VASCULITISpart 1
Dr. Ali Abdul-Rahman YounisRHEUMATOLOGIST(FIBMS)
VASCULITIS
These are a heterogeneous group of diseases characterized by inflammation and necrosis of bloodvessel walls, with associated damage to skin, kidney, lung, heart, brain and gastrointestinal tract.There is a wide spectrum of involvement and disease severity, ranging from mild and transient disease affecting only the skin, to lifethreatening fulminant disease with multiple organ failure.
VASCULITIS
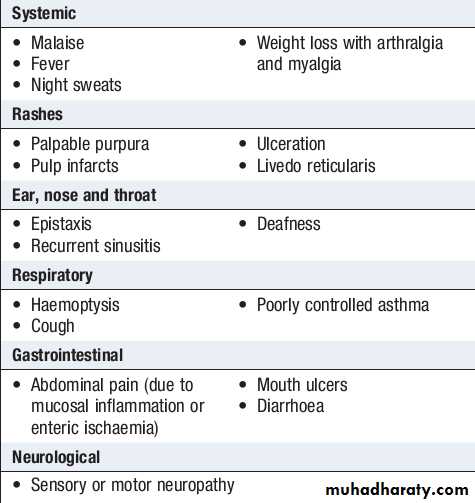
The clinical features result from a combination of local tissue ischaemia (due to vessel inflammation and narrowing) and the systemic effects of widespread inflammation.Systemic vasculitis should be considered in any patient with fever, weight loss, fatigue, evidence of multisystem involvement, rashes, raised inflammatory markers and abnormal urinalysis.
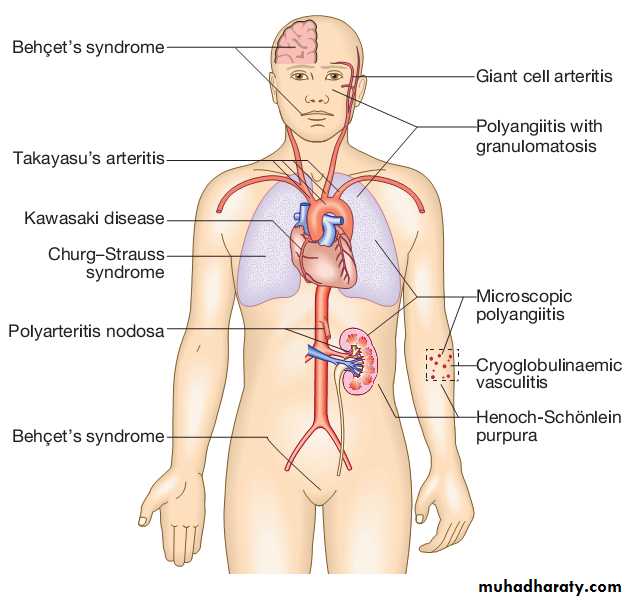
The anatomical targets of different forms of vasculitis are shown
Clinical features of systemic vasculitis
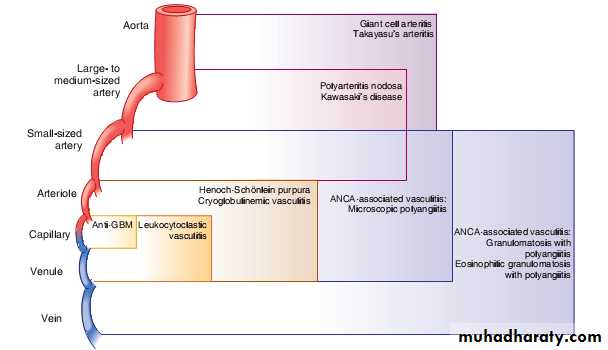
Primary vasculitis
• Large vessel –giant cell arteritis ,Takayasu’s arteritis• Medium vessel –classical polyarteritis nodosa ,Kawasaki disease
• Small vessel –microscopic polyangiitis ,wegner’s granulomatosis ,Churg-Strauss syndrome ,Henoch –Schonlein purpura ,mixed essential cryoglobulinaemia
• Drug induced vasculitis
• Serum sickness• Vasculitis associated with other primary disorders
• Infection –HBV ,HCV
• Malignancy
• Rheumatic diseases –SLE ,RA
• Endocarditis
Secondary Vasculitis
Takayasu’s disease
Takayasu’s disease predominantly affects the aorta, its major branches and occasionally the pulmonary arteries.
The typical age at onset is between 25 and 30 years, with an 8 : 1 female preponderance.
It has a worldwide distribution but is most common in Asia.
Takayasu’s is characterised by granulomatous inflammation of the vessel wall, leading to vessel occlusion or weakening of the vessel wall.
Clinical features
It presents with claudication, fever, arthralgia and weight loss.The vessels most commonly affected are the aorta and carotid, ulnar, brachial, radial and axillary arteries.
Clinical examination may reveal loss of pulses, bruits, hypertension and aortic incompetence.
Investigations
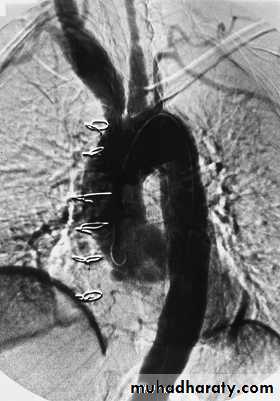
Investigations will identify an acute phase response and normocytic, normochromic anaemia.The diagnosis is based on angiography, which reveals coarctation, occlusion and aneurysmal dilatation.
The distribution of involvement is classified into four types:
• type 1: localised to the aorta and its branches
• type 2: localised to the descending thoracic and abdominal aorta
• type 3: combines features of 1 and 2
• type 4: involves the pulmonary artery.
Angiogram showing multiple changes of Takayasu’s
arteritis including dilation of the aortic root (with surgical wires from previous aortic valve replacement), aneurysmal dilation of the innominate and right carotid arteries, and occlusion of the distal left common carotid artery
Angiogram showing bilateral renal artery stenosis.
TreatmentTreatment is with high dose steroids and immunosuppressants.
With appropriate treatment, the 5 year survival is 83%.
Giant cell arteritis and polymyalgia rheumatica
Giant cell arteritis (GCA) is a granulomatous arteritis that predominantly affects medium sized arteries in the head and neck.It is commonly associated with polymyalgia rheumatica (PMR), which presents with symmetrical muscle pain and stiffness affecting the shoulder and pelvic girdles.
Since many patients with GCA have symptoms of PMR, and many patients with PMR go on to develop GCA if untreated, many rheumatologists consider them to be different manifestations of the same underlying disorder.
Giant cell arteritis and polymyalgia rheumatica
Both diseases are rare under the age of 60 years. The average age at onset is 70, with a female preponderance of about 3 : 1.The overall prevalence is about 20 per 100 000 in those over the age of 50 years.
Clinical features
The cardinal symptom of GCA is headache, which is often localized to the temporal or occipital region and may be accompanied by scalp tenderness.
Jaw pain develops in some patients, brought on by chewing or talking, due to ischaemia of the masseter muscles.
Visual disturbance can occur and a catastrophic presentation is with blindness in one eye due to occlusion of the posterior ciliary artery. On fundoscopy, the optic disc may appear pale and swollen with haemorrhages, but these changes may take 24–36 hours to develop and the fundi may initially appear normal.
Other visual symptoms include loss of visual acuity, reduced color perception and papillary defects.
Rarely, neurological involvement may occur, with transient ischaemic attacks, brainstem infarcts and hemiparesis.
Clinical features
The cardinal features of PMR are symmetrical muscle pain and stiffness affecting the shoulder and pelvic girdles.Constitutional symptoms, such as weight loss, fatigue, malaise and night sweats, are common.
The onset of symptoms is usually fairly sudden over a few days, but may be more insidious.
On examination, there may be stiffness and painful restriction of active shoulder movement but passive movements are preserved. Muscles may be tender to palpation but weakness and muscle wasting are absent.
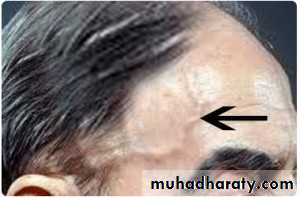
Giant cell arteritis (GCA) involving the temporal artery.
Short segments of curved artery were erythematous and tender (long arrows). The bandage on the scalp covers a similar artery that was biopsied and showed GCA. A previous biopsy specimen of a proximal segment of the right temporal artery, which was normal on physical examination, was normal histologically. The faint scar from that biopsy can be seen above and anterior to the right ear (short arrows).Thick, pulseless temporal artery
ophthalmoscopic appearance of the acute phase of anterior ischemic optic neuropathy seen in patients with giant cell arteritis
and loss of vision. The optic disc is pale and swollen, the retinal veins are dilated, and several flame-shaped hemorrhages and a cotton-wool spot (retinal infarct) are visible.
Investigations
The typical laboratory abnormality is an elevated ESR, often with a normochromic, normocytic anaemia. CRP may also be elevated and in some cases this precedes elevation of the ESR. Rarely, PMR and GCA can present with a normal ESR.The diagnosis is usually based on a combination of the typical clinical features, raised ESR and prompt response to steroid.
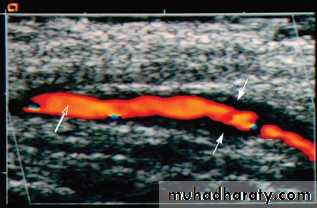
More objective evidence for GCA should be obtained whenever possible. There are three investigations to consider: temporal artery biopsy, ultrasound of the temporal arteries and 19 fluorodeoxyglucose positron emission tomography (19FDG PET scan).
Characteristic biopsy findings are fragmentation of the internal elastic lamina with necrosis of the media in combination with a mixed inflammatory cell infiltrate.
Investigations
Diagnostic yield is highest with multiple biopsies and multiple section analysis (to detect ‘skip’ lesions). A negative biopsy does not exclude the diagnosis.On ultrasound examination, affected temporal arteries show a ‘halo’ sign.
A strongly positive 19FDG PET scan is highly specific but sensitivity is low.
Caution is needed in interpreting weakly positive images. Low-grade vascular uptake may occur in atheromatous arterial disease.
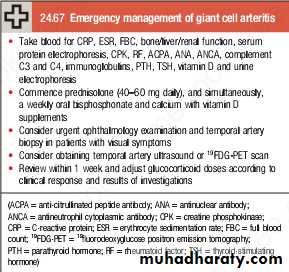
Management
Corticosteroids are the treatment of choice and should be commenced urgently in suspected GCA because of the risk of visual loss.Response to treatment is dramatic, such that symptoms will have completely resolved within 48–72 hours of starting corticosteroid therapy in virtually all patients.
It is customary to use higher doses in GCA (60–80 mg prednisolone) than in PMR (15–30 mg), although the evidence base for this is weak.
In both conditions the steroid dose should be progressively reduced, guided by symptoms and ESR, with the aim of reaching a dose of 10–15 mg by about 8 weeks. Thereafter, the rate of reduction should be slower – by 1 mg per month – until an acceptable dose is achieved (5–7.5 mg daily).
Management
If symptoms recur, the dose should be increased to that which previously controlled the symptoms, and reduction attempted again in another few weeks. Most patients need steroids for an average of 12–24 months.Some patients also require steroid sparing agents, such as methotrexate or azathioprine, if they require a maintenance dose of prednisolone of more than 7.5 mg daily. Prophylaxis against osteoporosis should be given in patients with low BMD.