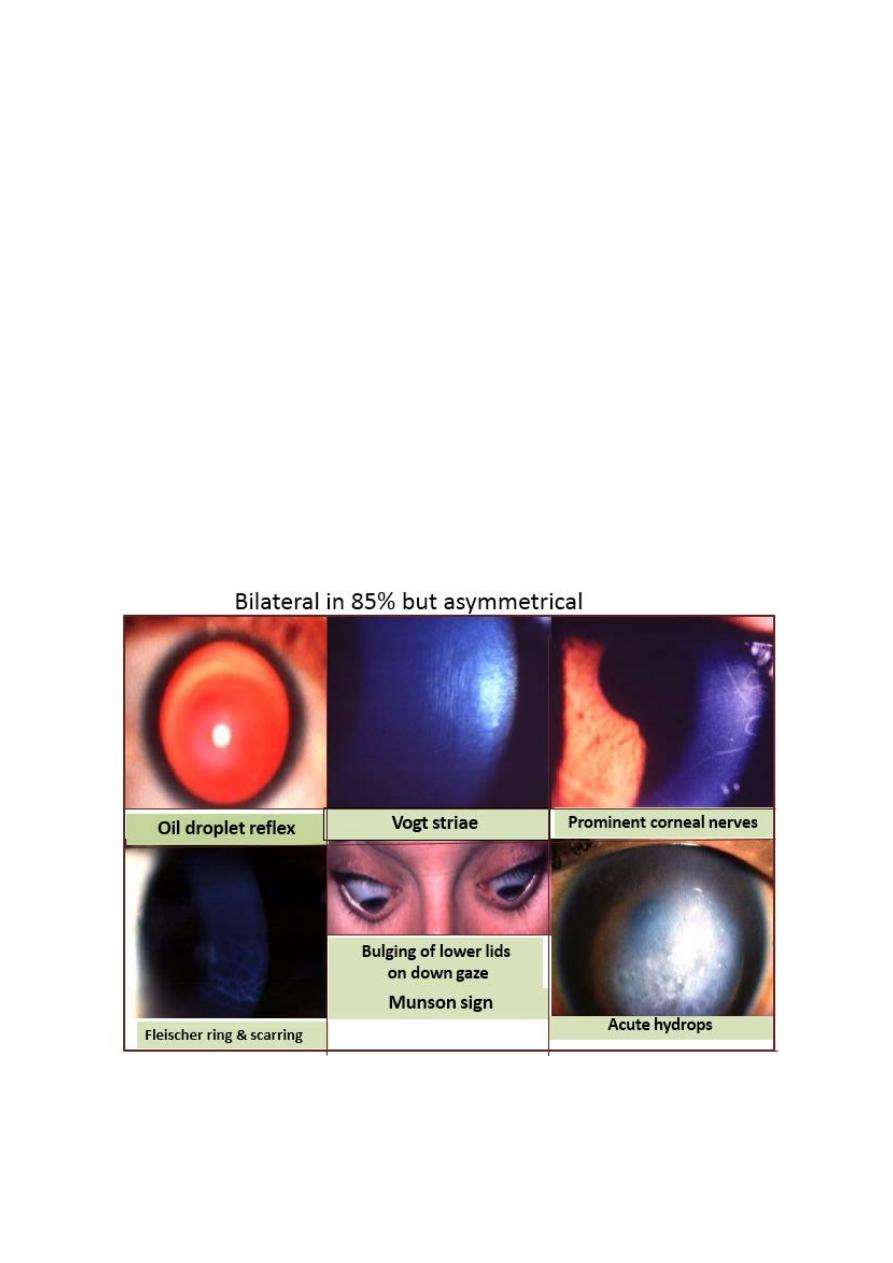
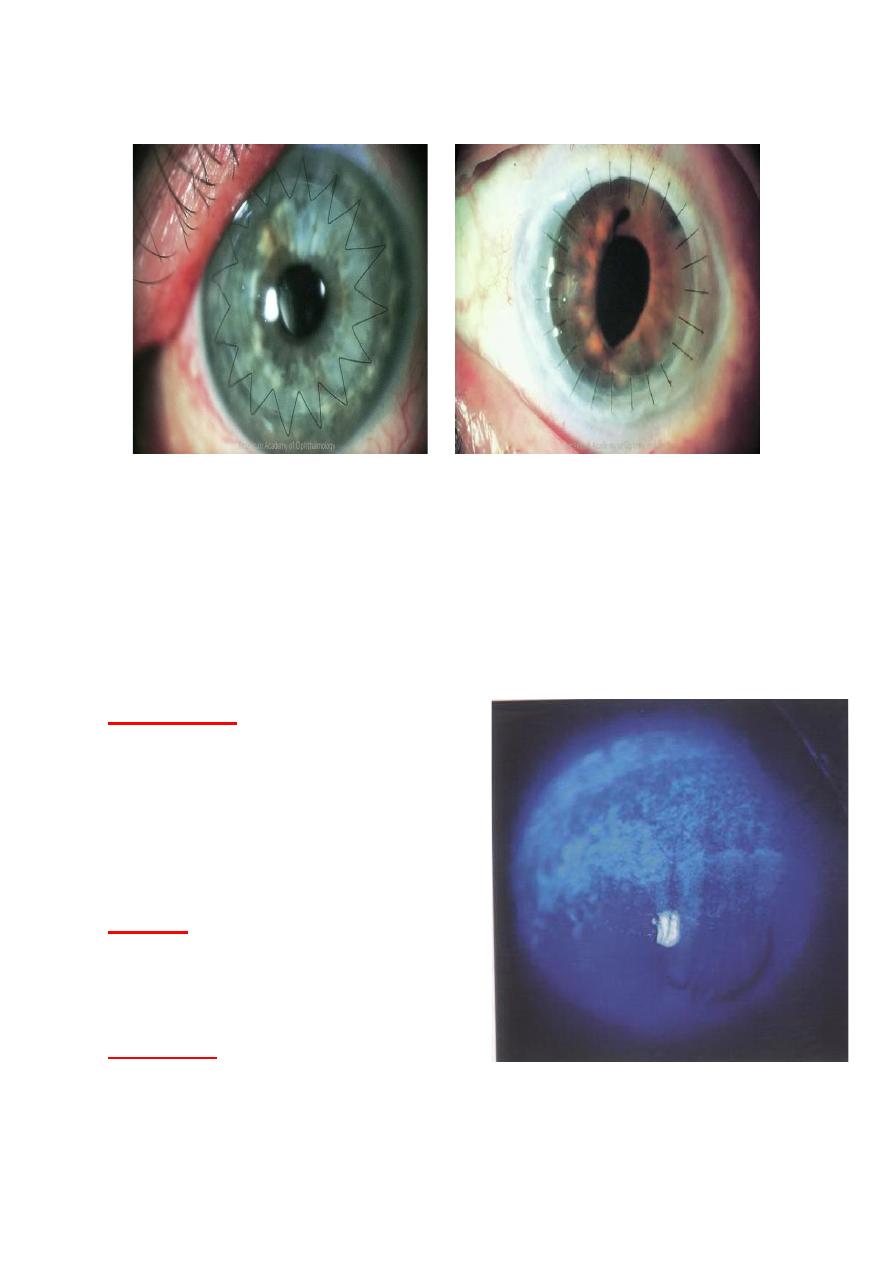
Signs of keratoconus:
Signs:
1- Direct ophthalmoscopy from a distance of one foot shows an oil
droplet reflex.
2- Retinoscopy shows an irregular scissor reflex.
3- Slit-lamp biomicroscopy shows fine, vertical deep stromal striae
(Vogt lines) which disappear with external pressure on globe.
4- Epithelial iron deposits may surround the base of the cone
(Flescher ring) best seen with cobalt blue filter.
Progressive corneal thinning to as little as one third of normal
thickness associated with poor visual acuity resulting from marked
irregular myopic astigmatism.
5- Bulging of lower lid in down gaze (Munson sign).
22
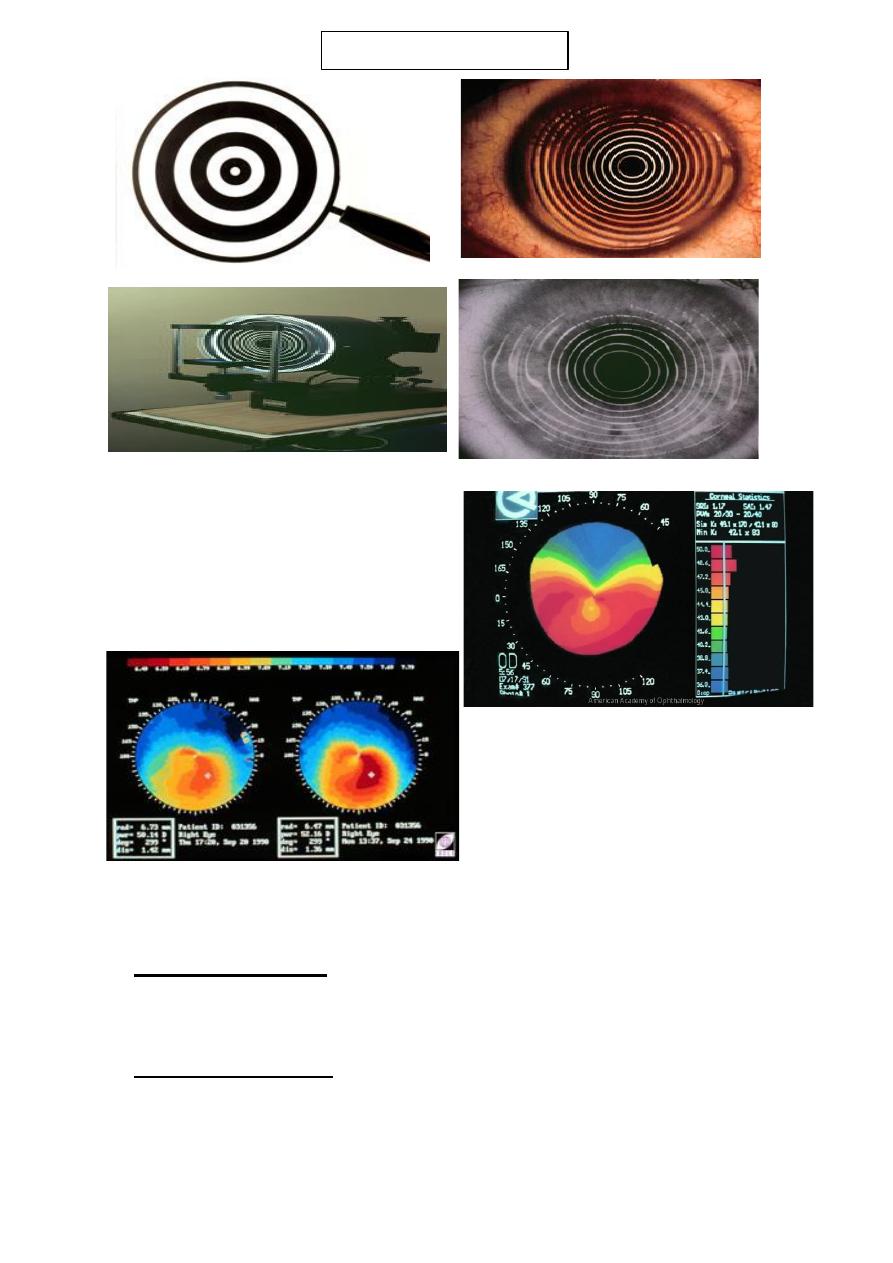
Corneal topography:
shows irregular astigmatism and is
the most sensitive method of
detecting early Keratoconus and
monitoring progression.
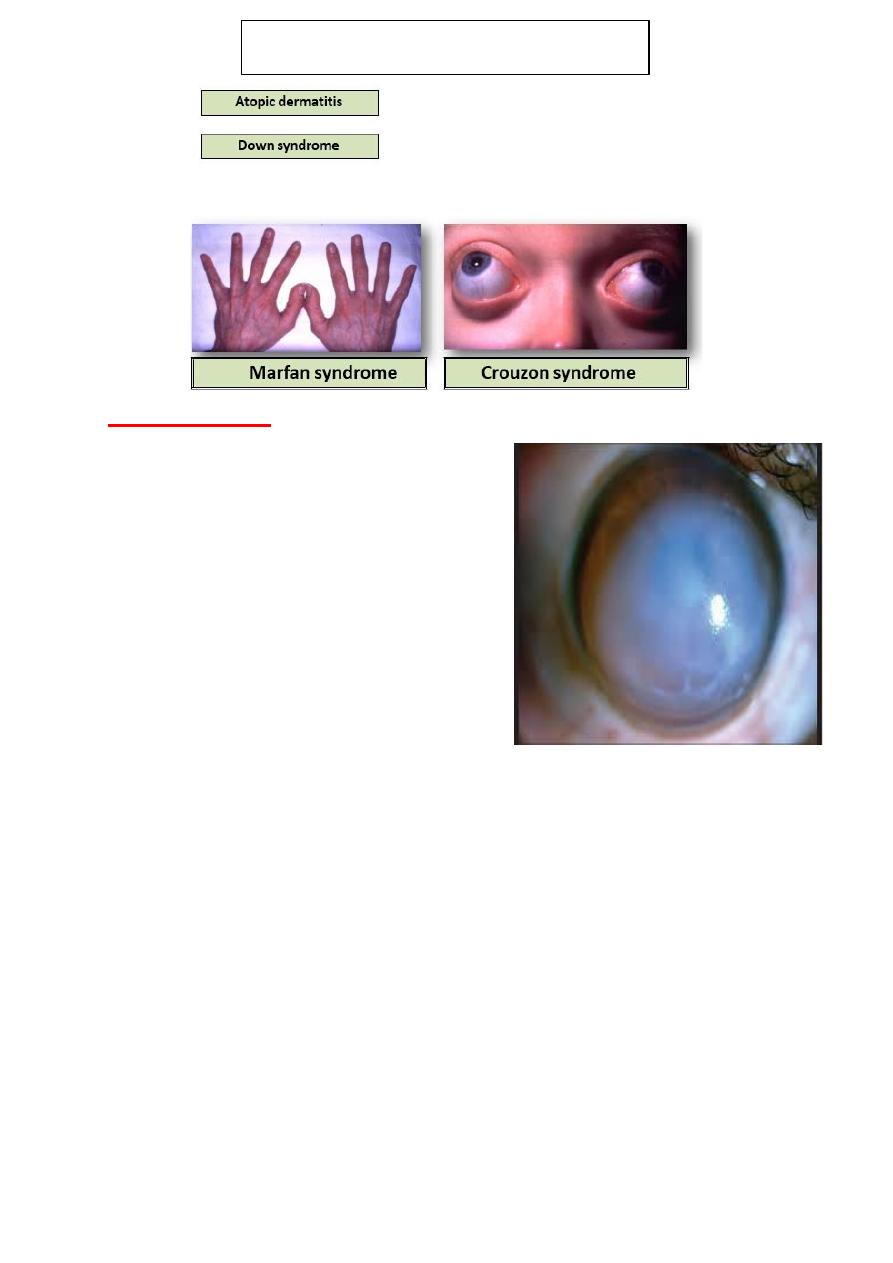
associations of keratoconus:
1- Systemic disorders: Down, Turner, Ehler-Donalos, Marfan
syndromes, atopy, osteogenesis imperfecta, mitral valve prolapse and
mental retardation.
2- Ocular associations: include vernal keratoconjunctivitis, blue
sclera, aniridia, ectopia lentis, Leber congenital Amaurosis and
retinitis pigmentosa.
Plasido disc
23
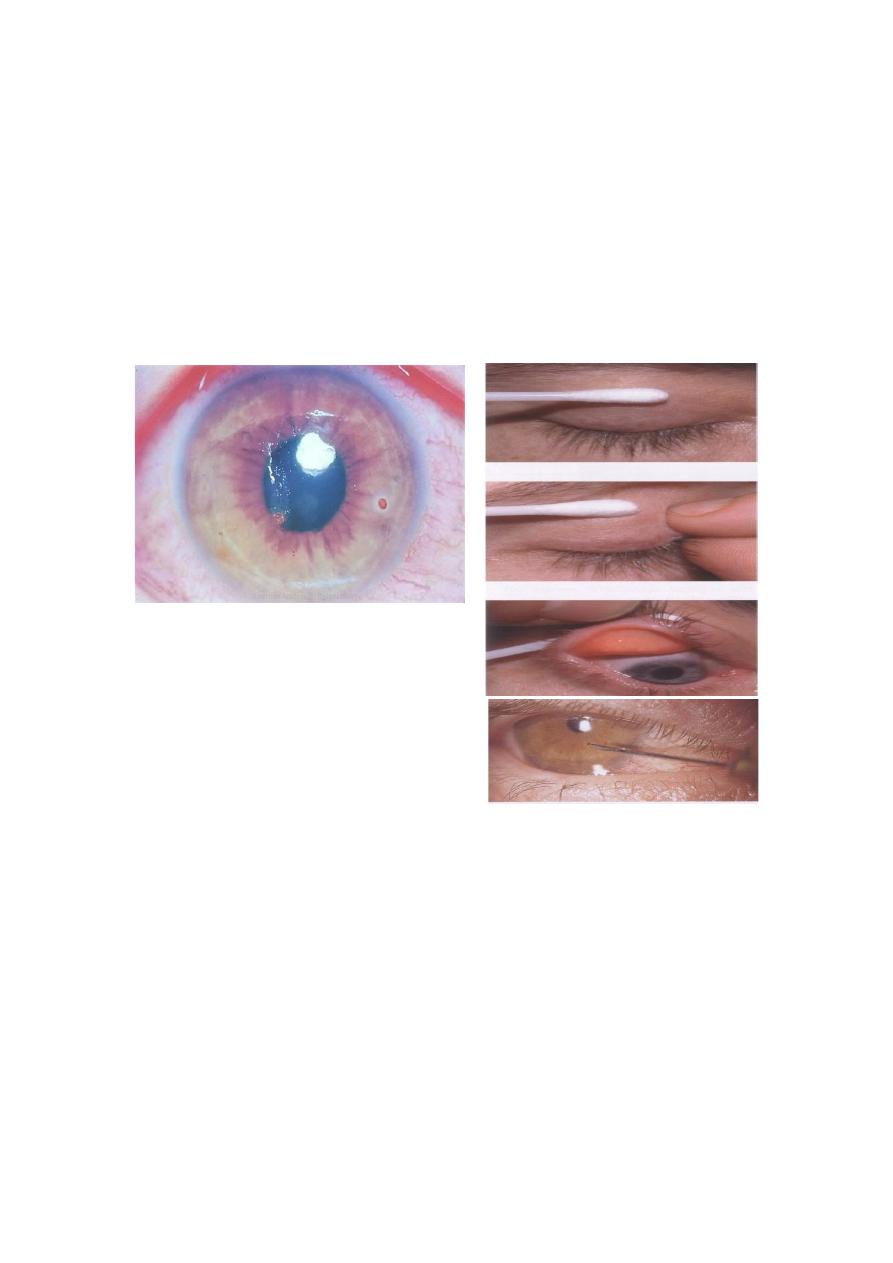
Acute Hydrops:
• Hydrops is an acute complication
of keratoconus that typically
results markedly reduced visual
acuity, pain, photophobia, redness
and tearing.
• It is a direct result of a break in
Descemet′s membrane, which
allows rapid imbibition of aqueous
by hydrophilic stromal
Proteoglycans.
• Corneal thickness rapidly increases and corneal transparency is
reduced. Perforation is a rare complication.
• Proper management includes patching or bandage contact lens
application, cycloplegia and topical hypertonic sodium chloride
drops and/or ointment. Keratoplasty is the definitive treatment.
• It is caused by rupture in Descemet’s membrane that show
influx of aqueous into the cornea. This cause sudden drop in
visual acuity associated with discomfort and watering.
• Although breaks usually heals within 6-10 weeks and corneal
edema clears a variable amount of stromal scarring may
Systemic associations of keratoconus
24
develop. Acute episodes are initially treated with hypertonic
saline and patching of soft bandage contact lens.
• Healing may result in improved visual acuity as a result of
scarring and flattening of the cornea. Keratoplasty should be
deferred until the edema resolved.
Treatment lines:
1- Spectacles: in early cases to correct irregular astigmatism .
2- Rigid contact lenses: are required for higher degree of
astigmatism to provide a regular refracting surface.
3- corneal collagen cross-linking.
4- Intra-corneal ring segment.
5- Keratoplasty: (penetrating or deep lamellar) is indicated for
patients with advanced progressive disease especially with
significant corneal scarring.
Management
of keratoconus consists of two main general
approaches, which are visual rehabilitation by mean of spectacles,
contact lenses, and intracorneal ring segments implantation, and
impending the progression of the disorder by corneal collagen
cross-linking (CXL) using riboflavin and ultraviolet A (UVA)
irradiation.
In advanced cases, lamellar or penetrating keratoplasty is the
recommended treatment option.
Keratoconus:
Treatment Corneal collagen cross linking CXL
Corneal collagen cross-linking is a minimally invasive surgical
treatment used to strengthen the tissue of the ectatic cornea by
augmenting chemical bonds between the stromal collagen fibrils.
Increased stiffness (stiffening effect) of the cornea after CXL results
in stabilization of ectatic disorder. During CXL treatment, the
epithelium has to be removed to permit the penetration of riboflavin
solution into the corneal stroma. Without epithelial debridement, CXL
treatment may impair the efficacy of the CXL process.
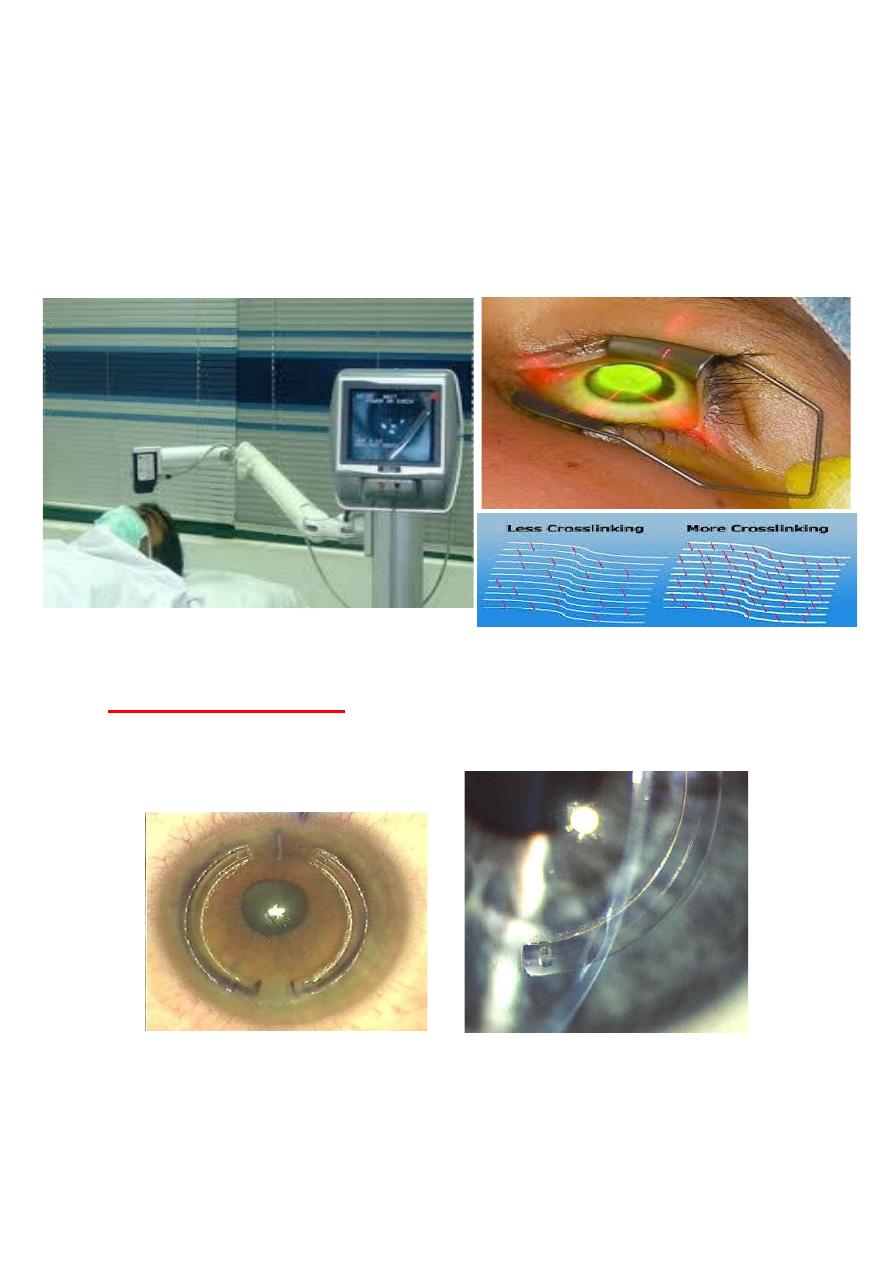
25
Epithelial removal during CXL may be performed either with
mechanical debridement or with Excimer laser trans-epithelial
phototherapeutic keratectomy (t-PRK).
Recently reports of keratoconus patient who demonstrated significant
visual and topographic improvement after CXL treatment using t-
PRK for epithelial removal.
Keratoconus: treatment
Other surgical options:
• Intra-corneal ring
implantation (INTACS).
26
Penetrating keratoplasty (corneal graft)
Corneal injuries:
Corneal abrasion
Corneal foreign body
Radiation damage
Chemical injuries
Corneal abrasion:
Presentation
Immediate pain.
Foreign-body sensation.
Tearing.
Discomfort with blinking.
Causes:
Finger nail, fist, edge of piece of
paper, contact lens improper fit.
Treatment:
Antibiotics eye ointment with
topical cycloplegia.

27
Topical non-steroidal anti- inflammatory agent ± oral pain
medication for 24-48 hours.
Corneal abrasion Are the most common, Result of blunt injury, they
may follow injuries with foreign bodies, fingernails and twigs.
Abrasions could be missed if Fluorescein is not instilled.
The aims of treatment:
To ensure healing of the defect.
Prevent infections.
Relive pain.
Small abrasions can be treated with chloramphenicol ointment twice a
day or eye drops q.i.d.
Large abrasions: double eye pads with chloramphenicol ointment, the
pad must be firm enough to keep the eyelid shut.
If there is significant pain, cycloplegic eye drop (e.g. cyclopentolate
1%) may help.
Oral analgesics, such as paracetamol and NSAIDs can also be used.
Patient should seek further ophthalmological help if the eye continue
to be painful, vision blur, or development of purulent discharges.
Corneal foreign body:
A patient may not recall a foreign body having entered the eye, so it is
essential to be on the lookout for a foreign body if the patient has an
uncomfortable red eye.
Local anesthetics to examine eye and remove foreign body. Local
anesthetics should never be given to patients themselves, because they
impede healing and further injuries may occur to anaesthetized eye!
The upper lid must be everted to exclude a sub-tarsal F.B, particularly
if there is corneal scratches or a continuing feeling that a F.B is
present.
28
Corneal F.B are often more difficult to remove if they are metallic
because they are often “Rust on”. A cotton wool bud can be used for
removal of F.B, but great care must be taken when using this as the
eye may easily be damaged. If there is any doubt, those patients
should be referred to an Ophthalmologist.
When the F.B has been removed, any remaining epithelial defect
remains can be treated as abrasion. They must be removed as they
will prevent healing and may permanently stain the cornea.
Radiation damage:
• The most common form of radiation damage occur when
welding has been carried out without adequate shielding of the
eye.
• The corneal epithelium is damaged by ultraviolet rays and
patient typically presents with painful weeping eyes some hours
after welding and commonly known as “ Arc eye”.
•
Treatment:
as for corneal abrasion.
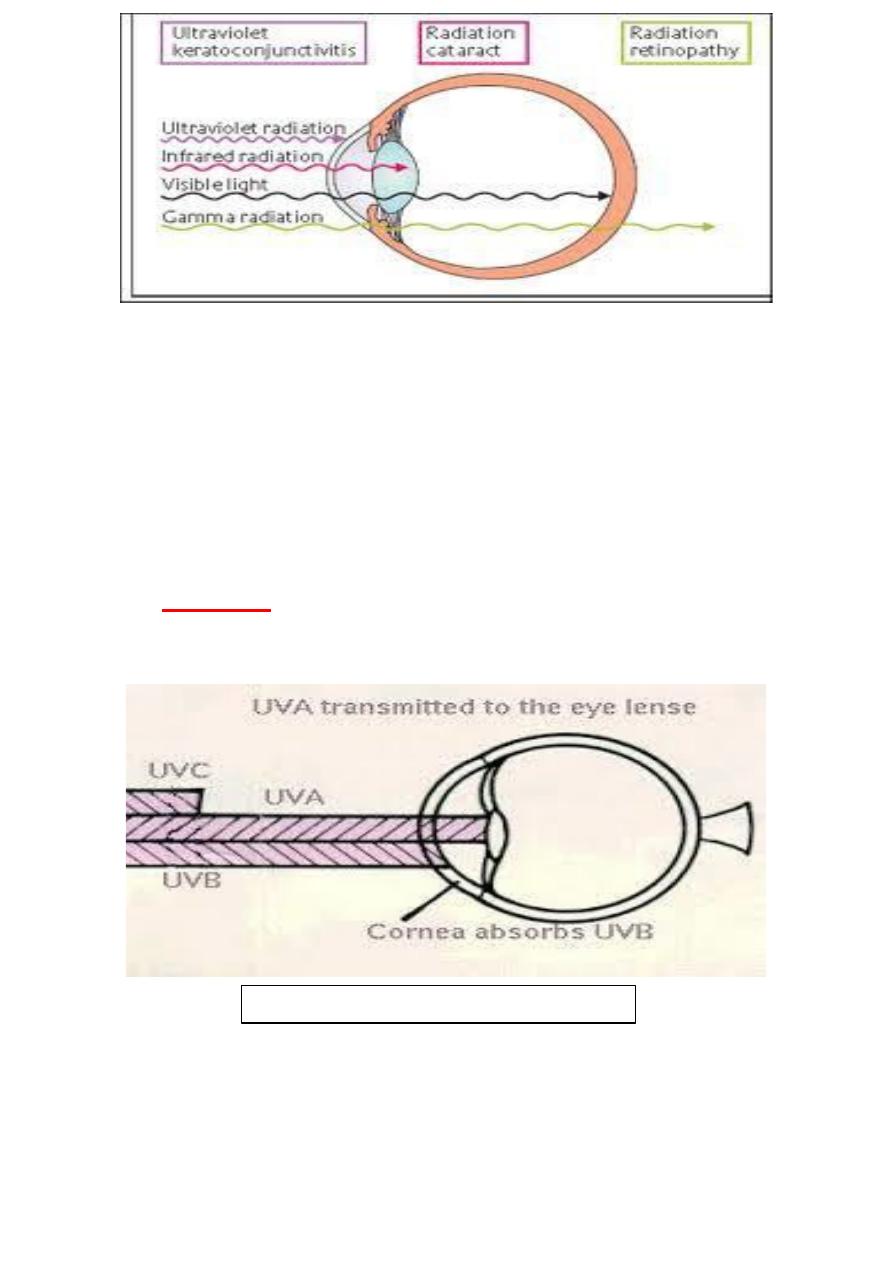
29
The most common causes of ocular UV injuries are unprotected
exposure to sun-lamps, arc welding, and prolonged out door
exposure to reflected sunlight.
Snow blindness, which occurs in skiers and mountain
climbers, is caused by UV light reflected from snow.
Appropriate protection with UV-filtering eyewear can
prevent such injuries.
Treatment:
Patching to minimize discomfort from eye movement, topical
antibiotic ointment and cycloplegia, with systemic analgesia.
Radiation damage: ultraviolet light

30
Chemical injuries:
All chemical eye injuries are potentially blinding injuries.
If chemicals are splashed into the eye, the eye and the conjunctival
sacs (fornices) should be washed out immediately with copious
amount of water.
Acute management should consist of three “Irrigate, Irrigate,
Irrigate“.
Alkali are potentially damaging and any loose bits such as lime
should be removed from the conjunctival sac with the aid of local
anesthetics if necessary.
Management:
Copious irrigation to neutralize PH.
Double evertion of eyelid, so that any retained particulate matter may
be removed.
Debridement of necrotic area of corneal epithelium to allow for
proper re-epithelialization.
Medical treatment:
Short course of steroid 7-10 days.
Cycloplegic (cyclopentolate 1%).
Prophylactic antibiotics for about 7-10 days.
Ascorbic acid: it improves wound healing topical Sod. Ascorbate 10%
is given two hourly in addition to systemic dose of 2 grams q.i.d.
Citric acid: reduce intensity of inflammatory response (topical Sod.
Citrate 10% 2 hourly for 10 days).
Tetracycline: effective collagenase inhibitors and inhibits neutrophils
activities and reduce ulceration.
Doxycycline 100 mg b.d.
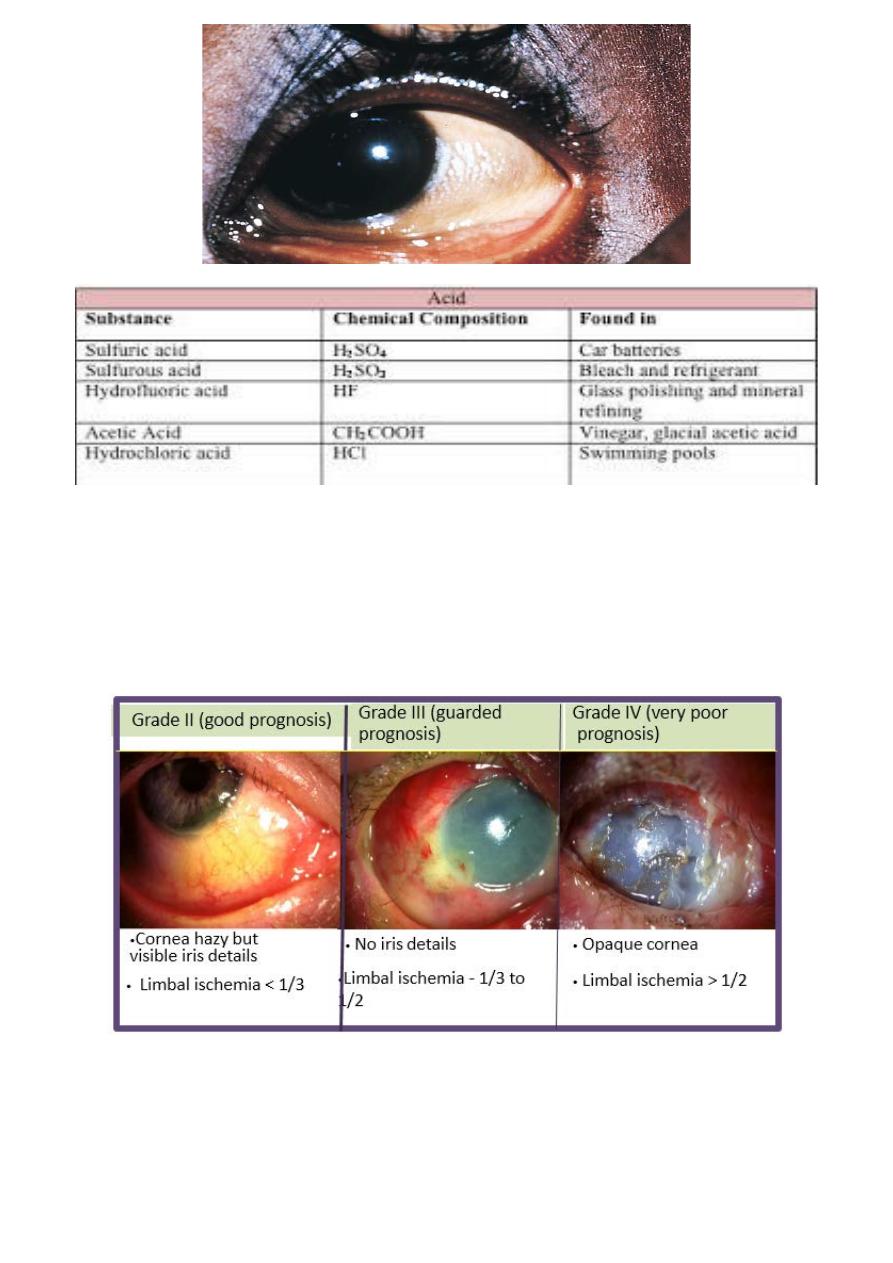
31
Grading of severity of chemical injuries:
Grade I (excellent prognosis)
• Clear cornea
• Limbal ischemia - nil
32
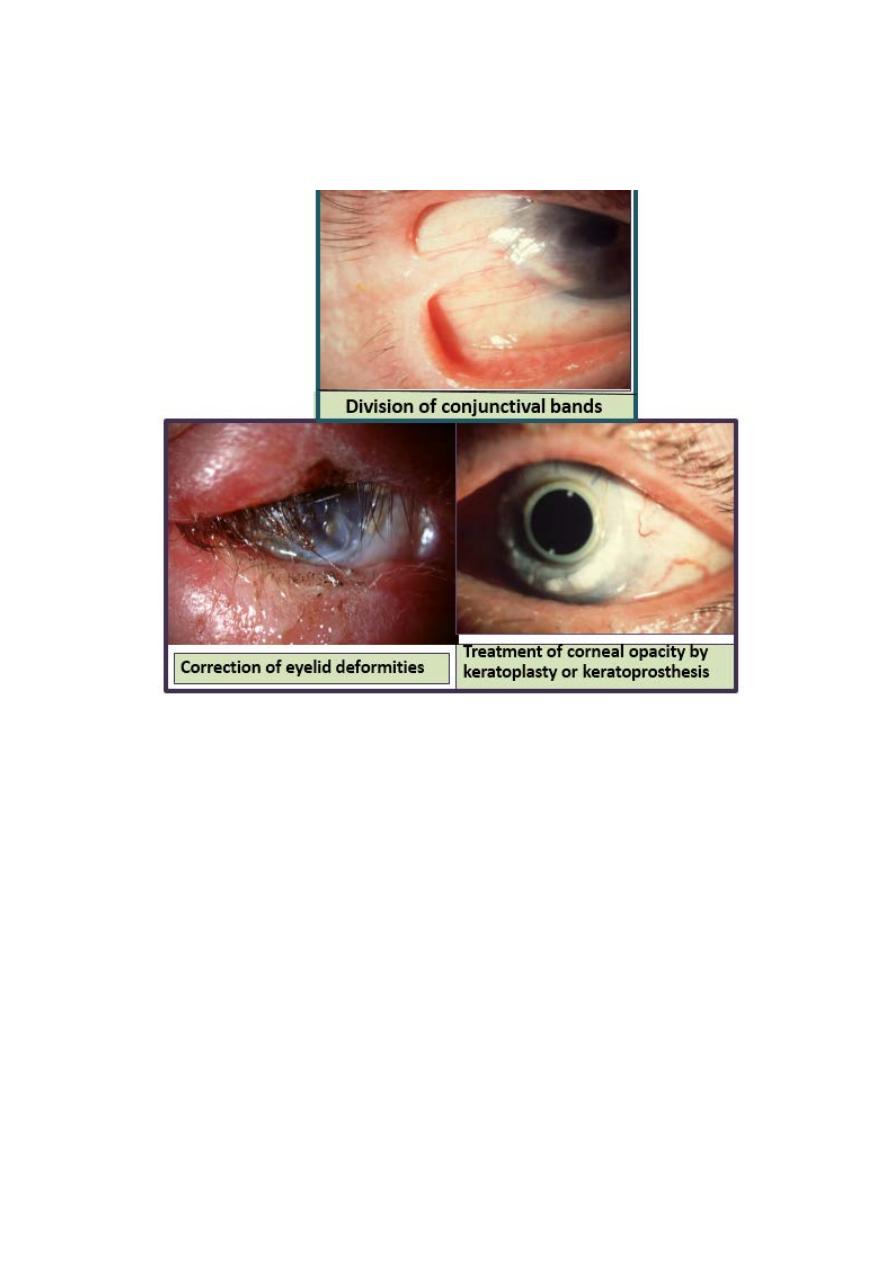
Surgical treatment of chemical injuries:
