Autoimmune Connective Tissue DiseasesPart 1(SLE)
Dr. Ali Abdul-Rahman YounisRHEUMATOLOGIST(FIBMS)
CONNECTIVE TISSUE DISEASES
CTD are group of chronic inflammatory disorders that involve multiple body systems and therefore exhibit a wide spectrum of clinical manifestations .These share overlapping clinical features, characterized by :
• dysregulation of immune responses.
• autoantibody production often directed at components of the cell nucleus.
• widespread tissue damage.
systemic lupus erythematosus
Systemic lupus erythematosus (SLE) is a rare disease with a prevalence that ranges from about 0.03% in Caucasians to 0.2% in AfroCaribbeans.Some 90% of affected patients are female and the peak age at onset is between 20 and 30 years.
Lupus is associated with considerable morbidity and a fivefold increase in mortality compared to age and gender matched controls, mainly because of an increased risk of premature cardiovascular disease.
Pathophysiology
The cause of SLE is incompletely understoodGenetic factors play an important role.
There is a higher concordance in monozygotic twins.
The disease is strongly associated with polymorphic variants at the HLA locus.
In a few instances, SLE is associated with inherited mutations in complement components C1q, C2 and C4, in the immunoglobulin receptor FcγRIIIb or in the DNA exonuclease TREX1.
Pathophysiology
From an immunological standpoint, the characteristic feature of SLE is autoantibody production.
These autoantibodies have specificity for a wide range of targets but many are directed against antigens present within the cell or within the nucleus.
This has led to the hypothesis that SLE may occur because of defects in apoptosis or in the clearance of apoptotic cells, which causes inappropriate exposure of intracellular antigens on the cell surface, leading to polyclonal B and Tcell activation and autoantibody production.
This is supported by the fact that environmental factors that cause flares of lupus, such as UV light and infections, increase oxidative stress and cause cell damage.
Whatever the underlying cause of the autoantibody production, immune complex formation is thought to be an important mechanism of tissue damage in active SLE, leading to vasculitis and organ damage.
Clinical features
Symptoms such as fever, weight loss and mild lymphadenopathy may occur during flares of disease activity.Other symptoms such as fatigue, malaise and fibromyalgia like symptoms can be constant and not particularly associated with active inflammatory disease.
Musculoskeletal features
Arthralgia is a common symptom, occurring in 90% of patients, and is often associated with early morning stiffness.Tenosynovitis may also occur.
Polyarthritis –non erosive ,small joints of hand and wrist, deformities are uncommon.
Clinically apparent synovitis with joint swelling is rare.
Joint deformities may occur (Jaccoud’s arthropathy) as the result of tendon damage, but joint erosions do not occur.
Raynaud’s phenomenon
Raynaud’s syndrome is common and may antedate other symptoms by months or years.A common presentation is Raynaud’s in combination with arthralgia or arthritis.
Raynaud’s associated with SLE and other connective tissue disease needs to be differentiated from primary Raynaud’s, which is common in healthy young women.
Features in favor of secondary Raynaud’s include age at onset of over 25 years, absence of a family history of Raynaud’s, and occurrence in a male.
Examination of capillary nailfold loops using an ophthalmoscope (and oil placed on the skin) may help distinguish primary from secondary Raynaud’s.
Skin
Rash is common in SLE and is classically precipitated by exposure to UV light.Three distinct types occur:
- The classic butterfly facial rash (up to 20% of patients). This is erythematous, raised and painful or itchy, and occurs over the cheeks with sparing of the nasolabial folds .
-The subacute cutaneous lupus erythematosus (SCLE) rash, which is migratory, nonscarring and either annular or psoriaform.
- The discoid lupus rash characterised by hyperkeratosis and follicular plugging, with scarring alopecia if it occurs on the scalp.
Diffuse, usually nonscarring alopecia may also occur with active disease.
Other skin manifestations include periungual erythema (reflecting dilated capillary loops), vasculitis and livedo reticularis , which is also a common feature of the antiphospholipid syndrome .
Kidney
Renal involvement is one of the main determinants of prognosis.Regular monitoring of urinalysis and blood pressure is essential.
The typical renal lesion is a proliferative glomerulonephritis ,characterised by heavy haematuria, proteinuria and casts on urine microscopy.
Subclinical presentation- proteinuria only or proteinuria with haematuria
Any histologic pattern (minimal changes GN to cresentic GN)
Wide range of clinical presention(RPGN to chronic GN)
Hypocomplementic GN
Cardiovascular
The most common manifestation is pericarditis.Myocarditis and Libman–Sacks endocarditis can also occur.
The endocarditis is due to accumulation on the heart valves of sterile fibrin containing vegetations, which is thought to be a manifestation of hypercoagulability associated with antiphospholipid antibodies.
The risk of atherosclerosis is greatly increased, as is the risk of stroke and myocardial infarction. This is thought to be multifactorial due to the adverse effects of inflammation on the endothelium, chronic steroid therapy and the procoagulant effects of antiphospholipid antibodies.
Lung
Lung involvement is common and most frequently manifests as pleurisy or pleural effusion.Other features include pneumonitis, atelectasis, reduced lung volume and pulmonary fibrosis that leads to breathlessness.
The risk of thromboembolism is increased, especially in patients with antiphospholipid antibodies.
Neurological
Fatigue, headache and poor concentration are common, and often occur in the absence of laboratory evidence of active disease.
More specific features of cerebral lupus include visual hallucinations, chorea, organic psychosis, transverse myelitis and lymphocytic meningitis.
Haematological
GastrointestinalNeutropenia, lymphopenia, thrombocytopenia or haemolytic anaemia may occur, due to antibodymediated destruction of peripheral blood cells.
The degree of lymphopenia is a good guide to disease activity.
Mouth ulcers may occur and may or may not be painful.
Mesenteric vasculitis is a serious complication, which can present with abdominal pain, bowel infarction or perforation.Investigations
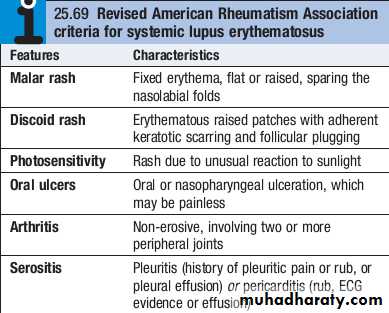
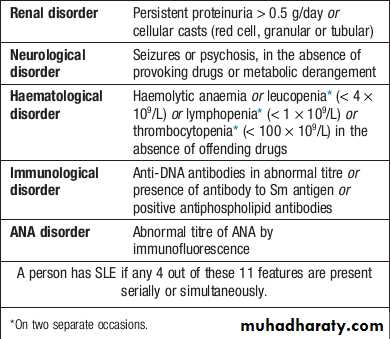
The diagnosis is based on a combination of clinical features and laboratory abnormalities.To fulfill the classification criteria for SLE, at least 4 of the 11 factors must be present or have occurred in the past.
Patients should be screened for ANA and antibodies to extractable nuclear antigens, and have complement levels checked along with routine haematology and biochemistry.
Patients with active SLE almost always test positive for ANA, but ANA negative SLE can very rarely occur in the presence of antibodies to the Ro antigen.
AntidsDNA antibodies are characteristic of severe active SLE but are positive in many, but not all, patients and are tested at the time of diagnosis by most laboratories using ELISA.
Investigations
Similarly, patients with active disease tend to have low levels of C3 and C4, but this may be the result of inherited complement deficiency that predisposes to SLE. Studies of other family members can help to differentiate inherited deficiency from complement consumption.
A raised ESR, leucopenia and lymphopenia are typical of active SLE, along with anaemia, haemolytic anaemia and thrombocytopenia.
CRP is often normal in active SLE, except in the presence of serositis, and an elevated CRP suggests coexisting infection.
Management
The therapeutic goals are to educate the patient about the nature of the illness, to control symptoms and to prevent organ damage.Patients should be advised to avoid sun and UV light exposure and to employ sun blocks (factor 25–50).
Mild to moderate disease
Patients with mild disease restricted to skin and joints can sometimes be managed with analgesics, NSAID and hydroxychloroquine (200–400 mg daily).Frequently, however, corticosteroids are also necessary (prednisolone 5–20 mg/day), often in combination with immunosuppressants such as methotrexate, azathioprine or mycophenolate mofetil (MMF).
Increased doses of steroids may be required for flares in activity or complications such as pleurisy or pericarditis.
The monoclonal antibody belimumab, which targets the βcell growth factor BLyS, has recently been shown to be effective in patients with active SLE who have responded inadequately to standard therapy.
Life-threatening disease
High dose corticosteroids and immunosuppressants are required for the treatment of renal, CNS and cardiac involvement. A commonly used regimen is pulse methyl prednisolone (10 mg/kg IV), coupled with cyclophosphamide (15 mg/kg IV), repeated at 2–3weekly intervals for six cycles.Cyclophosphamide may cause haemorrhagic cystitis, but the risk can be minimised by good hydration and coprescription of mesna, which binds its urotoxic metabolites.
Because of the risk of azoospermia and anovulation (which may be permanent), pretreatment sperm or ova collection and storage need to be considered prior to treatment with cyclophosphamide.
Mycophenolate mofetil has been used successfully in combination with highdose steroids for renal involvement in SLE, with results equivalent to those of pulse cyclophosphamide but fewer adverse effects.
The role of belimumab in lifethreatening SLE remains to be established since clinical trials of this agent excluded patients with renal and cerebral lupus
Maintenance therapy
Following control of the acute episode, the patient should be switched to oral immunosuppressive medication.
A typical regimen is to start oral prednisolone in a dose of 40–60 mg daily on cessation of pulse therapy, gradually reducing to reach a target of 10–15 mg/day or less by 3 months. Azathioprine (2–2.5 mg/kg/day), methotrexate (10–25 mg/week) or MMF (2–3 g/day) should also be prescribed.
The long term aim is to continue the lowest dose of corticosteroids and immunosuppressant that will maintain remission.
Cardiovascular risk factors, such as hypertension and hyperlipidaemia, should be controlled and patients advised to stop smoking.
Lupus patients with the antiphospholipid antibody syndrome who have had previous thrombosis require lifelong warfarin therapy.