EYELIDS
Dr Abdul melik Shallal
Eyelids
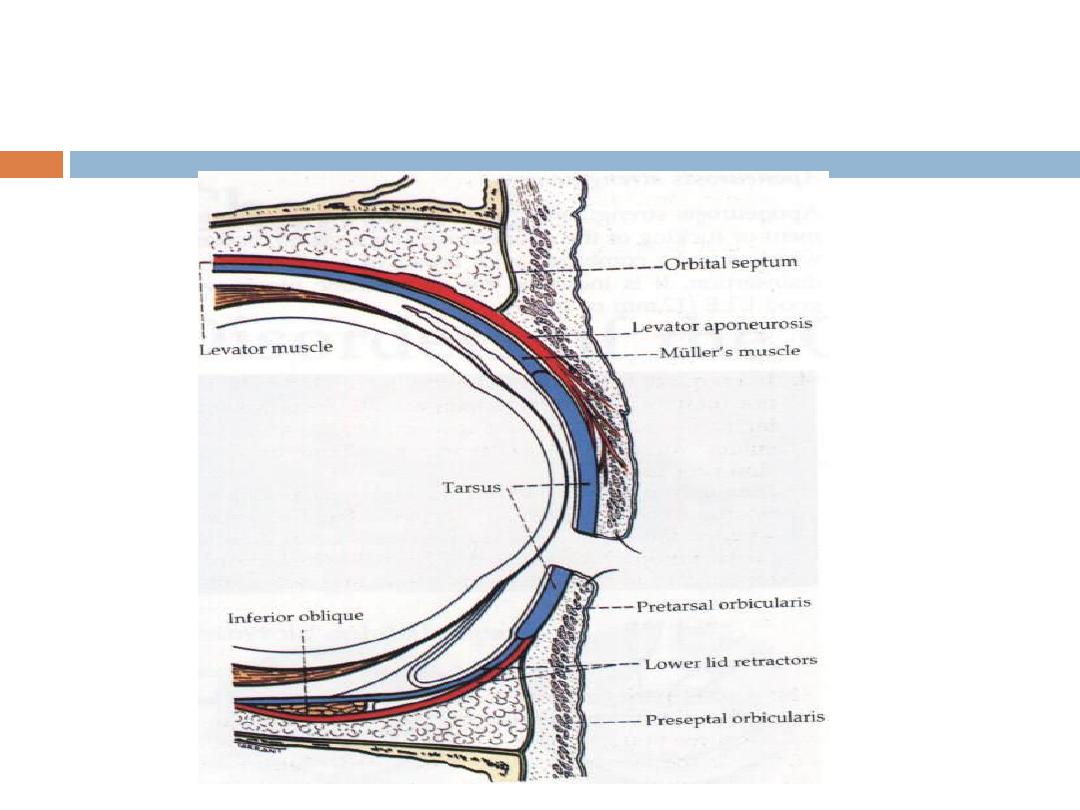
Anatomy:
Eyelids are thin movable curtains composed of
skin
on their
anterior surface
and mucus
membrane (
conjunctiva
) on the
posterior surface
Eyelids
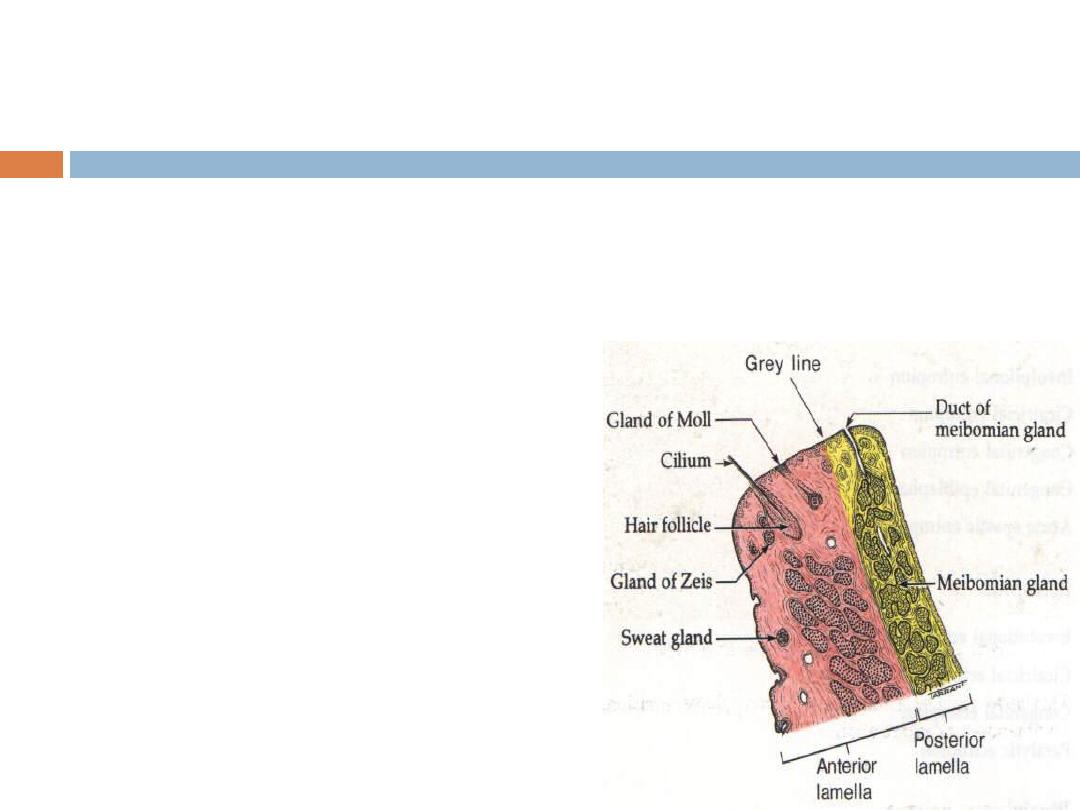
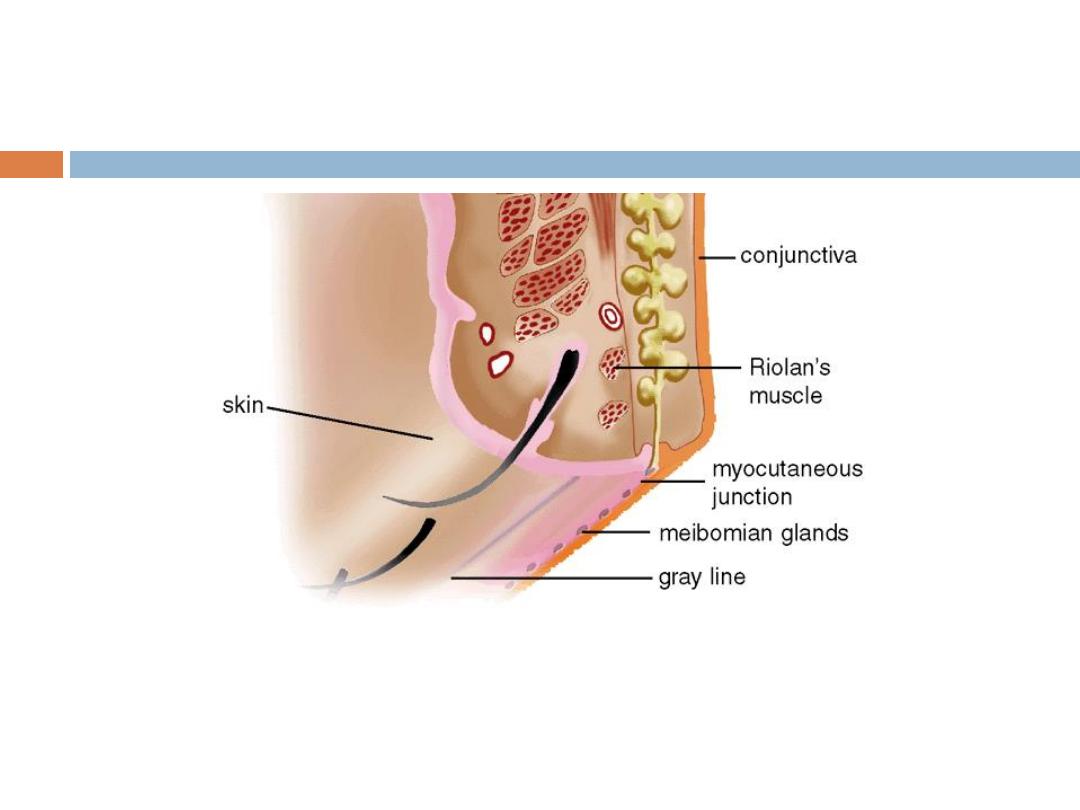
The free margin of the eyelids
contains:
1- The lashes (Cilia).
2- Grey line
3- Mucocutaneous junction.
4- Orifices of Meibomian glands.
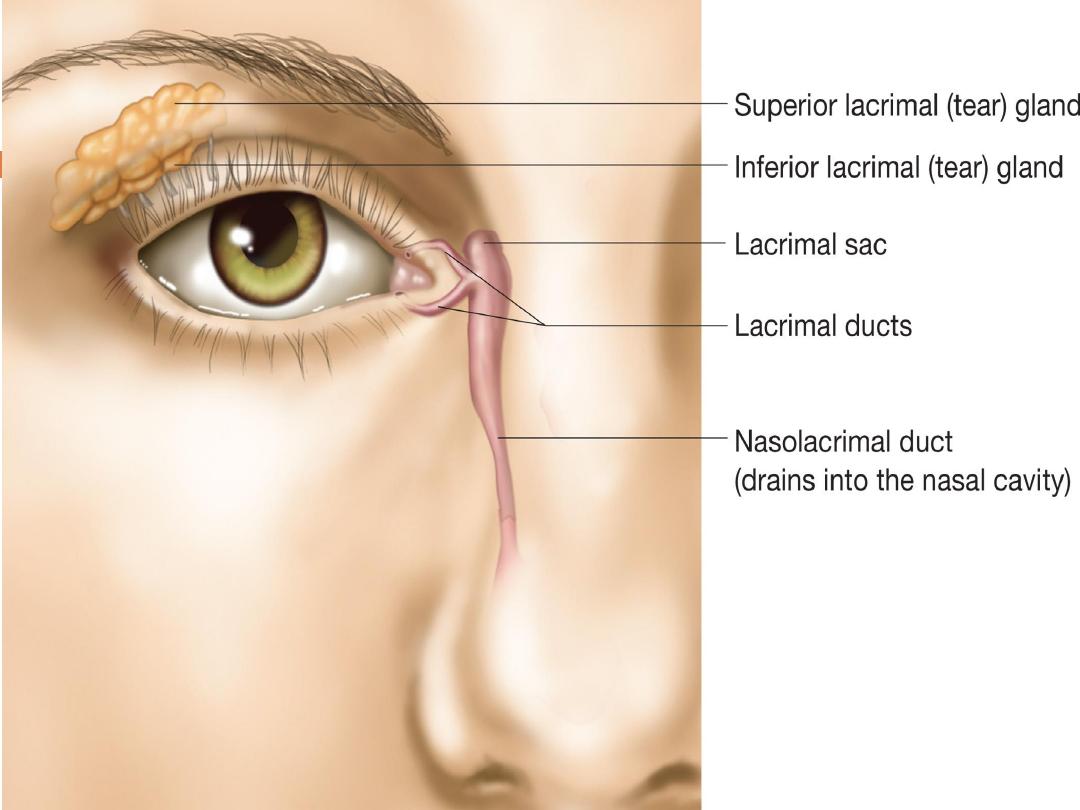
5- Superior and inferior puncti of
Naso- lacrimal system.
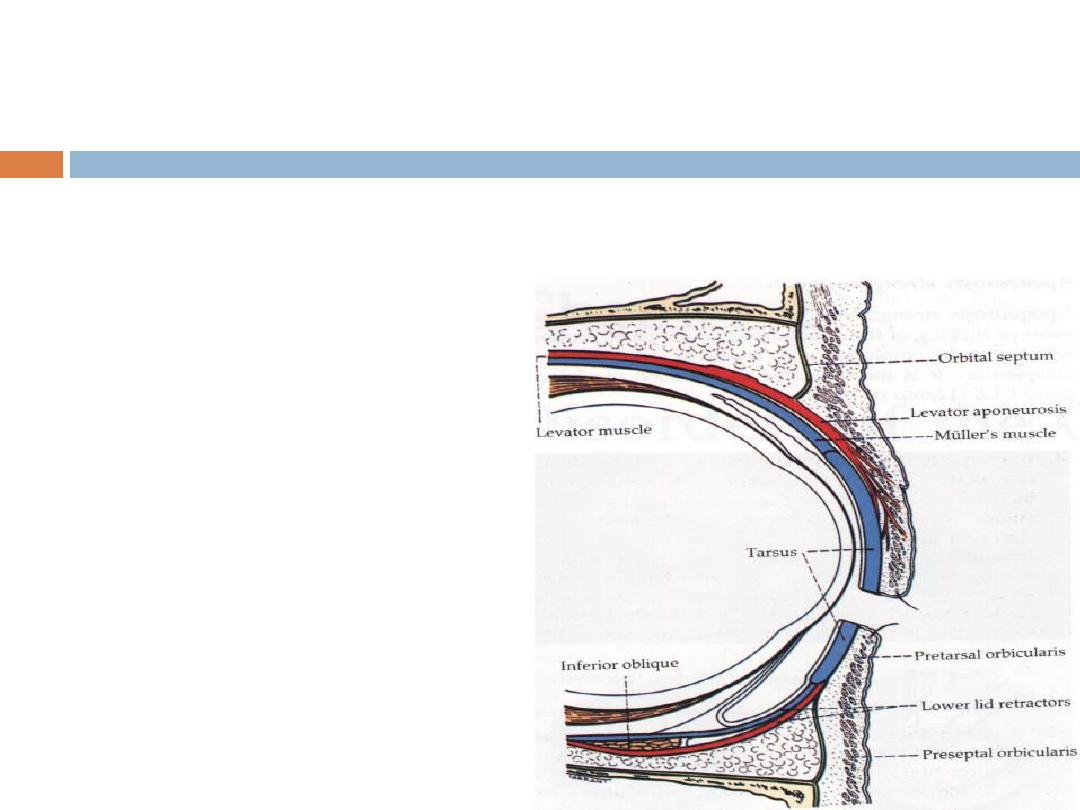
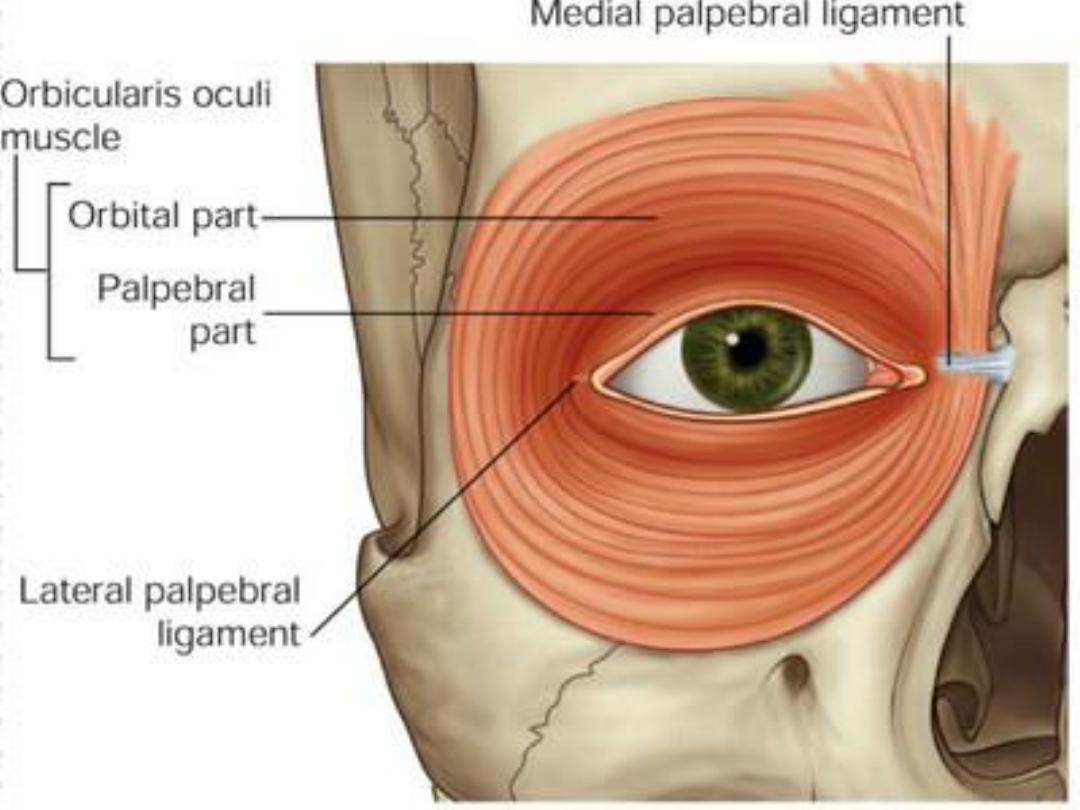
Muscles of the eyelids:
1- Orbicularis oculi muscle:
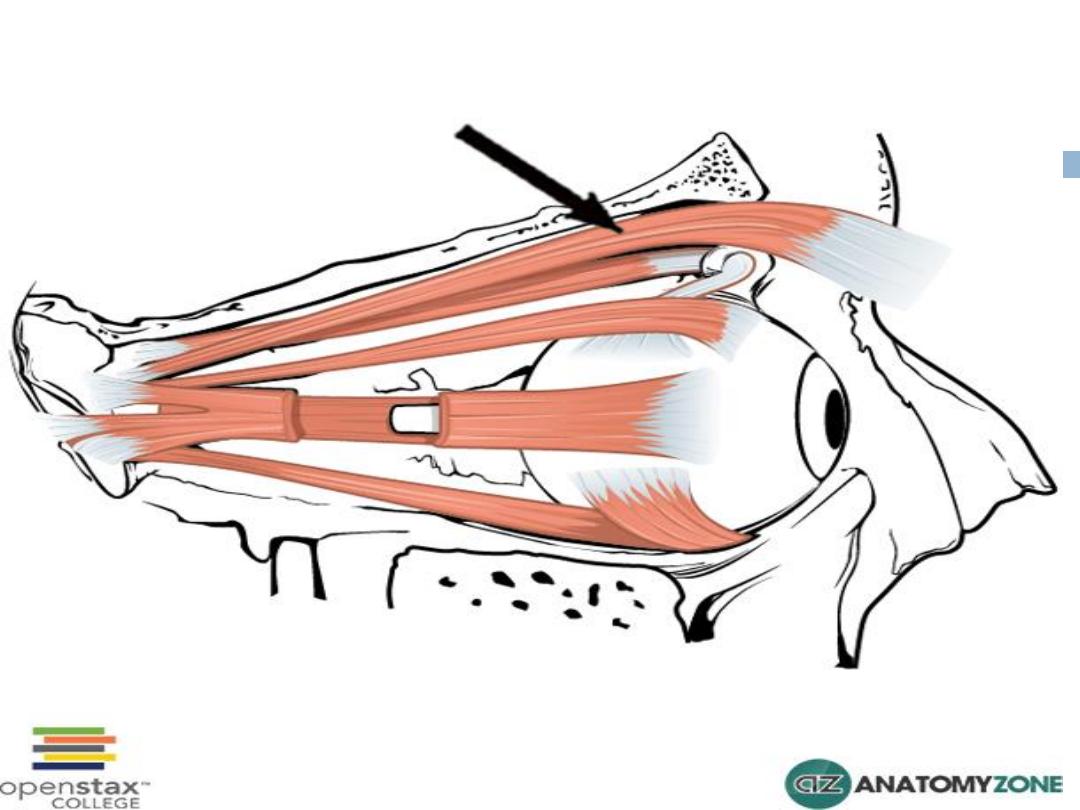
2- Levator palpebrae superioris
muscle:
3- Superior palpebral muscle
(Müller's muscle or superior tarsal
muscle):
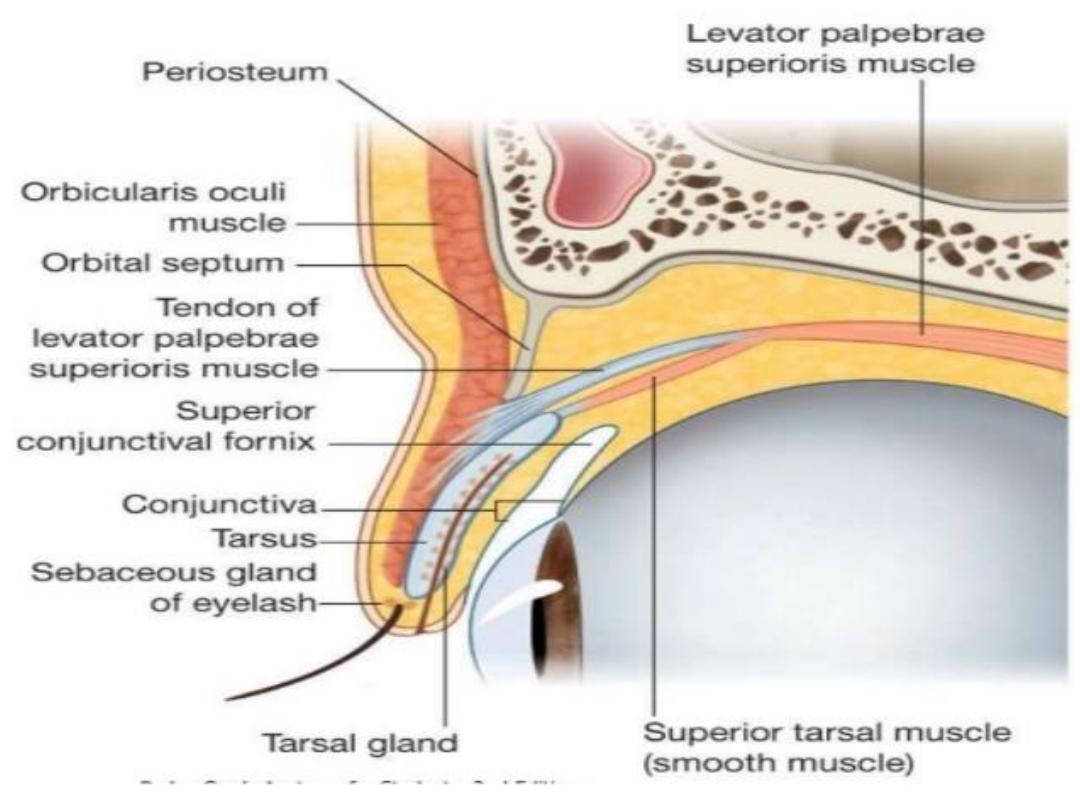
Glands in the eyelids:
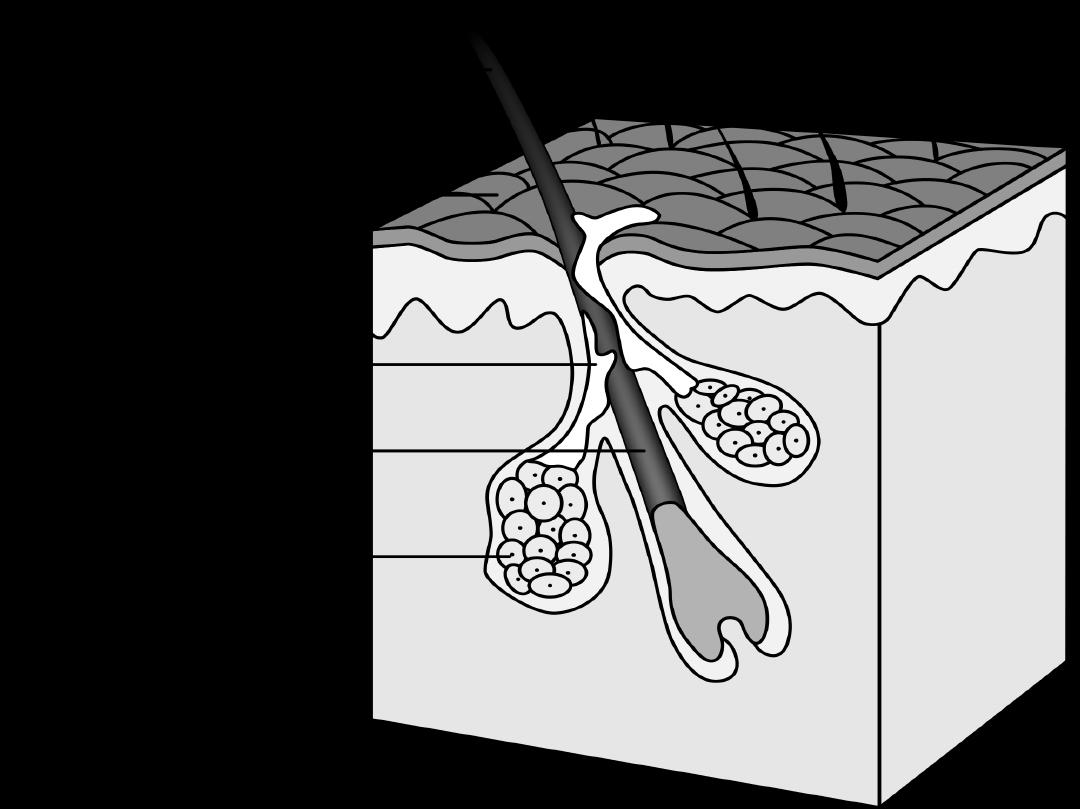
1- Meibomian glands (Tarsal gland):
2- Zeis glands:
3- Glands of Moll:
Congenital anomalies of eyelids:
1- Ablepharon:
2- Ankyloblepharon:
3- Coloboma.
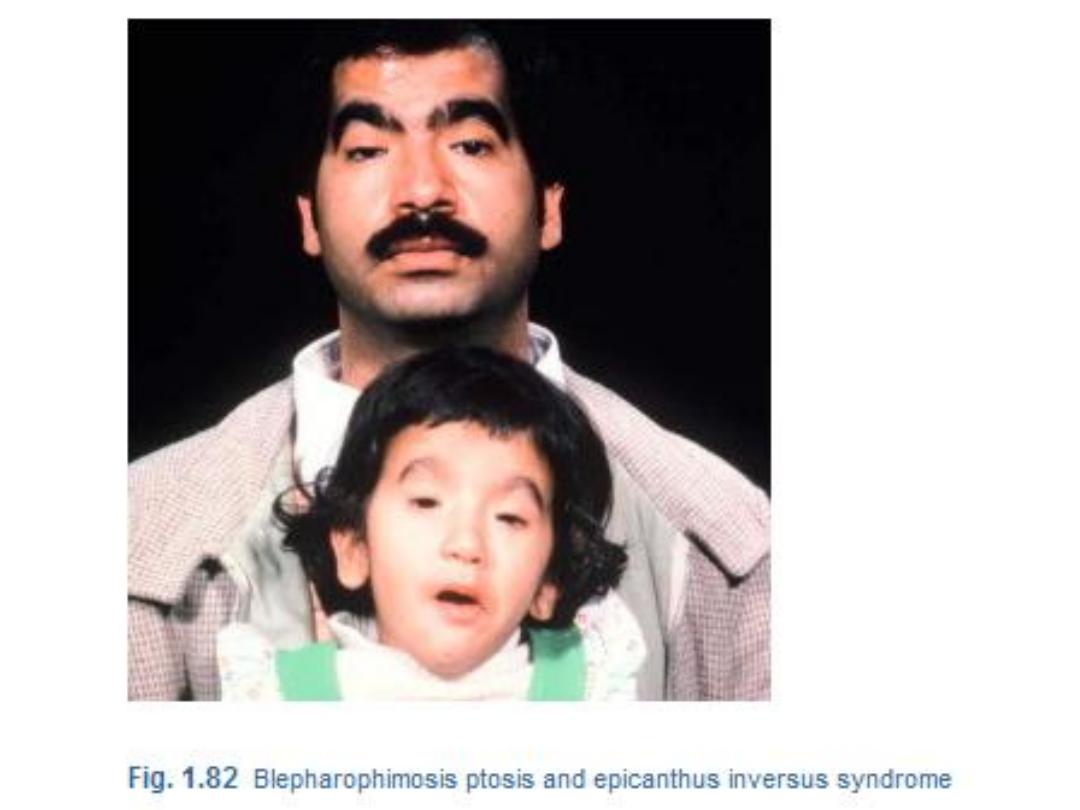
4- Blepharophimosis:
5- Epicanthus:


Abnormalities in shape and position:
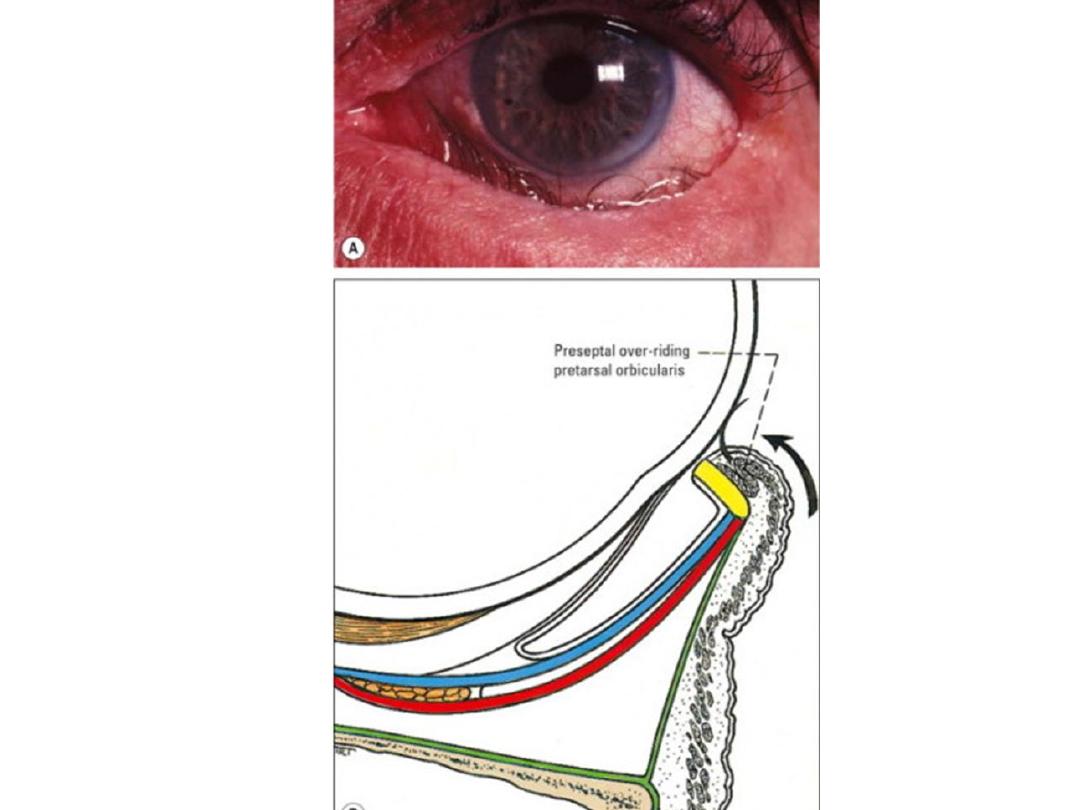
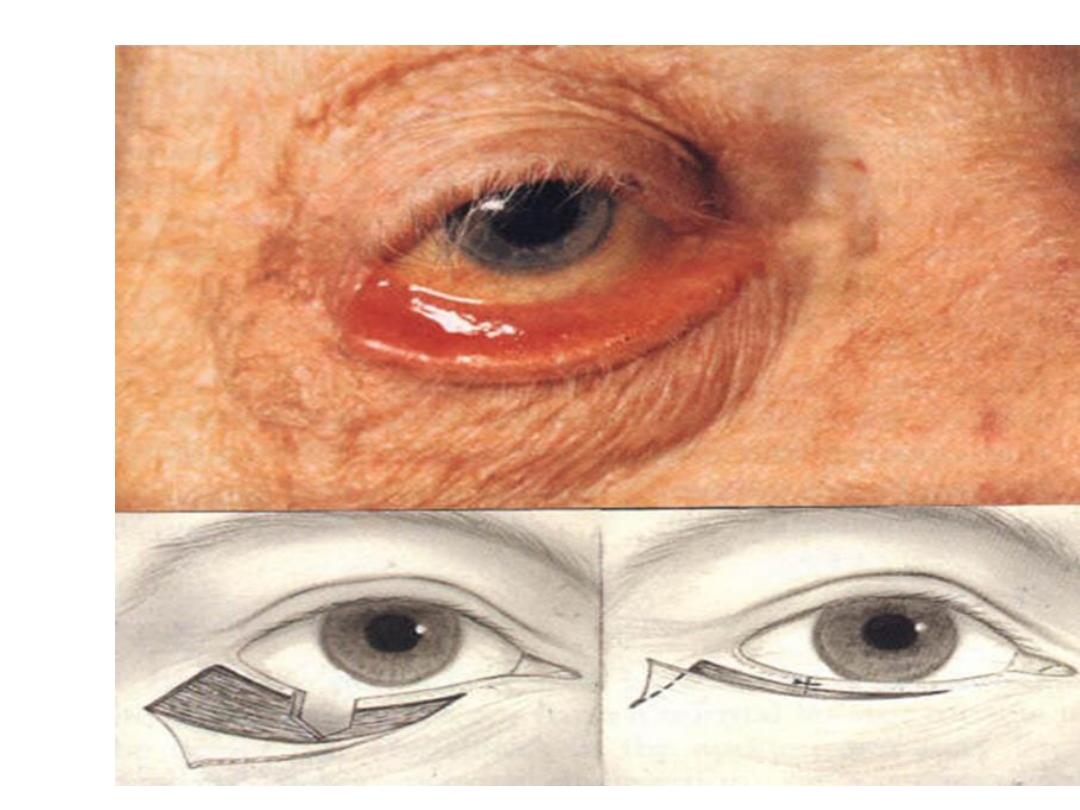
1- Entropion:
a- Congenital
b- Senile
c- Cicatricial
d- Spastic
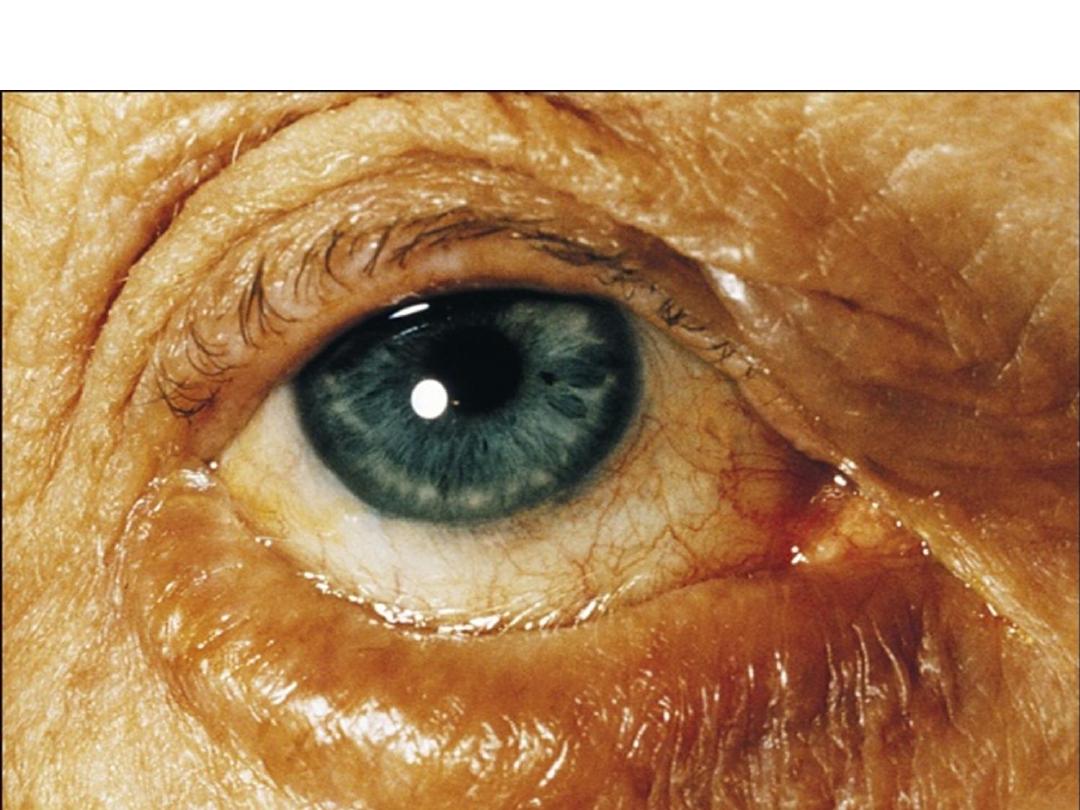
2- Ectropion:
a- Congenital
b- Senile (involutional)
c- Cicatricial
d- Paralytic
c- Mechanical


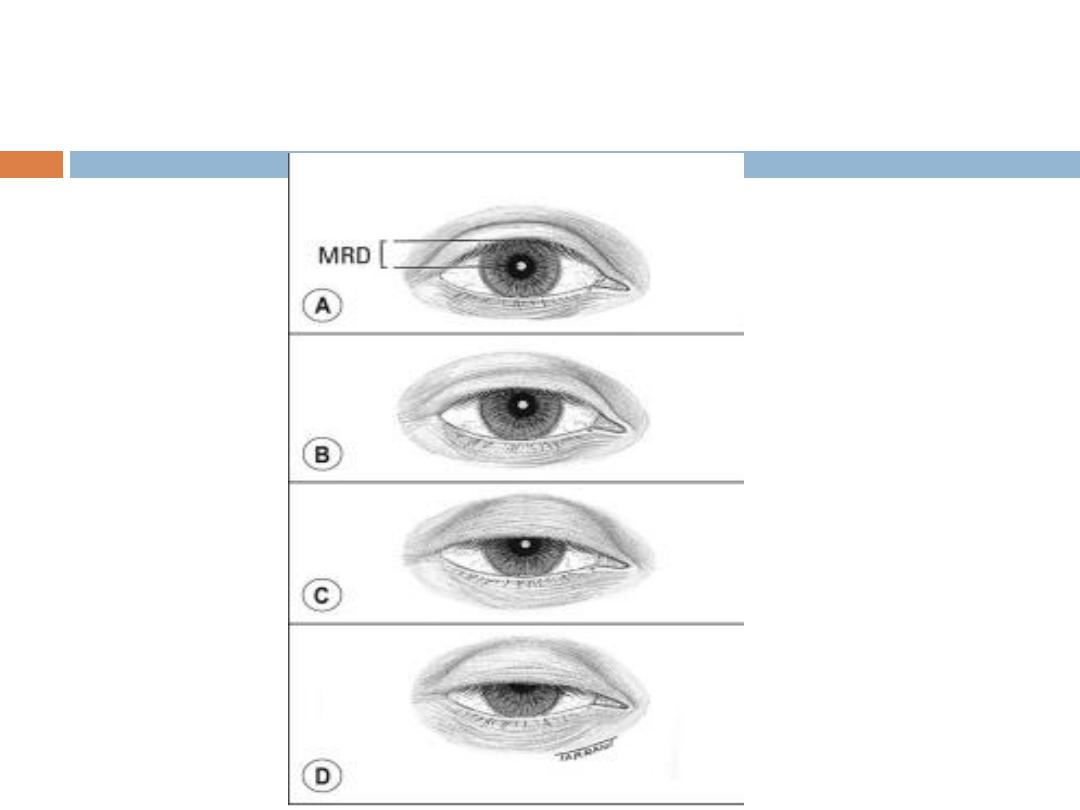
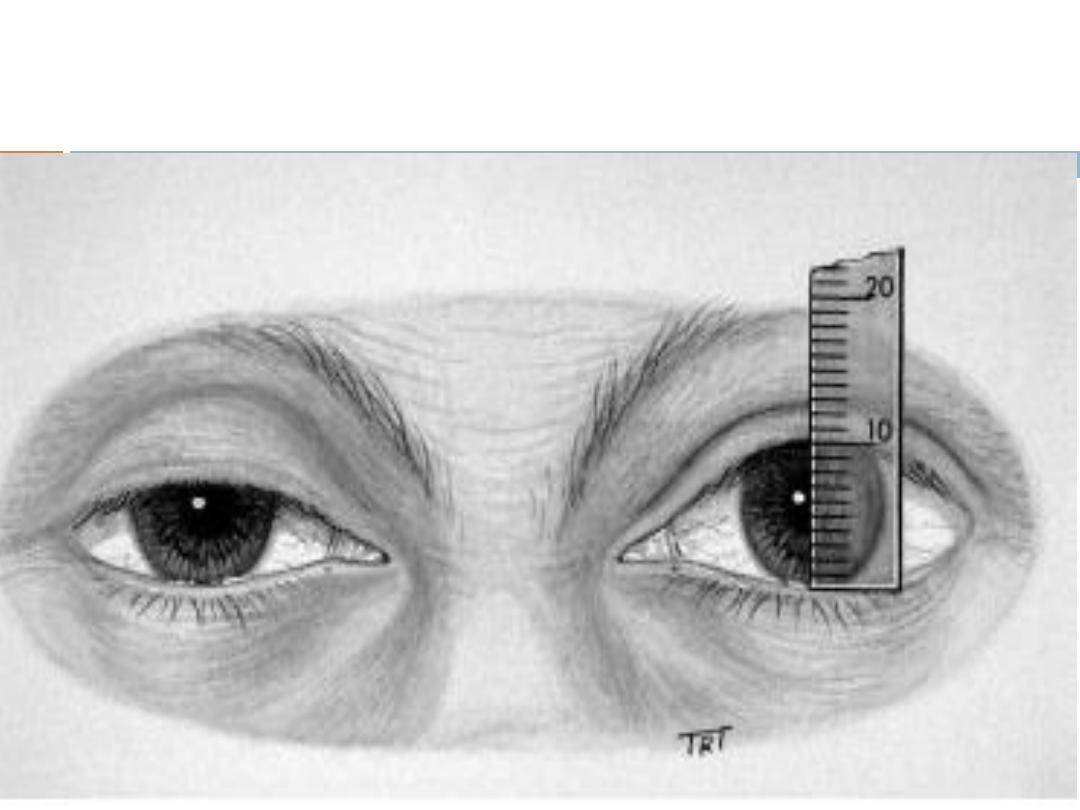
3- Blepharoptosis
3- Blepharoptosis
3- Blepharoptosis
3- Blepharoptosis:
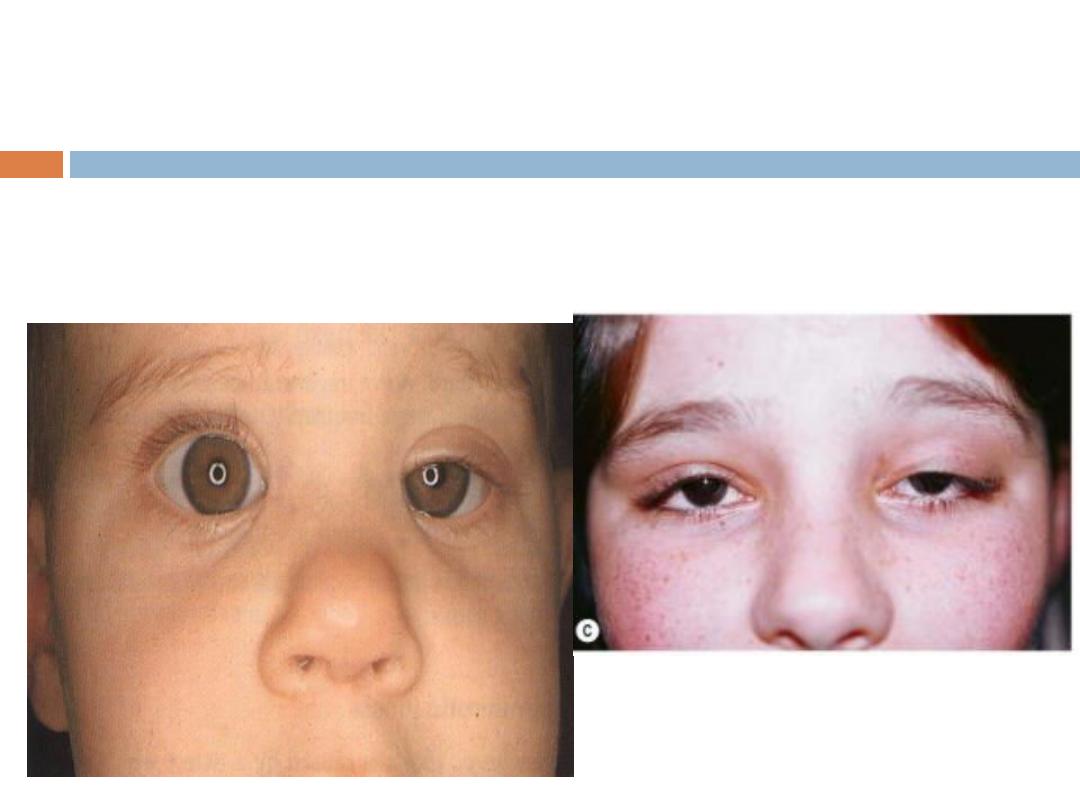
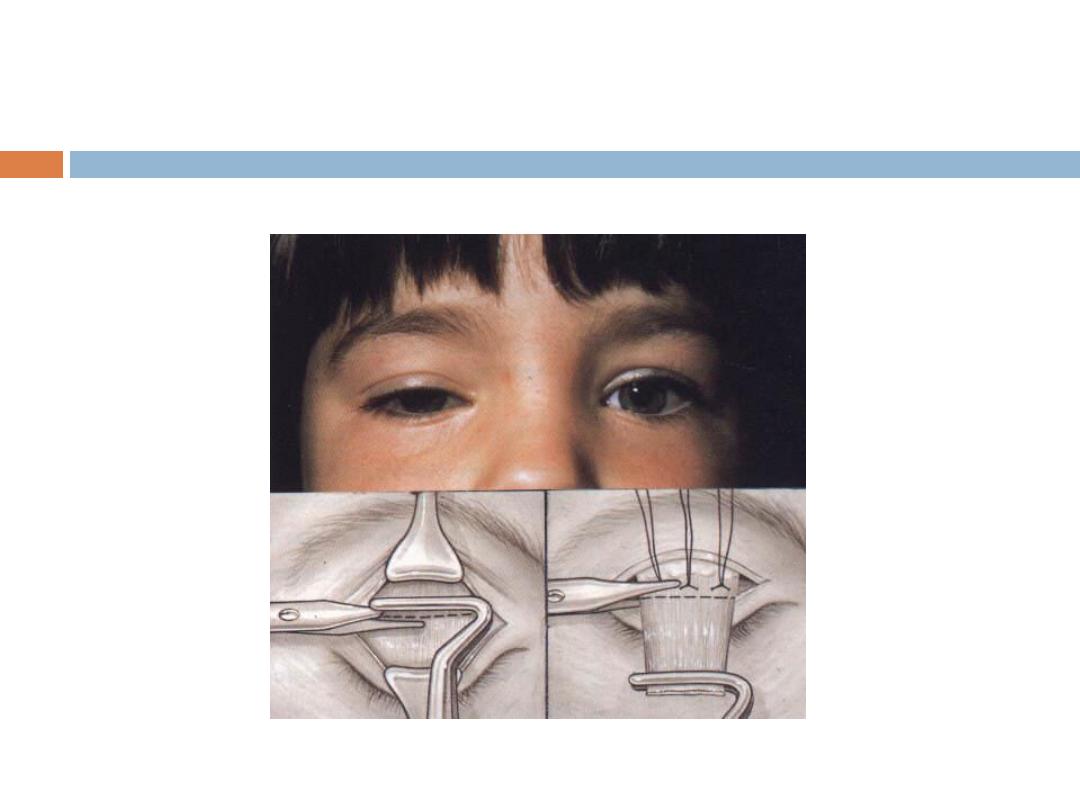
a- Congenital blepharoptosis:
3- Blepharoptosis:
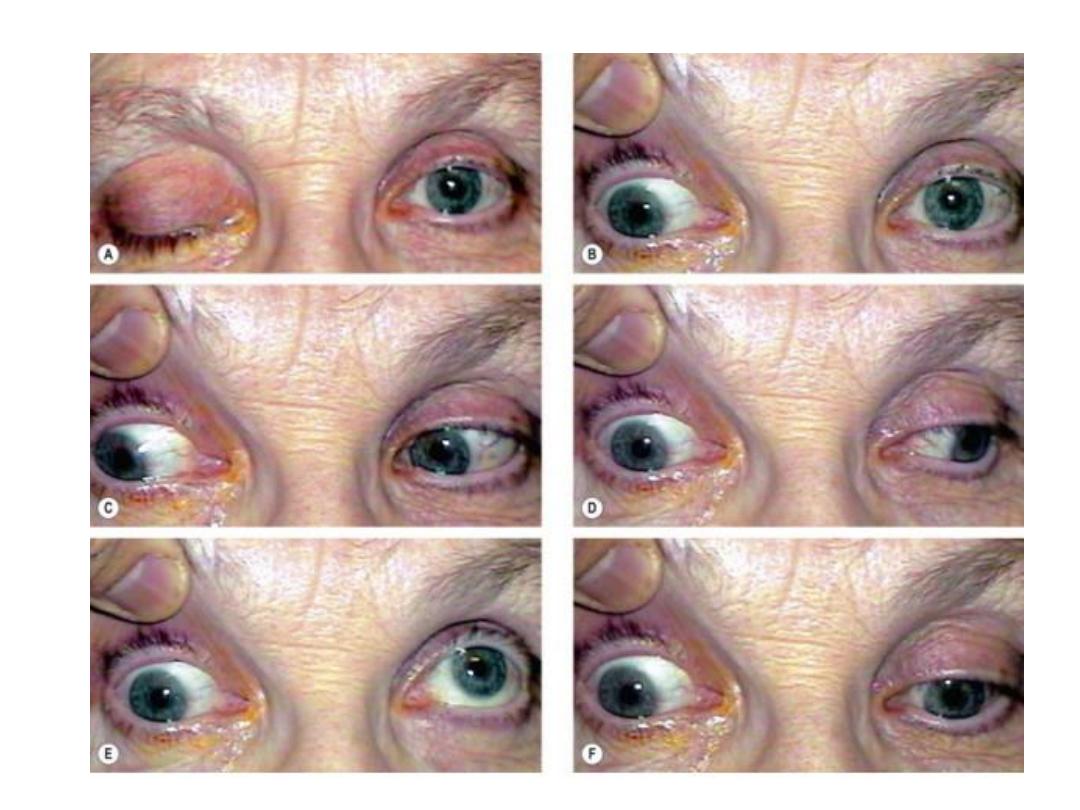
b- Neurogenic blepharoptosis:
i- Oculomotor nerve palsy:
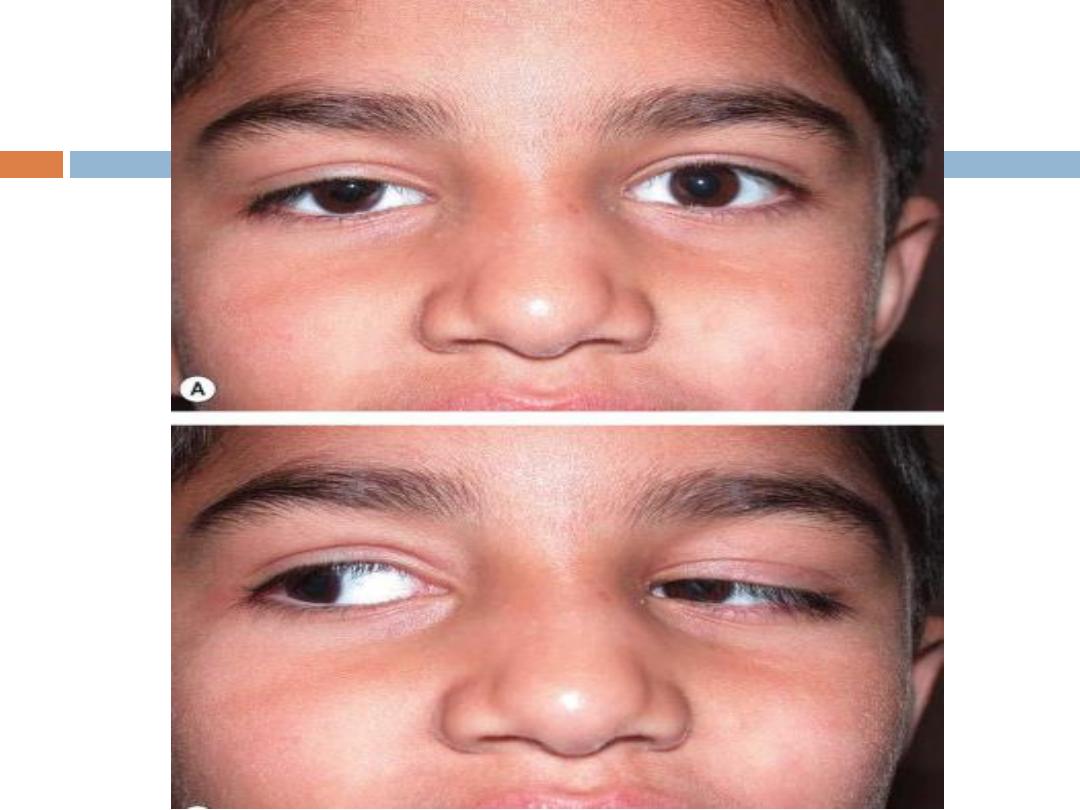
ii- Horner's syndrome
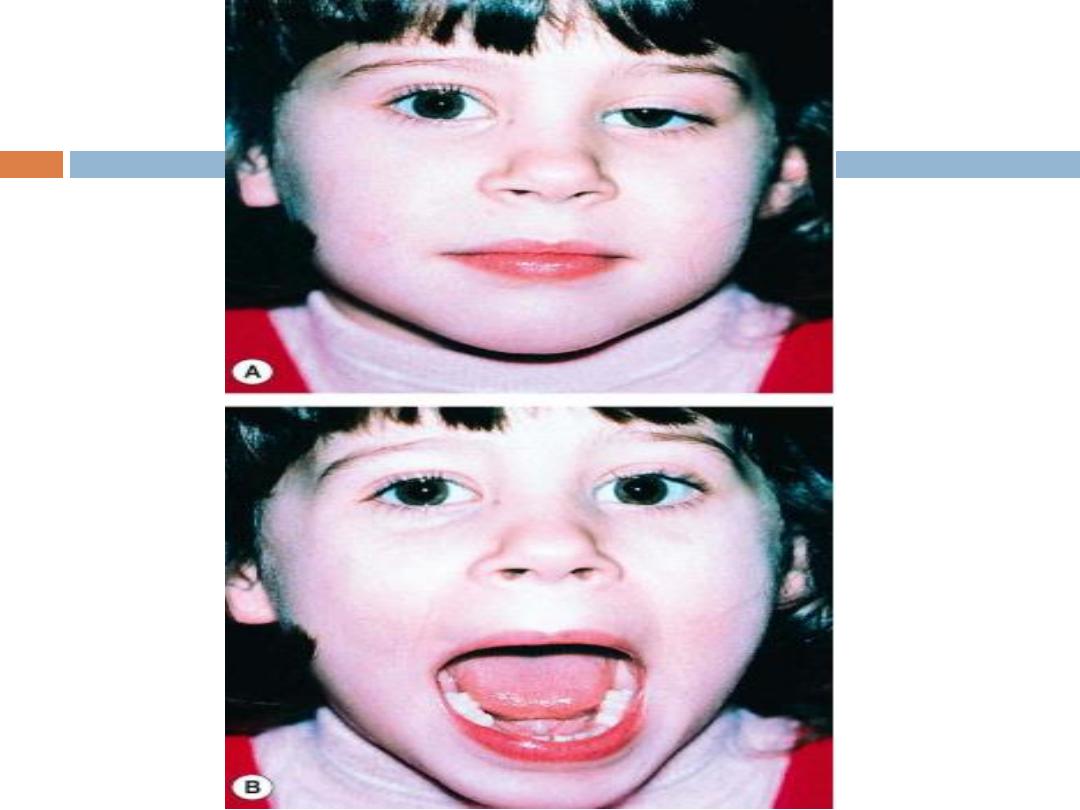
iii- Marcus Gunn Jaw-winking syndrome
iv- 3rd nerve misdirection:
why it is severe in (i) and mild in (ii)?

3- Blepharoptosis:
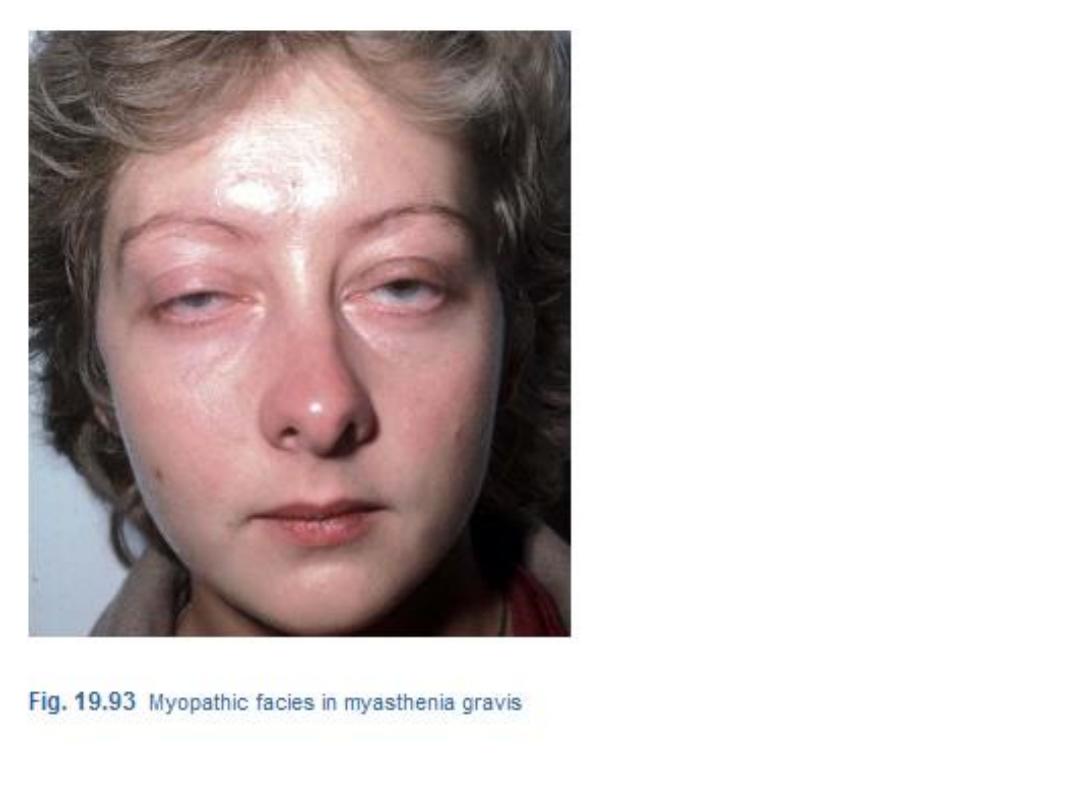
c- Myogenic blepharoptosis:
i- Myasthenia gravis:
ii- Myotonic dystrophy.
iii- Ocular myopathy
iv- Simple congenital myogenic blepharoptosis
v- Blepharophimosis syndrome.

3- Blepharoptosis:
d- Aponeurotic blepharoptosis:
i- Involutional (senile).
ii- Post operative.

3- Blepharoptosis:
e- Mechanical blepharoptosis:
i- Trachoma, VKC and eyelid tumor.
ii- Cicatricial
(due to LS and superior rectus fibrosis).
iii- Trauma
(collection of fluid).
iv- Iatrogenic by surgeons.
v- Lack of support (thisical or nanophthalmos)
3- Blepharoptosis:
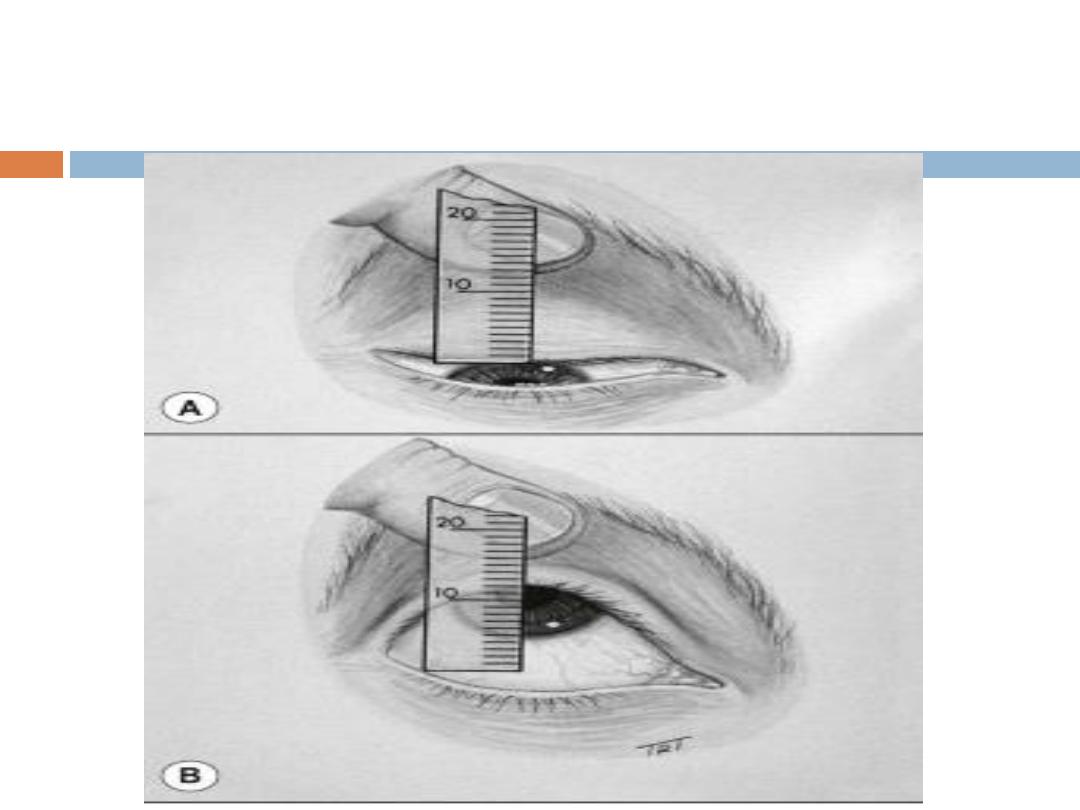
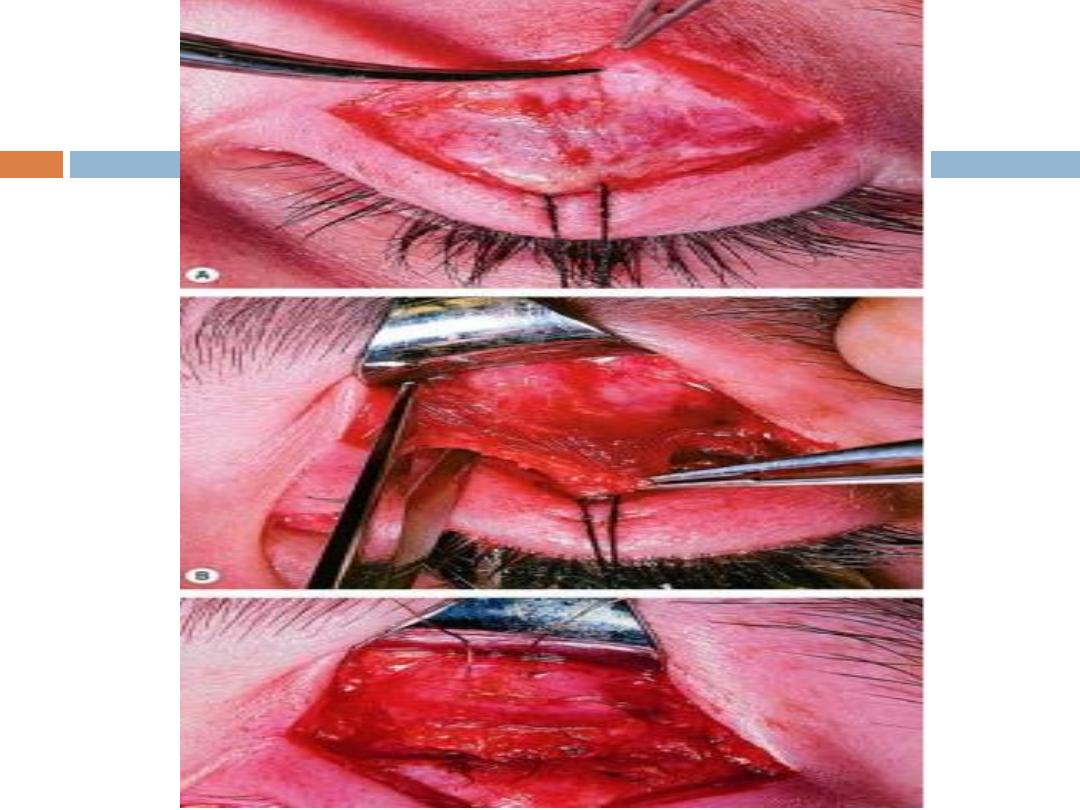
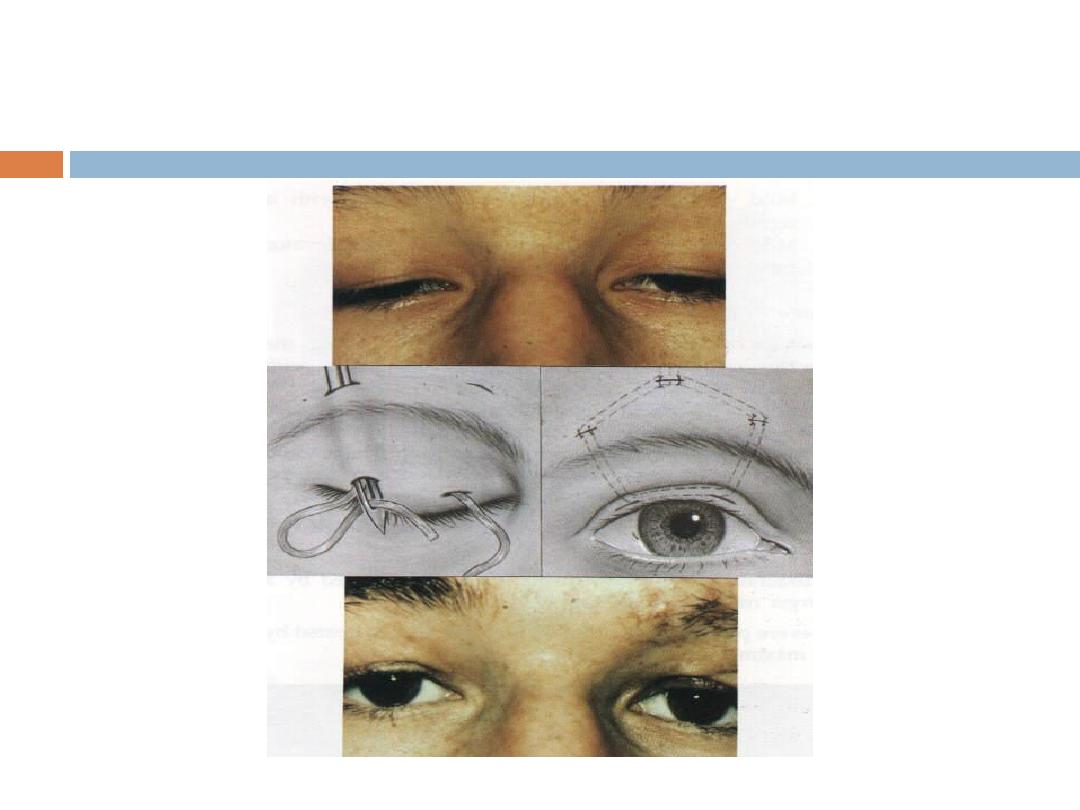
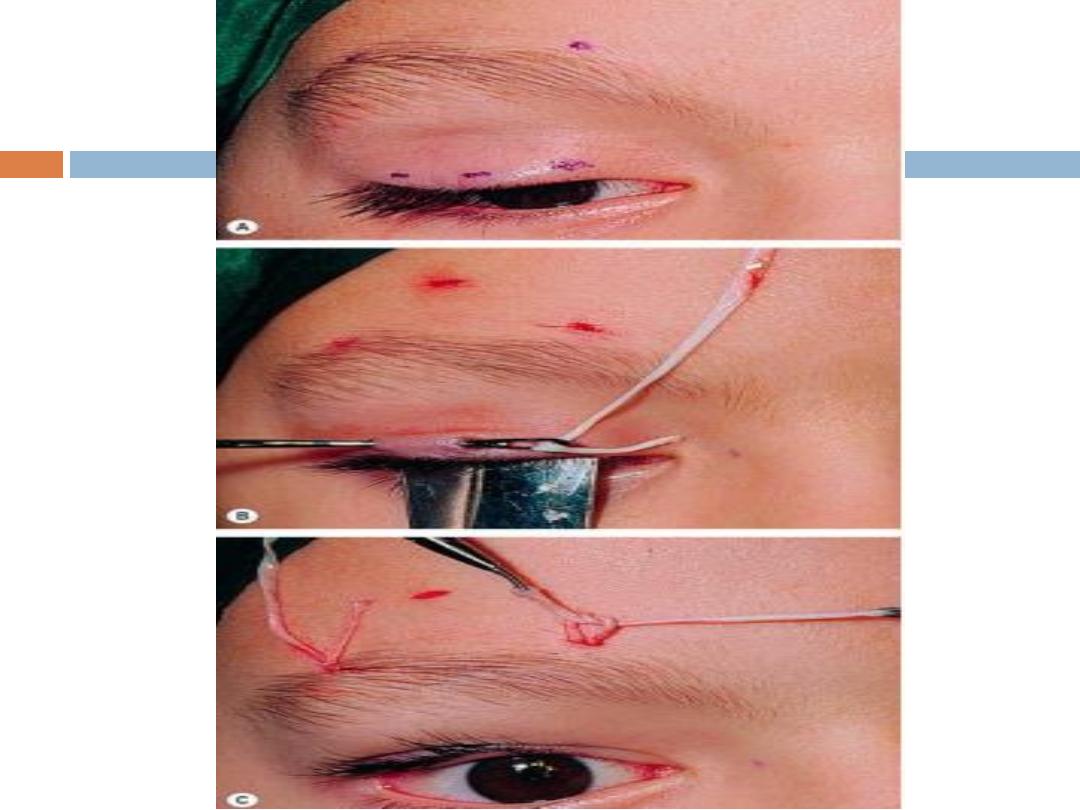
Treatment of ptosis:
The treatment is surgical except in
myasthenia gravis, where the treatment is medical:
a-
Levator resection
.
b-
Frontalis brow suspension
(Sling operation).
c-
Tarso-conjunctival resection
(Fasanella Servate
procedure).
a-
Levator resection
.
b-
Frontalis brow suspension
(Sling operation).
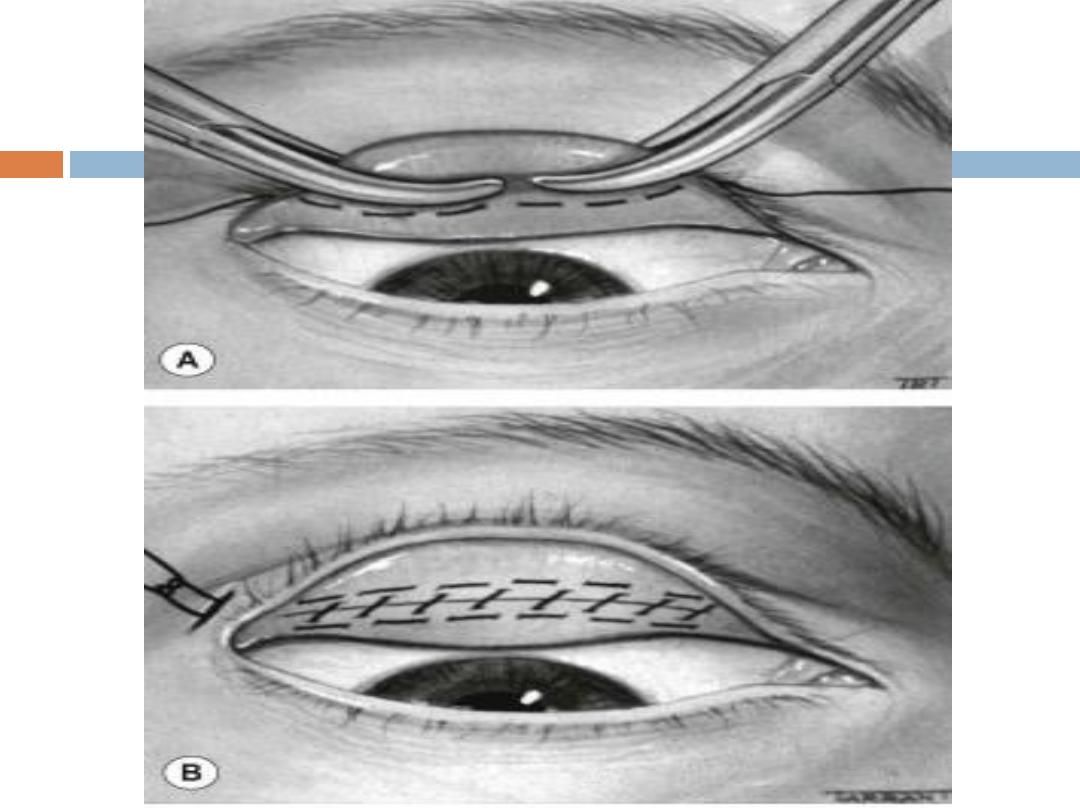
c-
Tarso-conjunctival resection
4- Trichiasis:
a-
Any cause leads to entropion of the eyelid
Pseudo-
trichiasis.
b-
Trachoma with or without entropion
True or pseudo-
trichiasis.
c-
Chronic Ant. blepharitis
True trichiasis.

Treatment:
For isolated misdirection cilia (true
trichiasis)
a-
Epilation:
Repeated every few weeks.
b-
Electrolysis
: Destruction to hair follicles by
cauterization.
c-
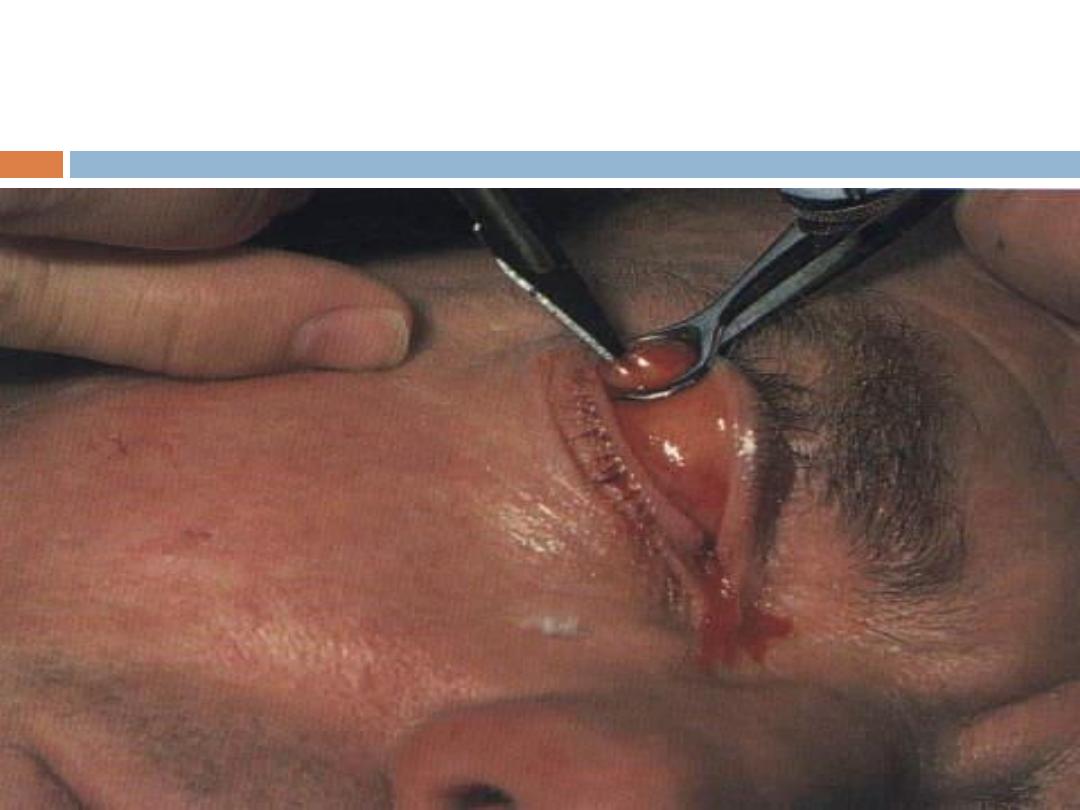
Cryosurgery:
Destruction to hair follicles by
freezing.
d-
Laser ablation:
Destruction to hair follicles by
laser.
Treatment
for pseudo-trichiasis
correction of entropion surgically.
5- Blepharospasm:
Involuntary sustained closure of the eyelids which
occurs spontaneously
(essential)
or by sensory
stimuli
(reflex)
.
6- Madarosis:
Local Causes:
chronic blepharitis, burns, radiation
and infiltrating tumor.
Systemic causes:
generalized alopecia, psoriasis,
SLE, syphilis and leprosy.

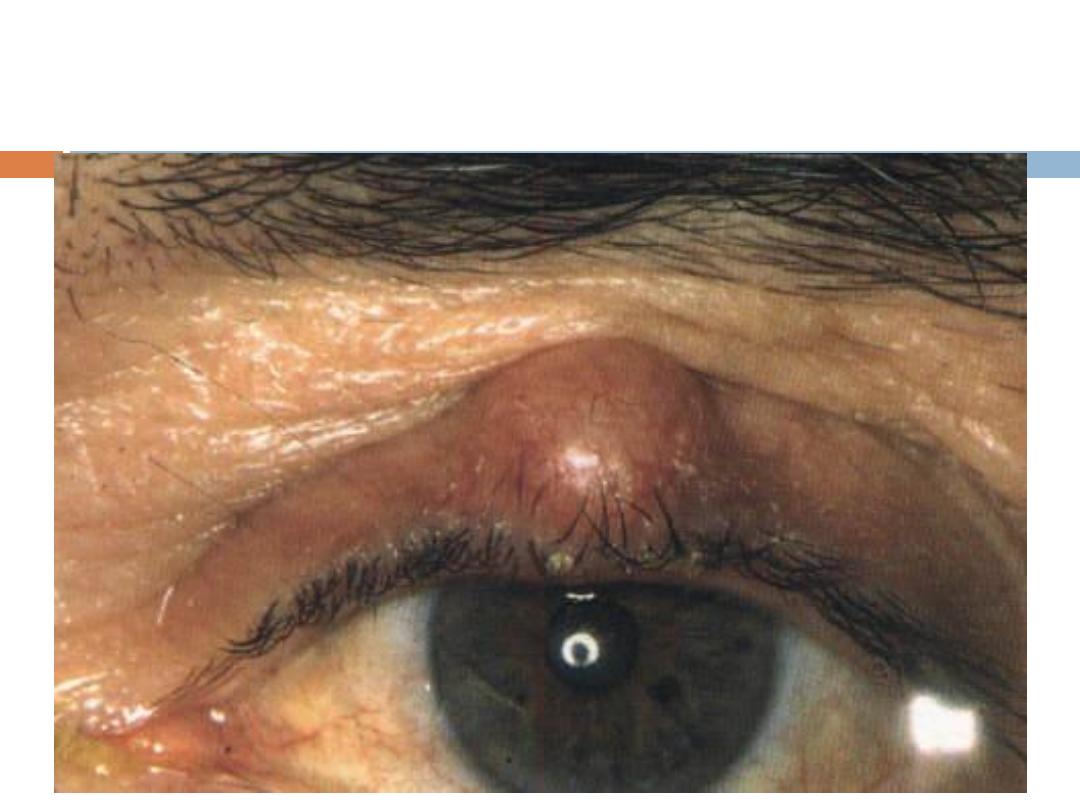
1- Chalazion (Meibomian cyst):
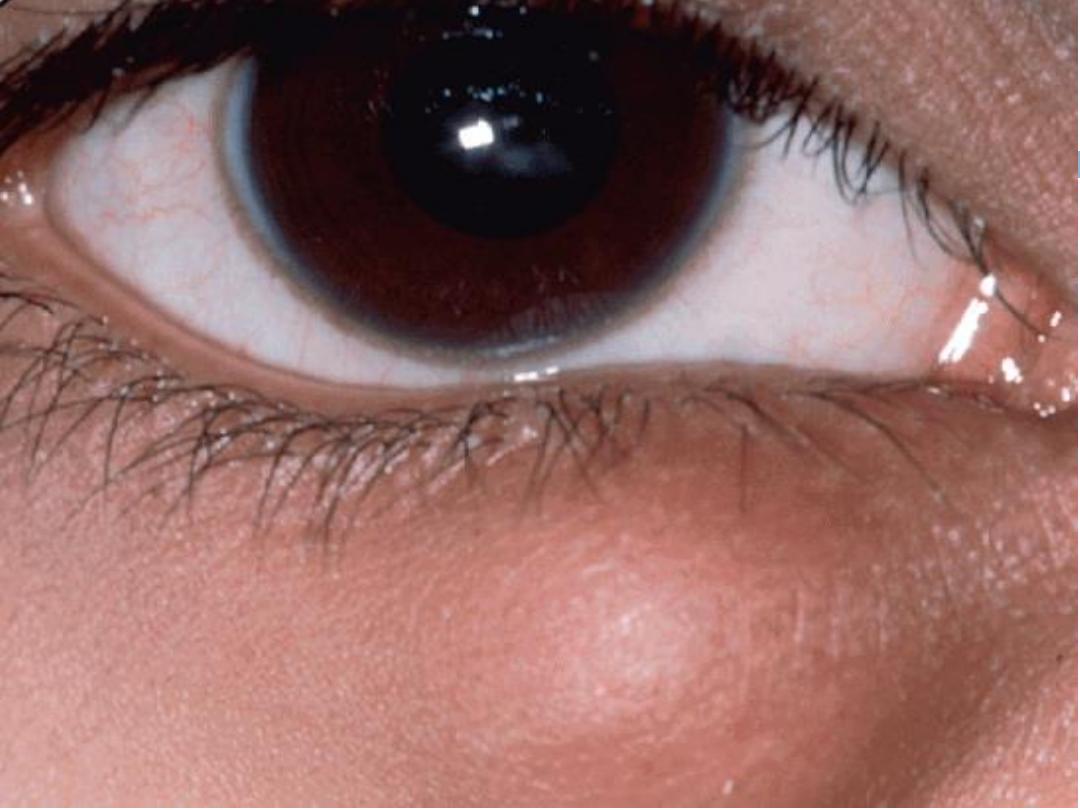
Chalazion (Meibomian cyst):
1- Chalazion (Meibomian cyst):

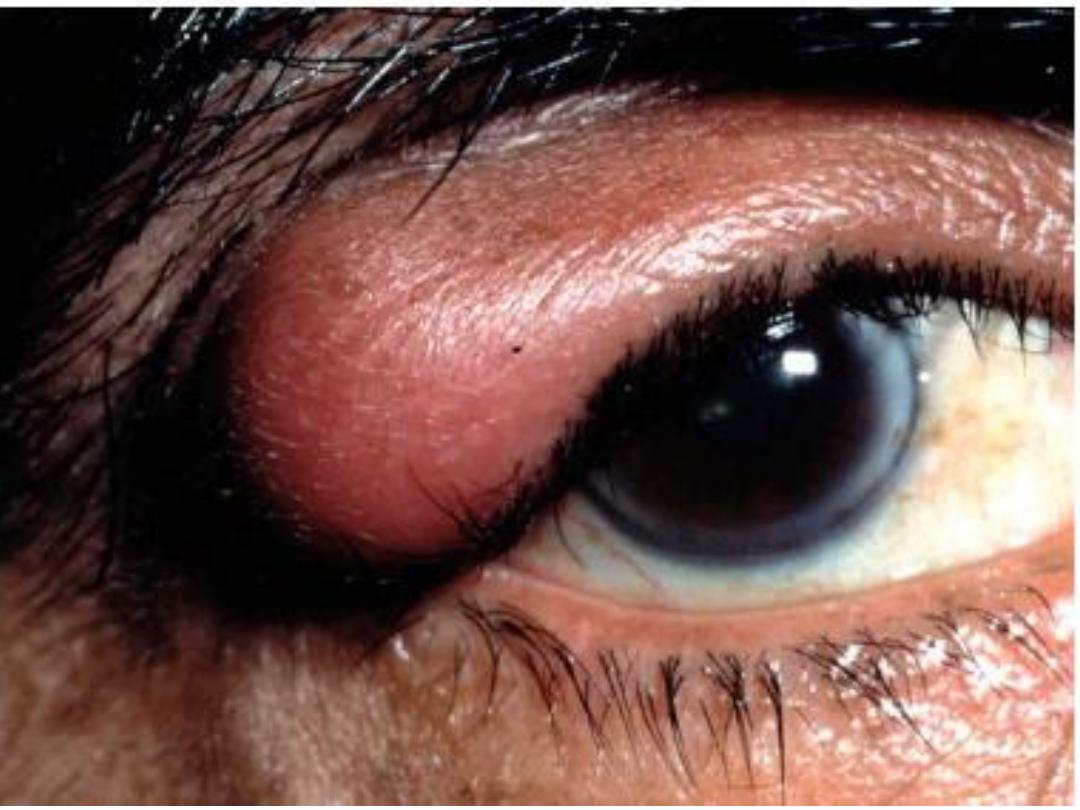
2- Internal Hordeolum:
It is a small abscess caused by an acute
staphylococcal infection of Meibomian glands.

3- External hordeolum (Stye):
Marginal Chronic Blepharitis
Types of chronic blepharitis:
1- Anterior:
a- Staphylococcal infection.
b- Seborrheic dysfunction.
c- Mixed.
2- Posterior:
a- Meibomianitis.
b- Meibomian seborrhea.
3- Mixed
Pathogenesis of chronic blepharitis:
1- Anterior chronic staphylococcal blepharitis:
2- Anterior chronic seborrhoeic blepharitis:
Neutral lipids break
down by
mycobacterium acne
in to
Bacterial lipase
and
irritating fatty
acids
responsible for increase of symptoms.
3- Posterior chronic blepharitis
down
broken
acnes
erium
Corynebact
Symptoms of chronic marginal blepharitis:
Burning
grittiness
mild photophobia
crusting and redness of the lid margin.
The symptoms are characterized by
remissions and
exacerbations
. The symptoms usually worse
in
mornings.
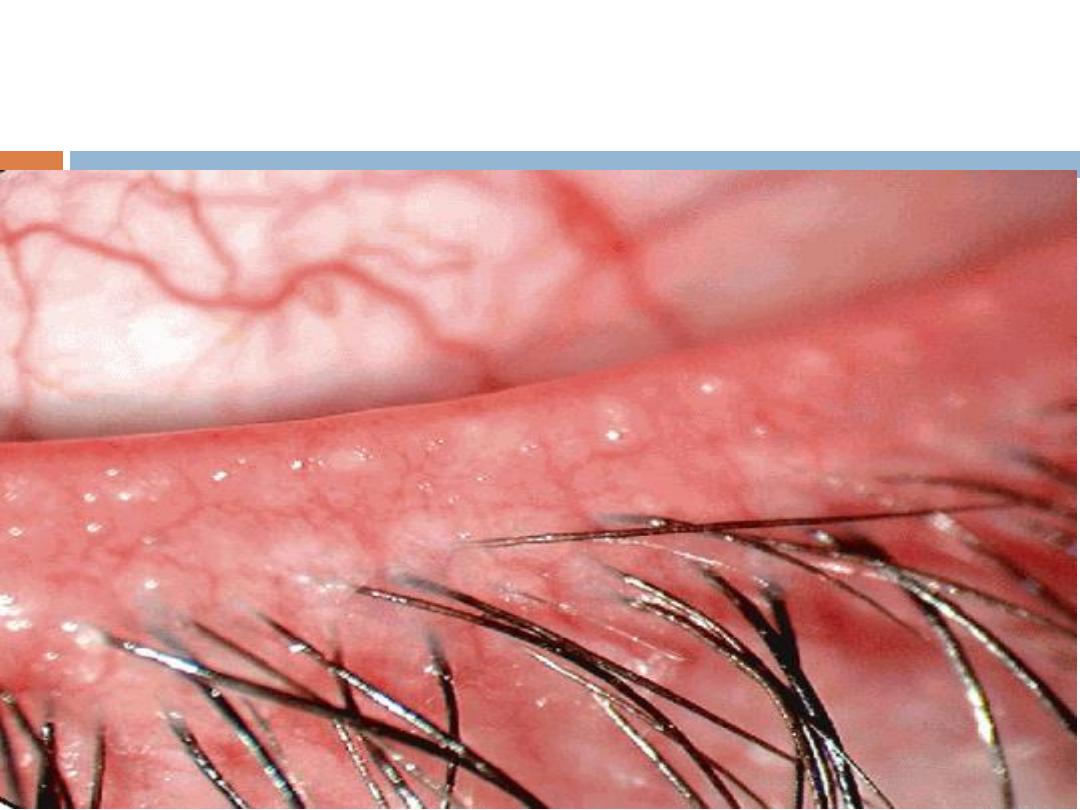
Signs of anterior blepharitis:
Hyperaemia
Telangiectasia
.
Intrafollicular abscess may be present
(staphylococcal blepharitis).
In longstanding cases the lid margin became scarred
and hypertrophied, trichiasis, madarosis and
occasionally poliosis (whitening of the eyelashes) will
occur.
Scales:
Two types of scales:
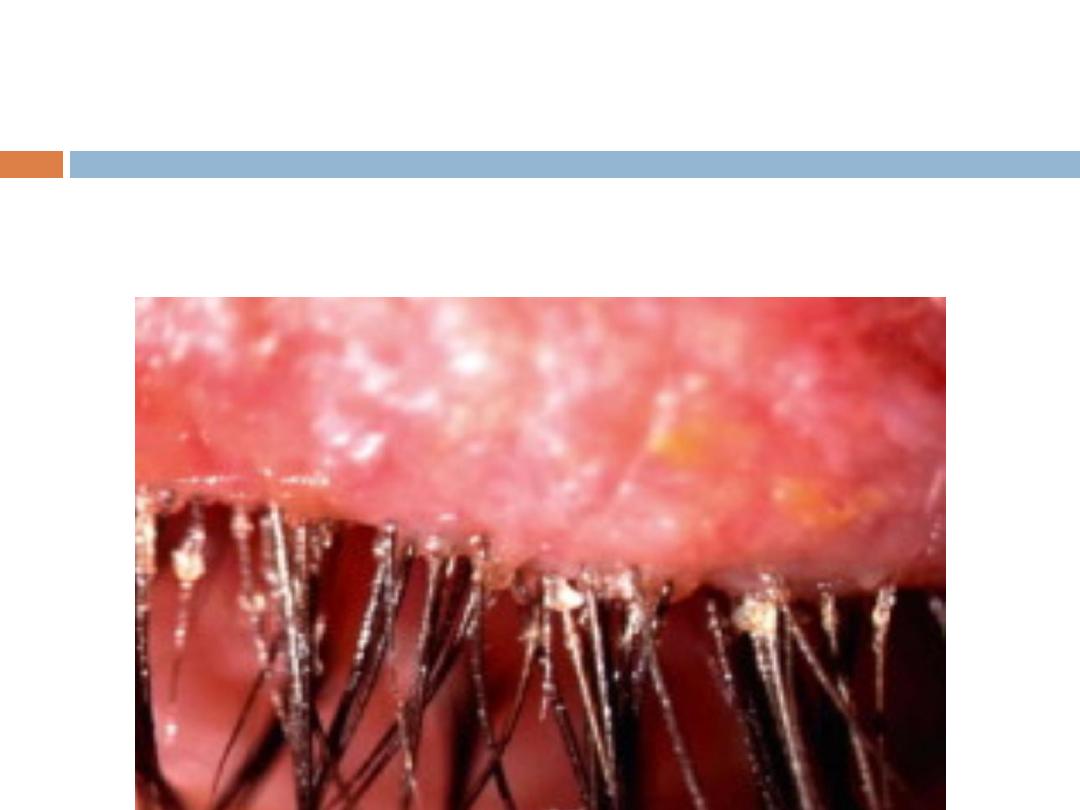
i- Staphylococcal blepharitis:
Are hard and brittle
and are centered around the lashses (collarettes).
Two types of scales:
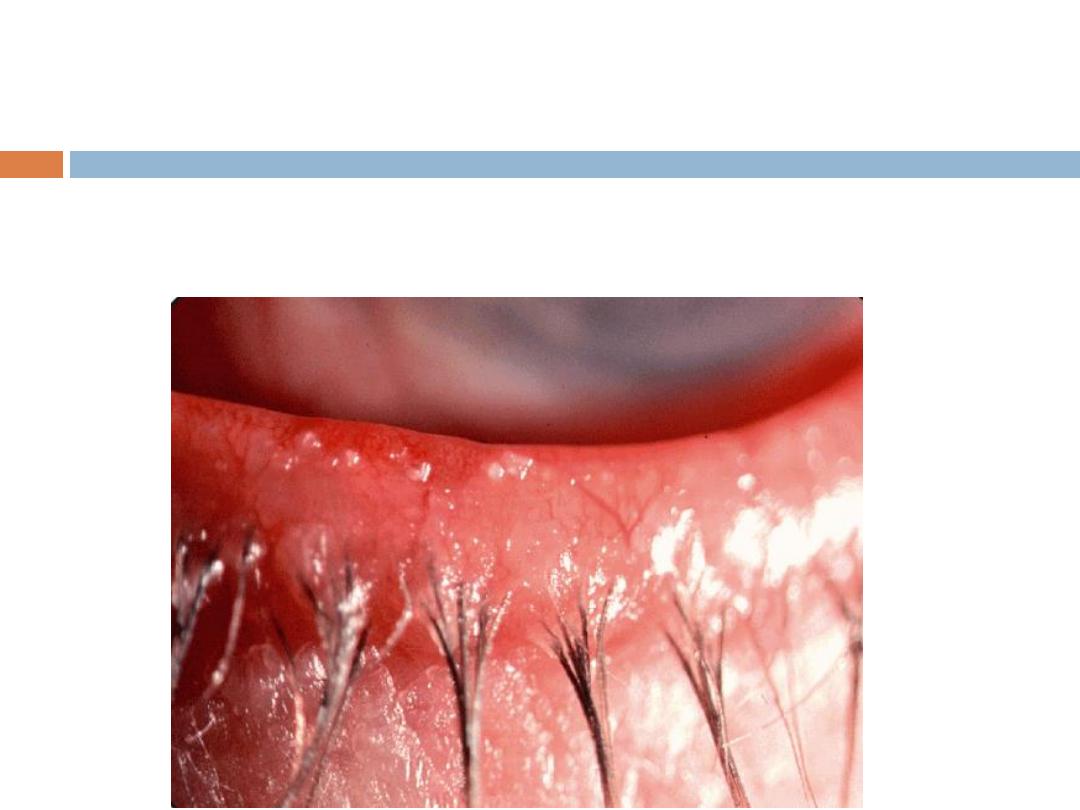
ii- Seborrhoeic blepharitis:
Are soft and greasy and
located anywhere on lid margin or on the lashes.
Complications of anterior blepharitis:
a- External hordeolum (stye).
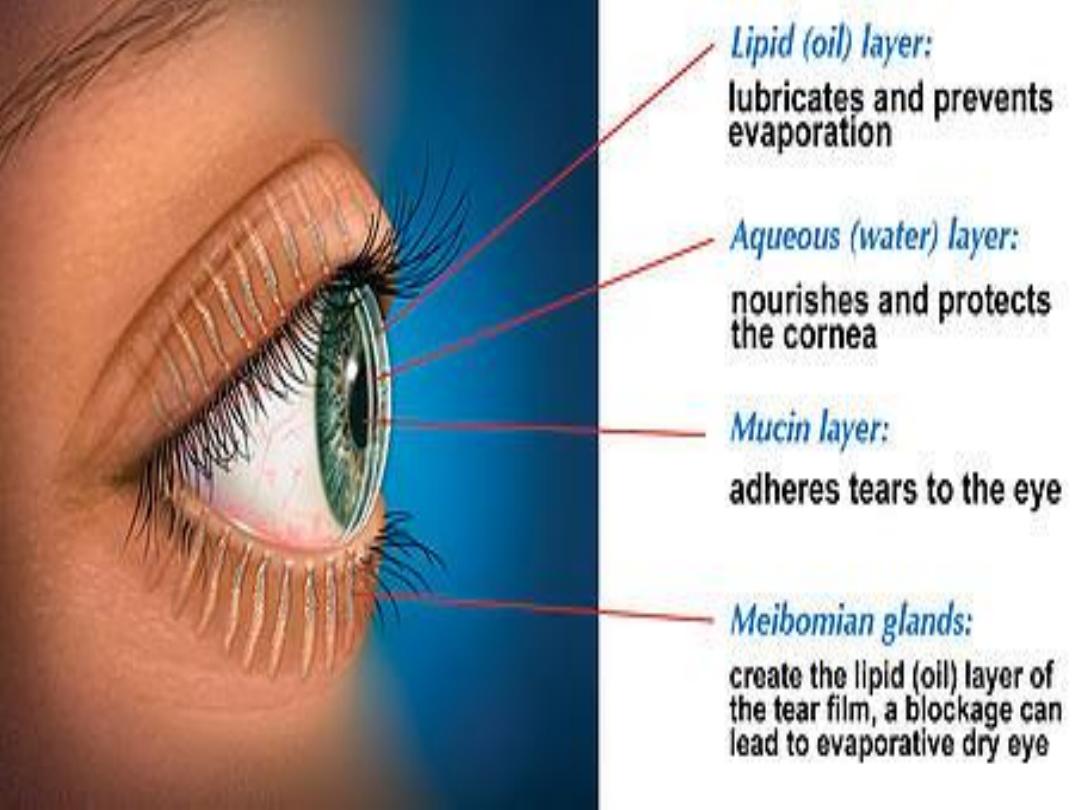
b- Tear film instability
c- Hypersensitivity to staphylococcal exotoxins
papillary conjunctival reaction, punctuate
epitheliopathy and marginal keratitis.
d- Lid margin may became scarred and
hypertrophied, trichiasis, madarosis and occasionally
poliosis (whitening of the eyelashes)
Treatment:
a- Lid hygiene:
b- Topical antibiotic ointment: fusidic acid or
chloramphenicol.
c- Weak topical steroids:
d- Tear substitutes.
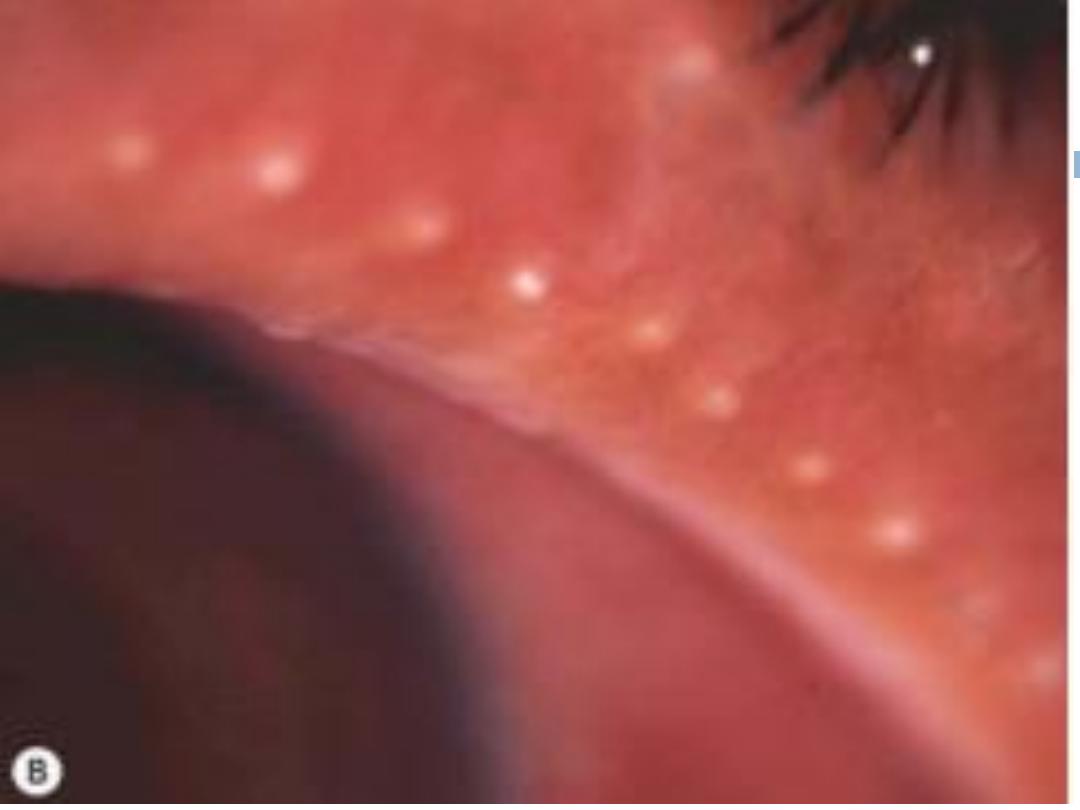
Signs of posterior blepharitis
a- Small oil globules.
b-Abnormal toothpaste like meibomian oil.
c- diffuse or localized inflammation centered around
meibomian gland orifices.
d- Blockage of the main meibomian ducts
e- Frothy secretion at lid margins & ocular canthi.
Signs of posterior blepharitis


Complications of Post. blepharitis:
a- Tear film instability & dry eyes.
b- Papillary conjunctivitis plus punctuate
epitheliopathy.
c- Internal hordeolum.
d- chalazia.
Treatment:
a- Systemic tetracyclines (as they affect Corynebacterium
acnes) for 6-12 weeks:
c- Lid hygiene.
d- Topical steroids.
e- Tear substitutes.
f- Warm compresses to melt solidified sebum and
mechanical expression (to evacuate meibomian glands from
their contents).
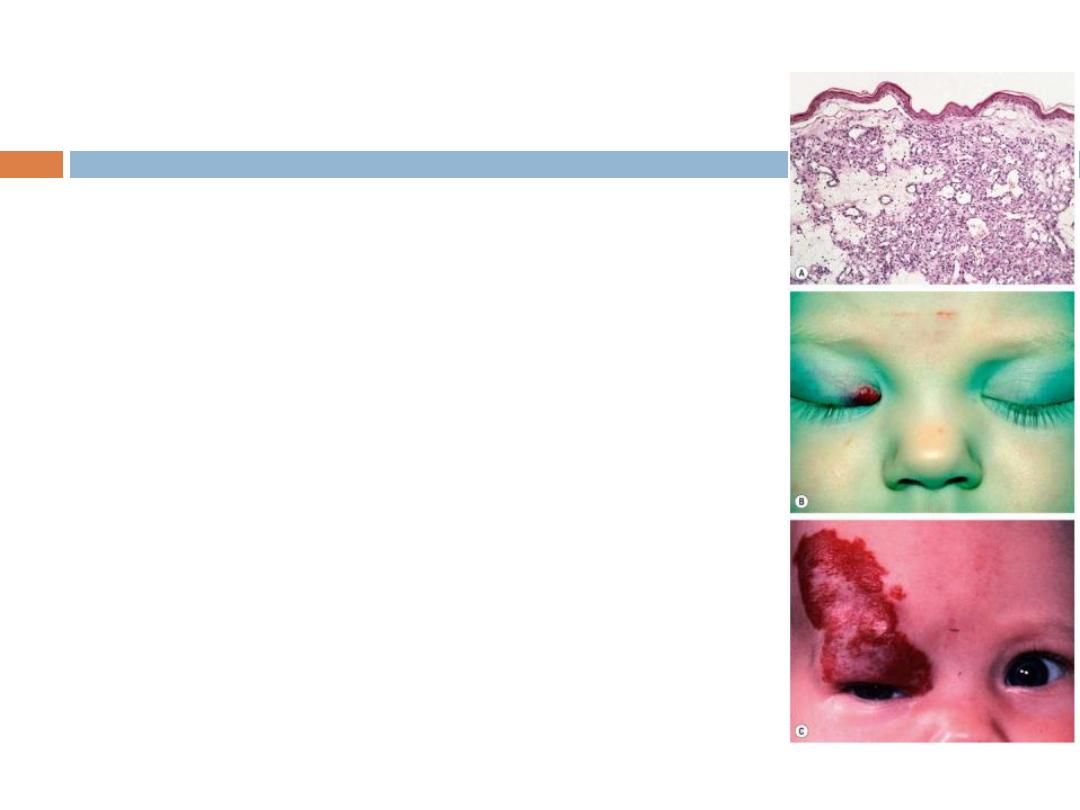
Benign tumours
Capillary haemangioma
.
Pyogenic granuloma
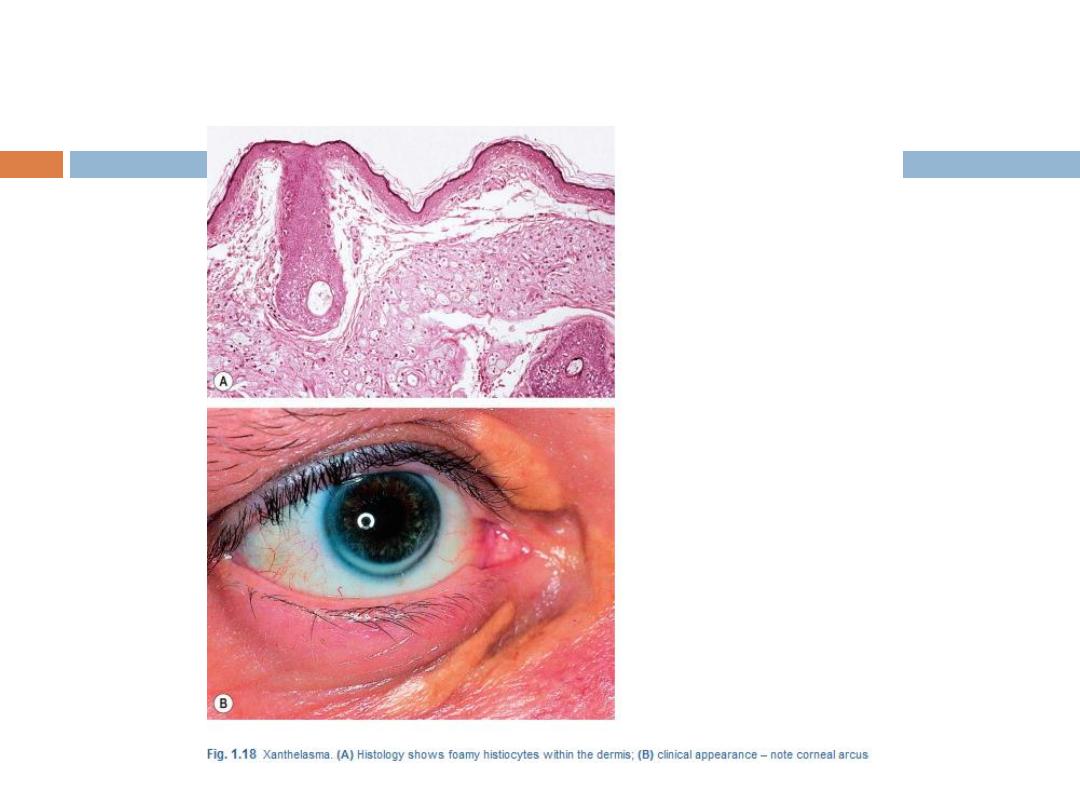
Xanthelasma
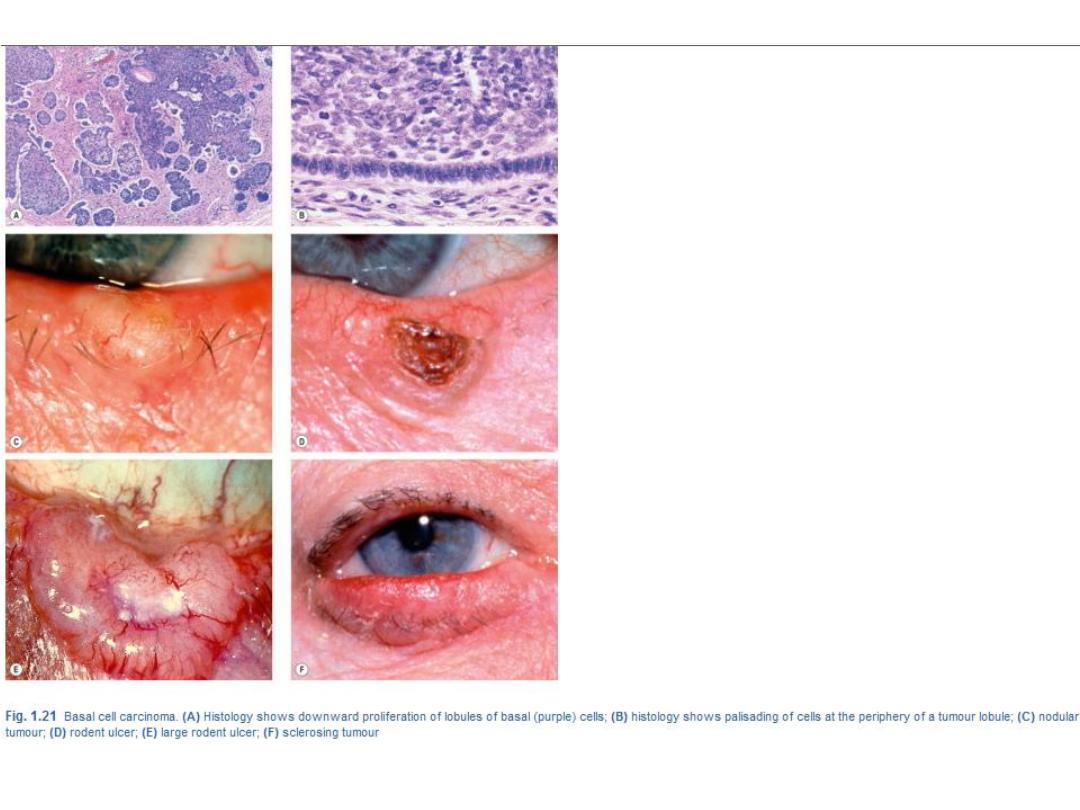
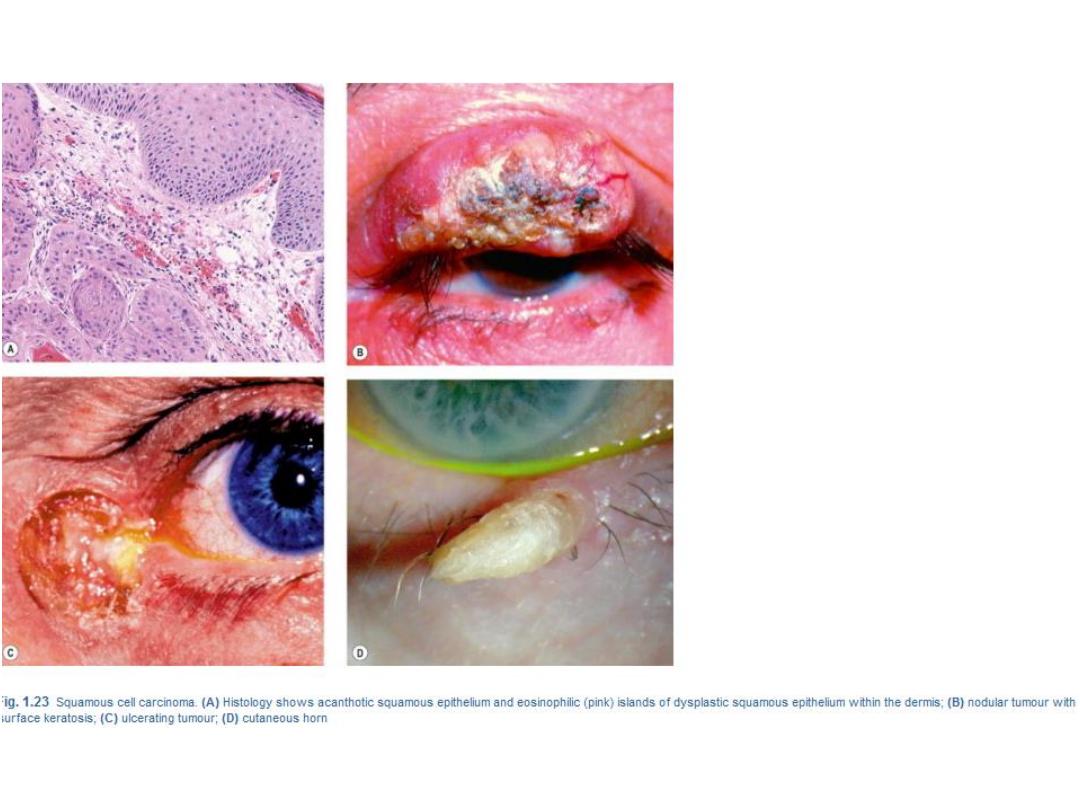
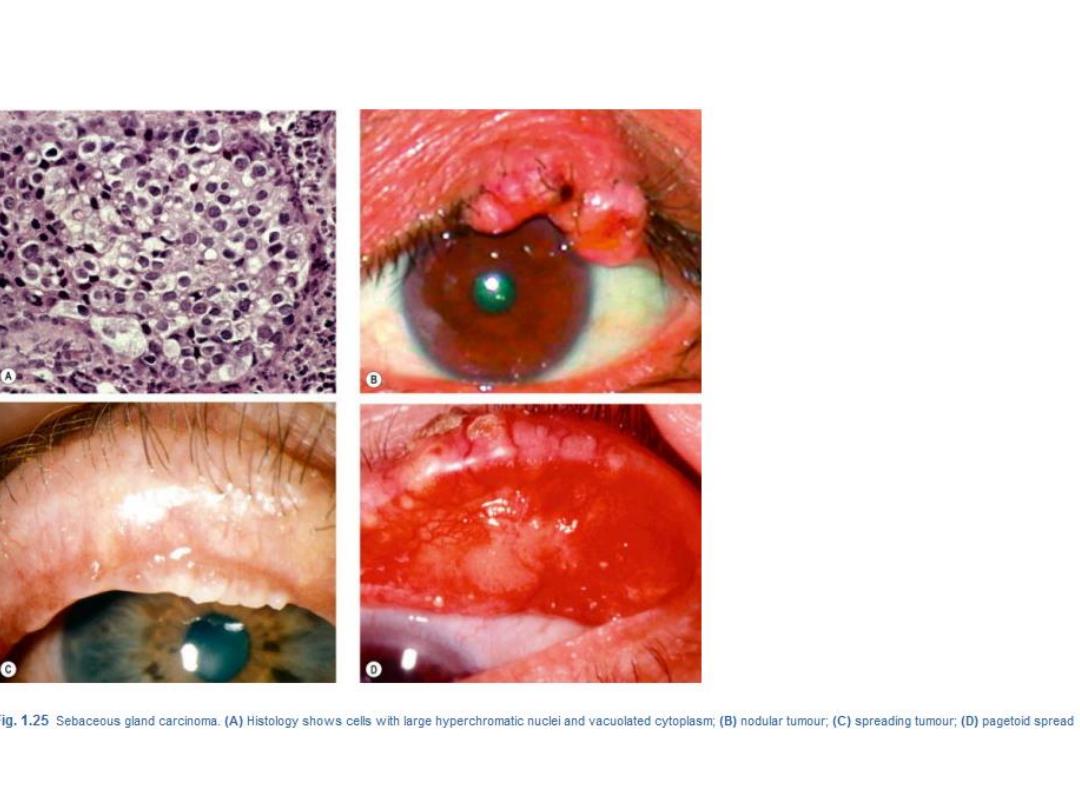
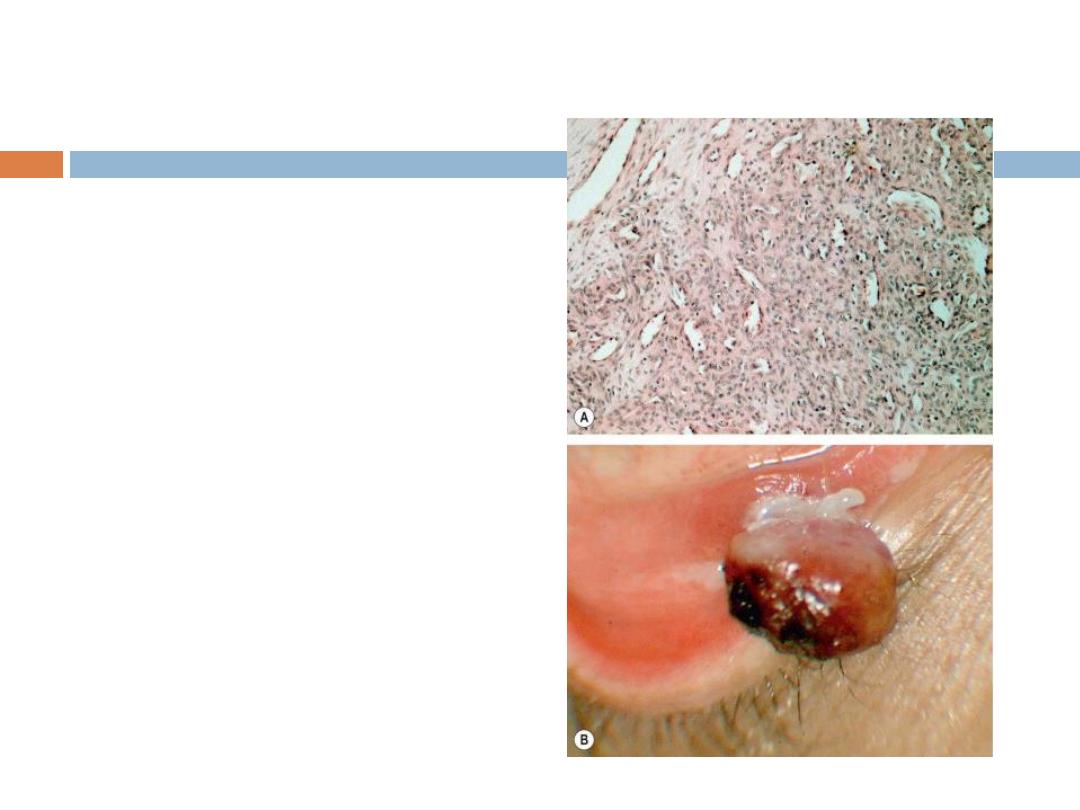
Malignant tumours
Predisposing conditions
General: old age, sun exposure, irradiation,
immune suppression, smoking, fair skin,
Scandinavian ancestry.
Rare:Young patients who suffer from one of
the following conditions may develop eyelid
malignancie
s: