1
Lecture (1) ENT Dr Haitham Alnori
18/12/2019 Assisstant Professor
OTOLOGY
Embryology
The auricle arises from a series of six tubercles which form around
the first visceral cleft about the sixth week of gestation. The external
auditory canal EAC arises from the ectoderm of the first visceral cleft. The
tympanic membrane has three layers; an outer epithelial layer which arises
from the ectoderm of the first visceral cleft, a middle fibrous layer arises
from the mesoderm between the first visceral cleft and the tubotympanic
recess, and inner mucosal layer arises from the endoderm of the
tubotympanic recess.
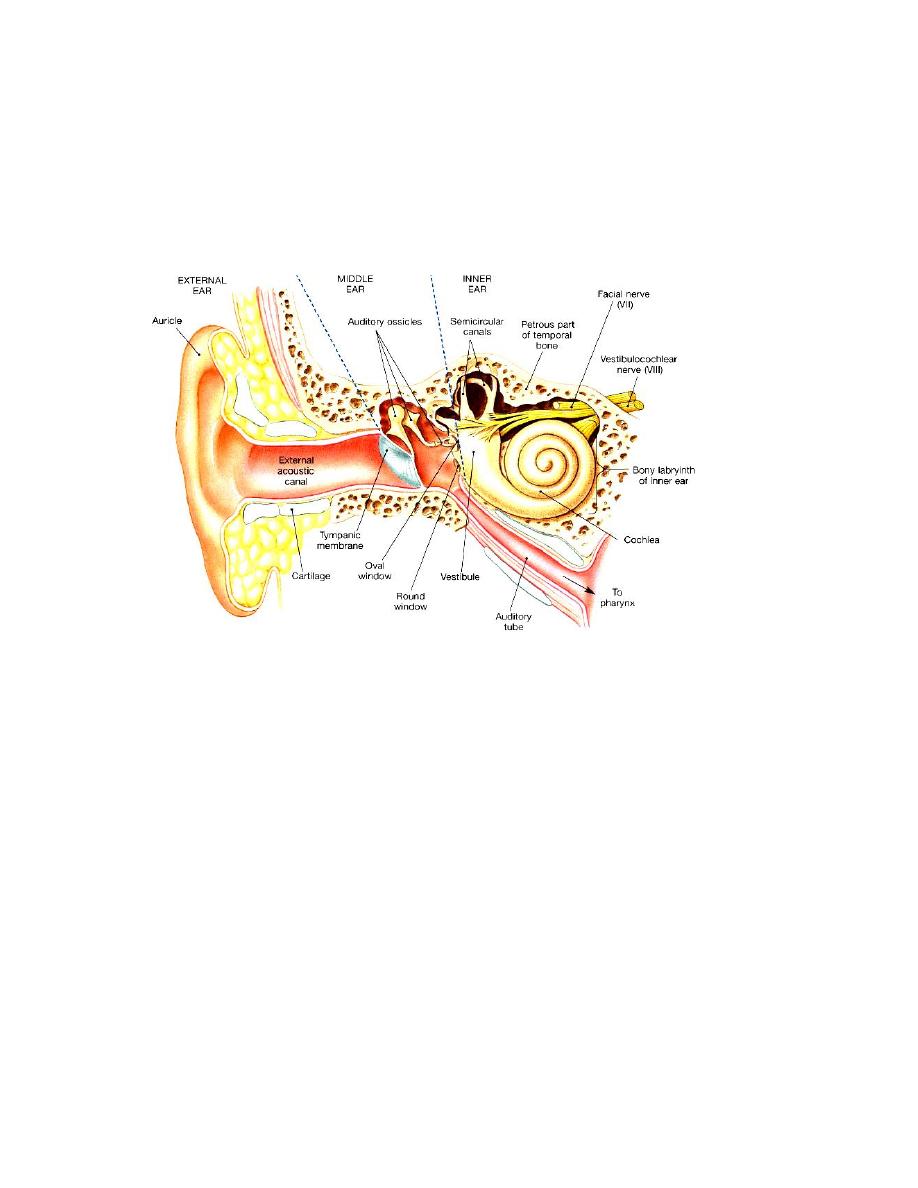
Anatomy
External Ear consists of;
1. The auricle (pinna).
2. The external canal (external auditory meatus).
The Auricle: Consists of yellow elastic cartilage except for the lobule which
is composed only of fat and fibroalveolar tissue. Skin on the lateral surface
2
is closely adherent to the perichondrium. The auricle is attached to the side
of the head by ligaments and rudimentary muscles.
Parts of the auricle: Helix, Antihelix, Tragus, Antitragus, Concha and Lobule.
External Acoustic Meatus ( External Auditory Canal)
In adults it measure about 2.5 cm, the outer third is cartilaginous and the
inner two thirds are bony. The sebaceous glands, hair follicles and
ceruminous glands (which secrete wax) are present only in the cartilaginous
portion. Skin is tightly adherent to the underlying cartilage.
Δ
Clinical Point: "Medical" ear sticks are not medical! They just act to
impact wax near the T.M.!
In adult there is an angle in the meatus, accordingly the pinna must be pulled
upwards, backwards and outwards when using a speculum to examine the ear
drum.
Nerve Supply: Rich nerve supply including branches of the 5
th
, 9
th
and 10
th
cranial nerves in addition to fibers of the great auricular nerve (C2 and C3)
and the lesser occipital nerve (C2).
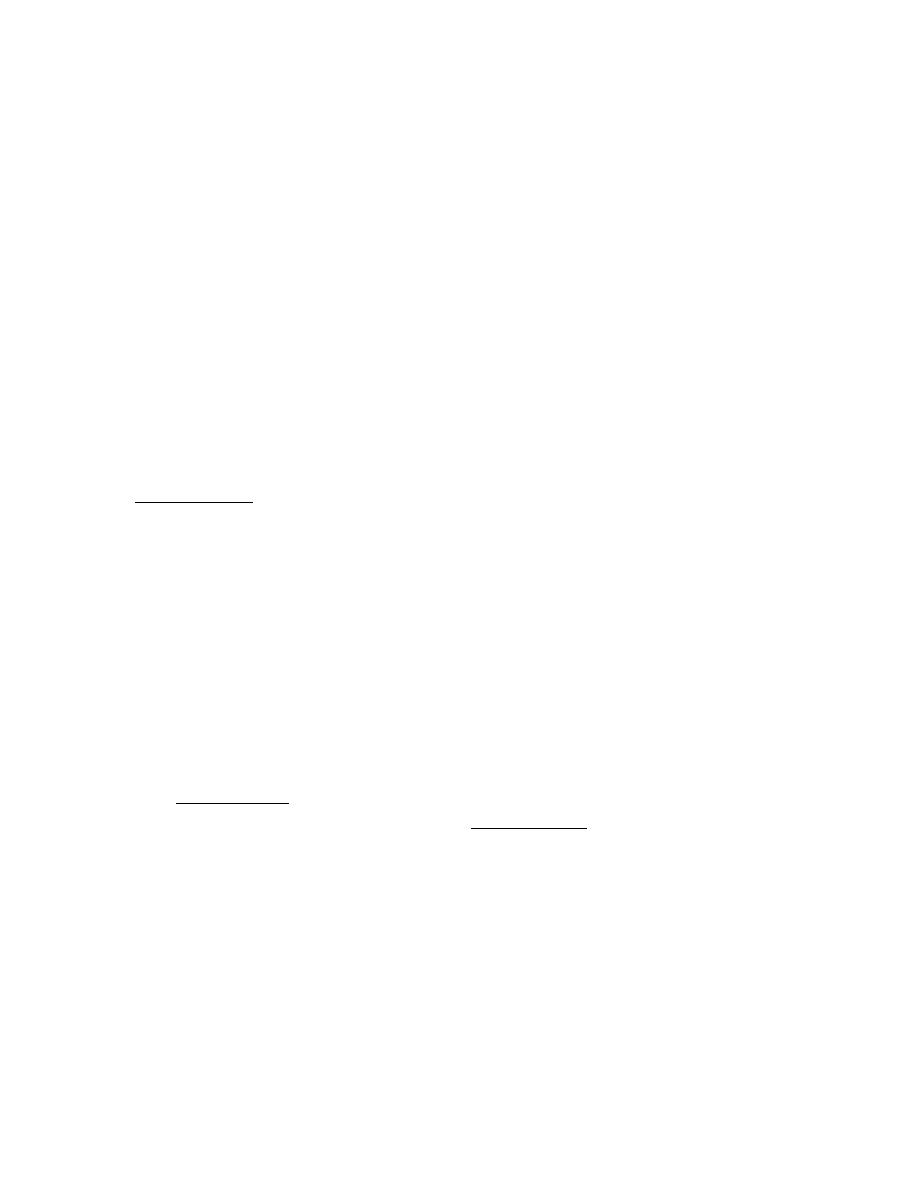
Middle Ear
Air filled cavity in the petrous bone described as six-sided box.
Roof; is formed by a thin plate of bone (tegmen tympani). This plate
separates the tympanic cavity and mastoid antrum from the middle cranial
fossa.
Floor; a thin plate of bone separates the cavity from the bulb of internal
jugular vein.
Anterior wall:
The lower portion is formed by a thin plate of bone separating the cavity
from the internal carotid artery. The upper portion has two openings, the
lower one being the Eustachian tube and above it lies the canal for tensor
tympani muscle.
Posterior wall:
High up in the posterior wall there is an opening (the aditus), which leads to
the mastoid antrum. The pyramid lies below the aditus, it contains the
stapedius tendon. The facial nerve bends downward near the aditus and
become very close to the posterior wall ( mastoid segment of facial nerve).
3
Medial wall:
The promontory is round bony swelling covering the basal turn of the
cochlea. Facial nerve: runs approximately horizontally superior to the
promontory. The oval window is closed by the footplate of stapes. The round
window is closed by secondary tympanic membrane.
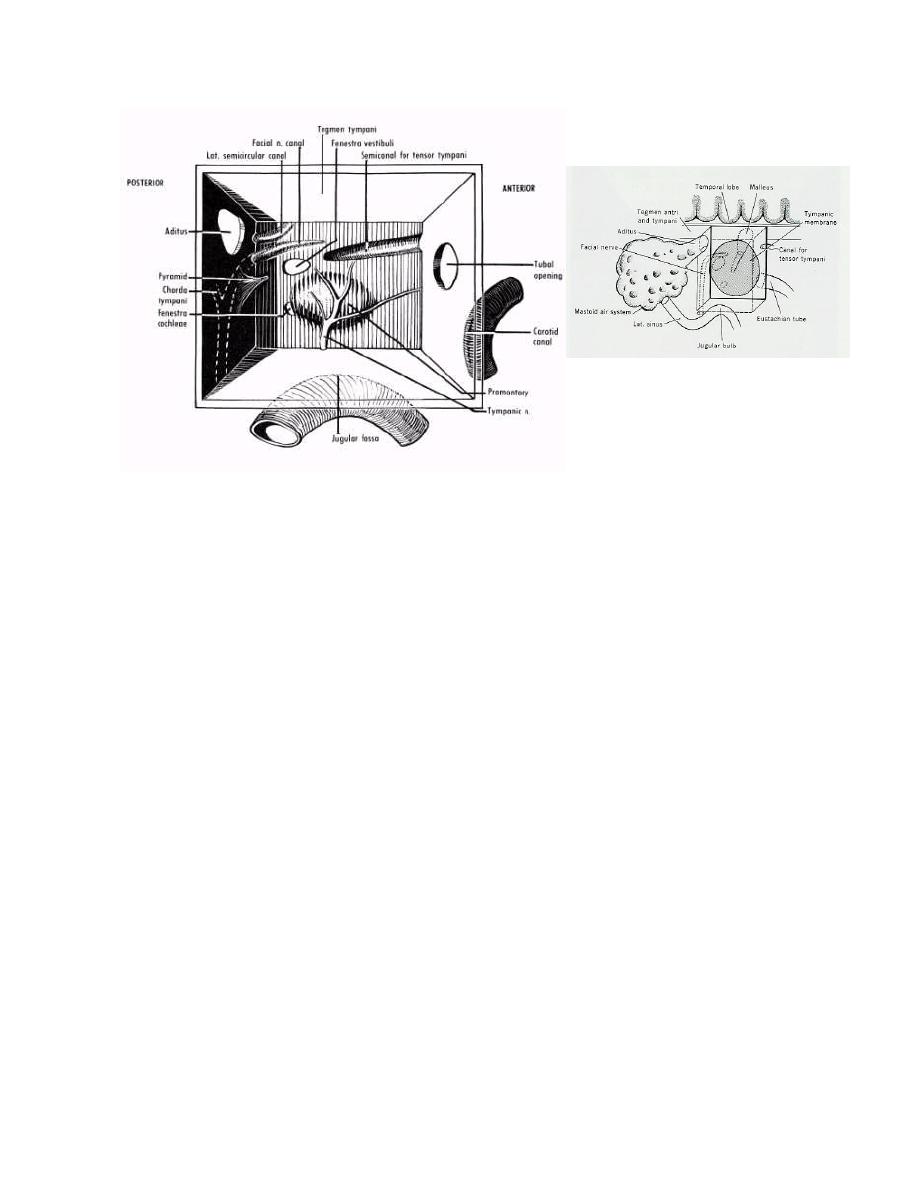
Lateral wall:
Is formed by the tympanic membrane (drumhead or eardrum). It separates
the external meatus from the middle ear and consist of three layers: an
outer epithelial layer, a middle layer of fibrous tissue and an inner layer of
mucous membrane. It has elliptic, funnel shape, about 8-10 mm in diameter.
The ear drum is supported around its periphery by a fibrous thickening, the
annulus, which is deficient at pars flaccida. Normal tympanic membrane is
pearly grey, semitransparent, luster and mobile.
Tympanic membrane is divided into two parts:
1. Pars tensa; represent the lower portion of the tympanic membrane.
2. Pars flaccida (Shrapnell`s membrane); this part of the drum is small
and comprises the uppermost part. The fibrous tissue layer is
deficient in this area, hence the flaccidity. It is frequently referred
to as the attic.
Contents of middle ear:
1. Air at atmospheric pressure, maintained by Eustachian tube.
2. Ossicles; Malleus, incus and stapes.
3. Muscles; Tensor tympani and stapedius.
4
4. Nerves; Facial nerve running in its bony (Fallopian) canal, giving chorda
tympani. Tympanic plexus; lies on the promontory.
Eustachian tube; Connects the tympanic cavity with the nasopharynx. It is
about 36mm in length in adult. At rest pharyngeal orifice of eustachian tube
is closed. It is actively opened during swallowing and yawing.
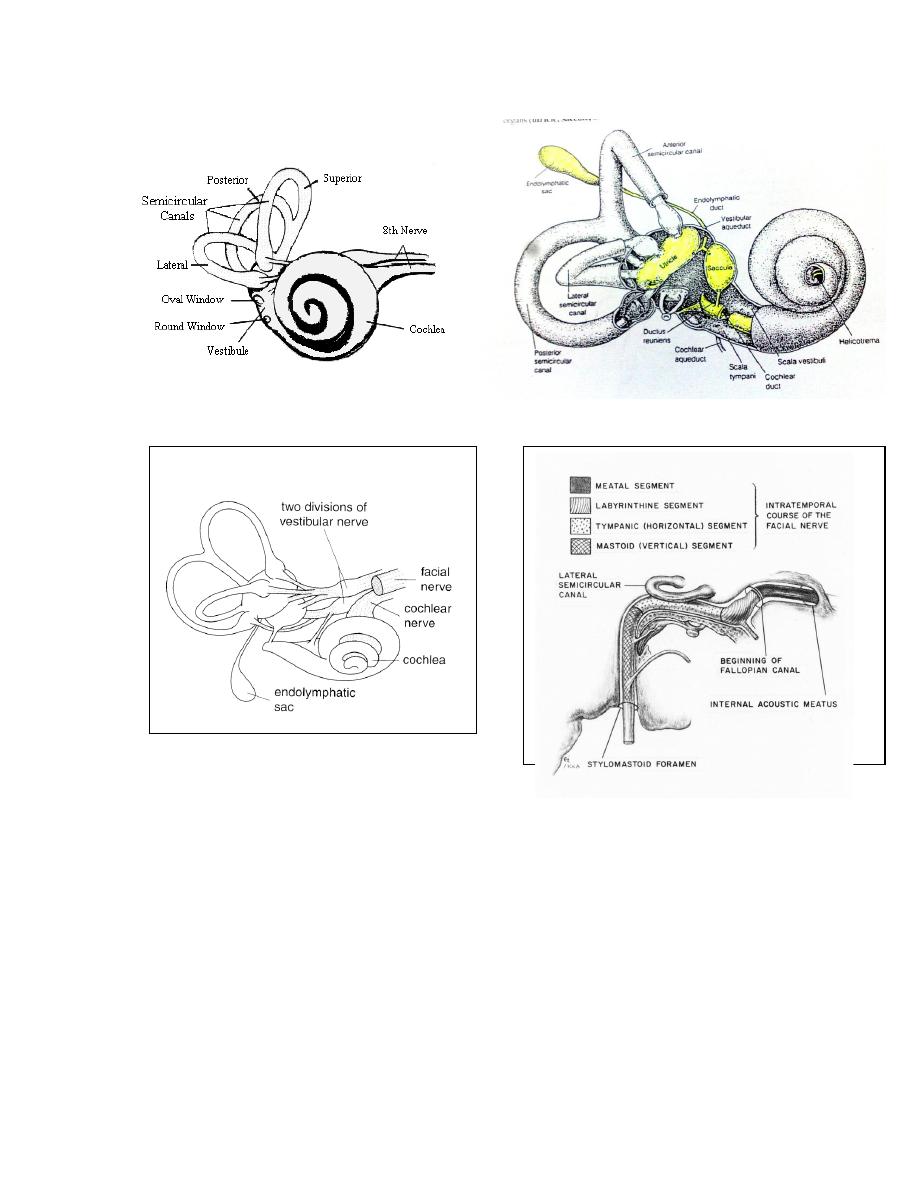
Inner Ear:
The inner ear, or labyrinth, consists of a bony labyrinth and membranous
labyrinth. The membranous labyrinth contains fluid known as endolymph
which is similar to the intracellular fluid. The space within the bony
labyrinth, between its wall and the membranous labyrinth contains another
fluid known as perilymph. The composition of the perilymph is very similar to
the extracellular fluid and CSF.
Bony labyrinth consists of bony cochlea anteriorly, vestibule in the middle
and bony semicircular canals SCC posteriorly( superior, posterior and lateral
SCC). Membranous labyrinth consists of auditory and vestibular components.
The vestibular element which is connected to the vestibular part of 8
th
cranial nerve, consists of utricle and saccule, and three semicircular canals.
The auditory element consists of the cochlear duct and is connected to the
cochlear part of the 8
th
cranial nerve.
5
Blood Supply;
The main supply comes from the labrynthine artery (internal acoustic
artery) which arises from the basilar or anterior inferior cerebellar artery.
Facial Nerve
This nerve emerges from the pons and after crossing the
cerebellpontine angle it enters the temporal bone at the internal auditory
meatus. It passes over the labyrinth until it reaches the medial wall of the
tympanic cavity. Hear it bends backwards at right angle where the
geniculate ganglion is situated and passes almost horizontally, enclosed in the
fallopian canal, above the oval window. When it reaches the aditus it turns
6
downwards behind the pyramid and continues almost vertically till it emerges
from the stylomastoid foramen.
The nerve to stapedius is given off close to the pyramid. Chorda
tympani nerve leaves the descending part of the facial nerve and enters the
tympanic cavity.
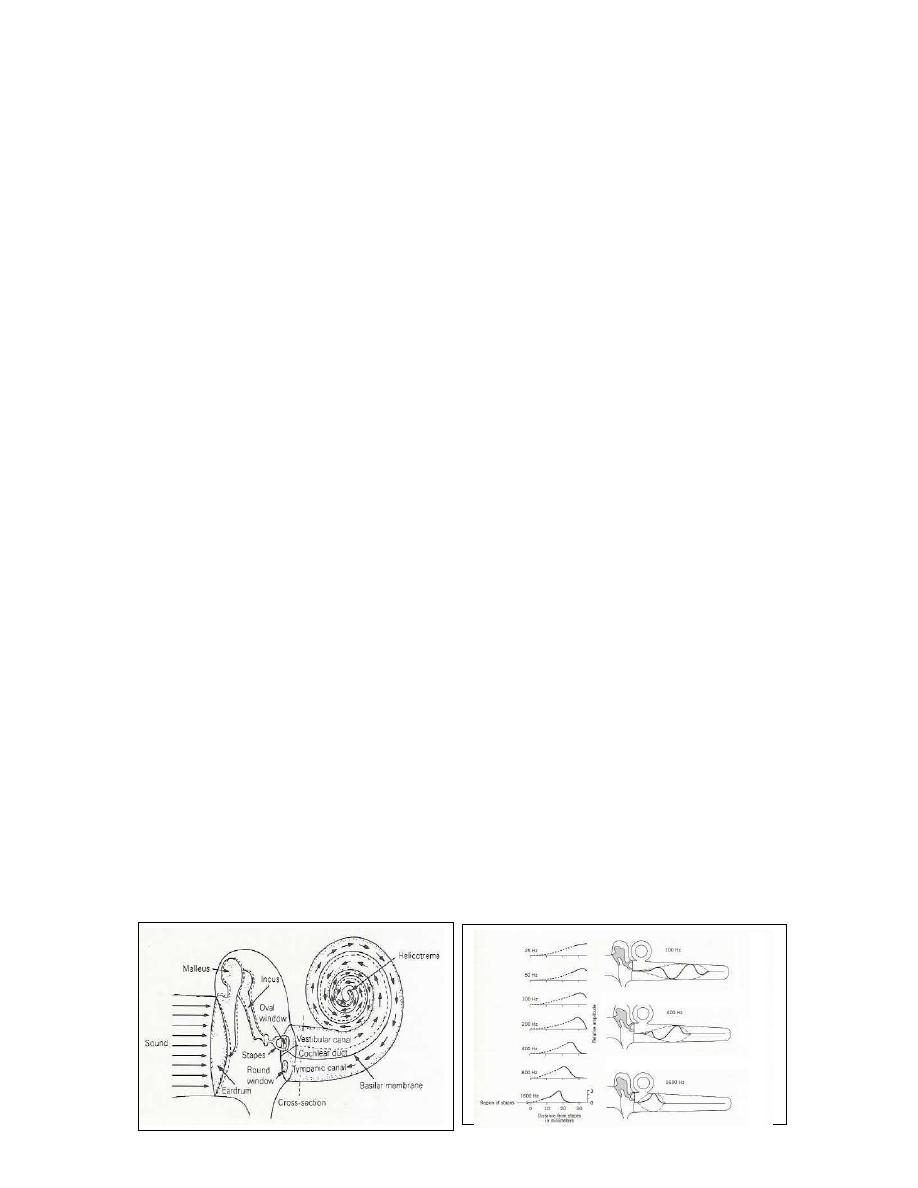
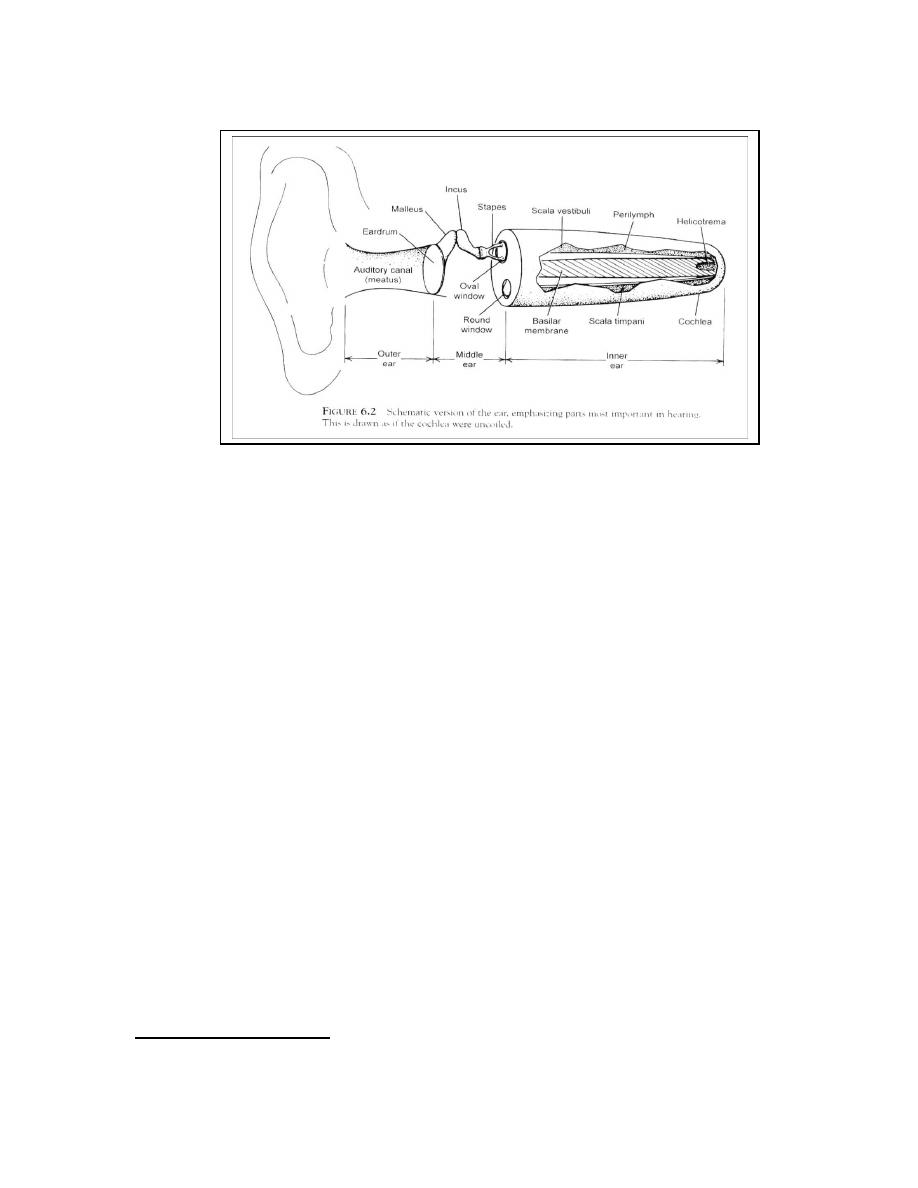
Physiology of hearing
The basic function of the auditory apparatus is to convert the sound
energy from mechanical vibrations in the air to mechanical vibrations in
the inner-ear fluids, and then to nerve impulses in the hair cells, to be
transmitted along the auditory nerve to the higher centers of hearing.
The auricle collects the sound waves, which pass through ear canal to the
tympanic membrane which in turn sets into motion. Vibrations are
transmitted to the ossicles. The stapes footplate is attached to oval window
and causes inner ear fluids to vibrate. Nerve signal is generated in the hair
cells and transmitted through auditory nerve.
Transformer Ratio: two factors are important to magnify the vibrations
and overcome the resistance of the inner ear fluids. The ratio between
surface area of tympanic membrane to that of oval window is 14:1. The lever
ratio of ossicular chain is 1.3:1.
14* 1.3= 18:1.
Physiology of the vestibular apparatus
Balance of body is maintained by coordination of information from three
systems: Proprioception, (i.e. sensation from muscles, joints and ligaments, )
vision and the vestibular system. Vestibular system consists of semicircular
canals, utricle and saccule. Utricle and saccule respond to linear acceleration.
Semicircular canals respond to angular (rotatory) acceleration, and
stimulation of the semicircular canals gives rise to the sensation of rotation.
7
Symptoms of ear disease
1. Hearing loss ( Deafness) :
It may be conductive, sensorineural or mixed. Conductive hearing loss (CHL)
may be due to diseases of the external auditory meatus, tympanic
membrane, the middle ear cavity or ossicles. Sensorineural hearing loss
(SNHL) can be a result of diseases of the cochlea or its neural connection.
In CHL the sound appears quieter but it is not distorted. Sound and speech
are well heard when amplified. In some cases the patient may hear better in
the presence of background noise e.g. railway carriage or bus. This is called
paracusis Willisii and it is found most typically in otosclerosis. The quality of
speech is well maintained because the patient hears his own voice clearly (by
bone conduction).
In SNHL the sound not only seems quieter but it is distorted as in majority
of cases the higher frequencies are more affected than the lower, leading
to difficulty in hearing the consonant sounds which are so important for
speech discrimination. In severe SNHL the patient does not hear his own
voice and leads to speech which is indistinct or expressionless. Tinnitus is
commonly associated.
Causes of hearing loss
Conductive
8
1.
External canal obstruction: impacted wax, foreign body, tumor, canal
atresia.
2.
Perforated eardrum: CSOM, traumatic..
3.
Ossicular chain fixation: otosclerosis, congenital fixation…
4.
Ossicular chain discontinuity: car accident, head injury…
5.
Fluid in middle ear: secretory otitis media (common cause of CHL in
children).
Sensorineural
1. Congenital hearing loss: bilateral and symmetrical ( may be Deaf Mute)
2. Ototoxic Drugs: e.g. aminoglycoside, frusemide, aspirin, quinine, cytotoxic
drugs.
3. Aging: hearing loss is symmetrical, and usually progressive (Presbycusis)
4. Infection: Mumps deafness is unilateral, measles: bilateral.
5. Trauma: fracture of base of skull
6. Tumor: cerebellopontine angle tumor : vestibular schwannoma.
7. Endolymphatic hydrops: Meniere's disease ( vertigo + deafness + tinnitus )
8. Noise-induced hearing loss and acoustic trauma.
2. Discharge( Otorrhea) :
Serous or purulent discharge; Otitis externa.
Mucopurulent discharge, foul smell long duration: chronic suppurative
otitis media.
Unilateral watery discharge following head injury or aural surgery:
CSF otorrhea. It occurs as a result of damage to tegmen tympani.
Bloody discharge; due to granulation tissue in chronic suppurative
otitis media or due to malignant disease.
3. Pain (Otalgia) :
It arises within the ear (primary) or outside the ear (referred otalgia) .
Referred otalgia is commonly referred to the ear from lesions of related
structures whose nerve supply also send branches to the ear. The ear
receives sensory nerve supply from..(see above). Referred otagia is
remembered by the mnemonic 10 Ts: trachea, thyroid (cartilage and gland),
tonsil (and tonsillectomy), tongue, TMJ( temporomandibular joint),
teeth(specially wisdom), trapezius (=neck spasm), tumor( mainly
hypopharynx),Tb and tics.
4. Tinnitus:
9
It is a subjective sensation of sound in the ear or head in the absence of any
relevant external signals. (Occasionally it is objective e.g. in palatal
myoclonus and glomus tumors). It is regarded as a sign of irritation of the
cochlea or auditory pathways. Tinnitus may be met with any form of ear
disease and is commonly associated with SNHL, and is also a symptom of
some general diseases which indirectly affect the ear through the
circulation. It is a common symptom of anaemia, thyrotoxicosis,
hyperdynamic circulation, renal failure and some intracranial tumors. It may
be caused by ototoxic drugs, such as quinine, salicylates and aminoglycocide.
5. Vertigo:
It is defined as illusion of movement or subjective sense of imbalance.
Vertigo is considered as a symptom of irritation of the vestibular apparatus
and it must be differentiated from conditions such as fainting, dizziness,
drop attack and postural hypotension. Vertigo may be central in origin
(cerebellum), or peripheral (labyrinth /vestibular nerve). Peripheral lesions
tend to produce intense vertigo of sudden onset. Nausea and vomiting are
common (which indicate severe vertigo). Central lesions-on the other hand-
produce less intense vertigo. Positional changes have less effect, but the
patient tends to have more disturbance of gait.
Physical Examination
It is performed with the aid of head mirror or head light, and ear speculum.
Otoscope( auriscope) is used for examination of ear canal and tympanic
membrane. Microscope is sometimes required for examination.
Hearing Tests
I. Voice tests: A person with normal hearing can hear conversation voice
with the opposite ear occluded in a quiet room from a distance of 6 meters.
II. Tuning fork tests:
Rinne's test:
It compares AC air conduction to BC bone conduction of each ear separately.
Normal = AC
BC ( Rinne +ve)
CHL =BC > AC (Rinne –ve)
SNHL = AC
BC (Rinne +ve) and often BC is not heard
Weber test:
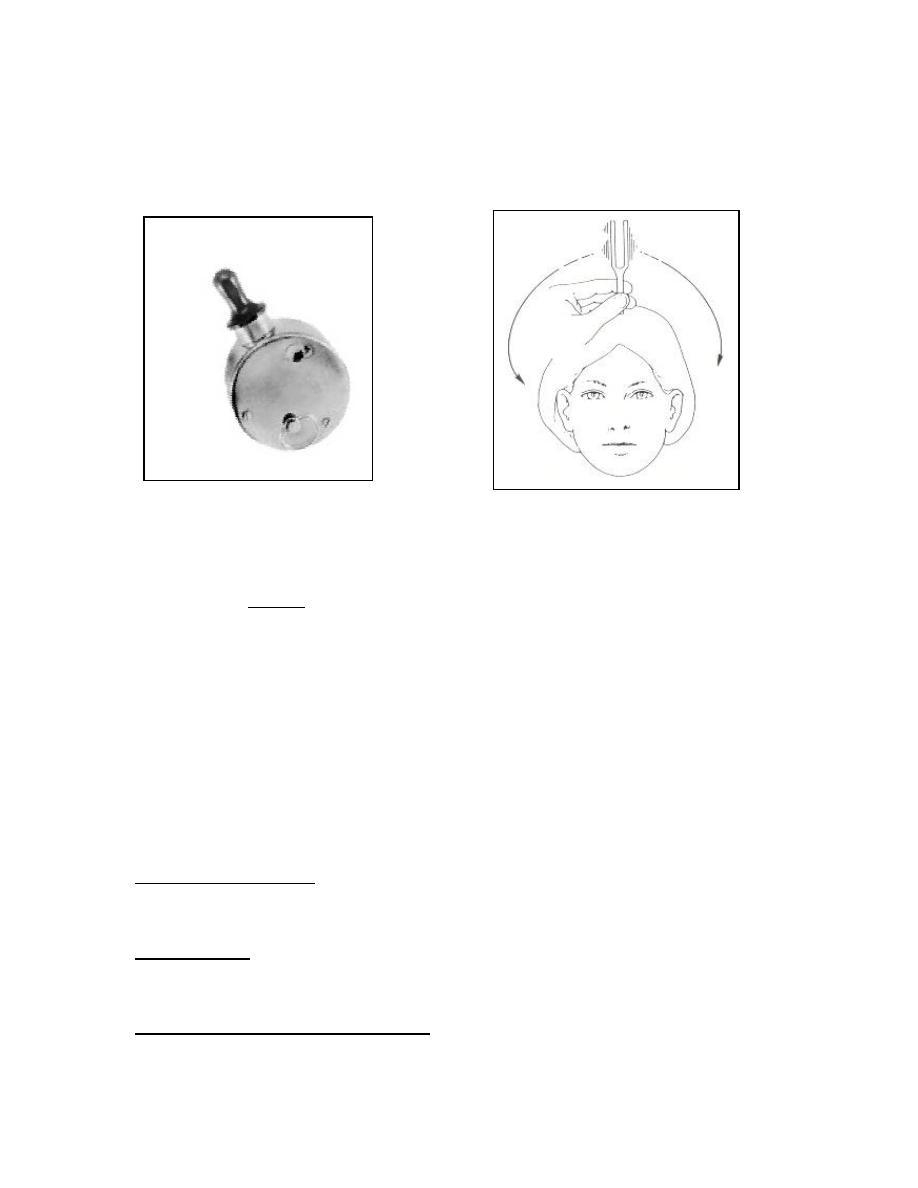
This test compares BC of the two ears.
Normally weber test is central (heard in the midline or in both ears)
10
In CHL sound is lateralized to the affected ear (due to masking of
environmental noise).
In SNHL the sound is heard in the non-affected ear (better cochlea).
Barany's noise box Weber test
False negative Rinne;
In unilateral severe SNHL (or dead ear), Rinne's test will appear to give a
negative result. AC is absent but BC may be good because the sound is
transmitted to the opposite cochlea through skull. This result may confuse
the examiner in making a wrong diagnosis of CHL. In this situation Weber
test is important and it is lateralized to the unaffected ear. This condition
can be overcome by applying a Barany's noise box to the non-test ear which
emits noise to the non -test ear to such a level that the TF cannot be heard
in that ear by cross hearing. It will then be found that the patient is unable
to hear the TF by either AC or BC.
III. Audiometric tests:
Pure Tone Audiogram: Normally AC and BC are both better than 30 dB and
there is no gap between them. In CHL AC is reduced while BC is normal, with
air bone gap ABG. In SNHL both AC and BC are reduced.
Tympanogram: Type A is normal. Type B is flat curve due to fluid behind
tympanic membrane ( secretory otitis media). Type C: small peak is found in
the negative pressure indicating Eustachian tube dysfunction.
Auditory brainstem response ABR: It is an objective assessment of hearing
to elicit brain stem signal in response to a sound (such as a click). In ABR
11
audiometry - also known as brainstem evoked response (BSER) – electrical
waves are generated by the cochlea, auditory nerve, brain stem and higher
centers in response to auditory stimulus and picked up from the vertex by
surface electrode.
Indications of ABR
1. To determine hearing threshold for infants, children and malingerers.
2. To differentiate between cochlear and retrocochlear pathology.
3. To aid in the diagnosis of brain stem pathology as multiple sclerosis.
Examination of vestibular function
It starts by testing hearing as some vestibular disorders are associated
with deafness. Then general examination to exclude non-vestibular causes of
dizziness. Nystagmus means involuntary, rhythmical, oscillatory eye
movement. It is usually horizontal or rotatory nystagmus in vestibular
diseases. Clinical tests of balance include Romberg's test, Unterberger's
test, Halmagyi head thrust and Dix-Hallpike positional test.
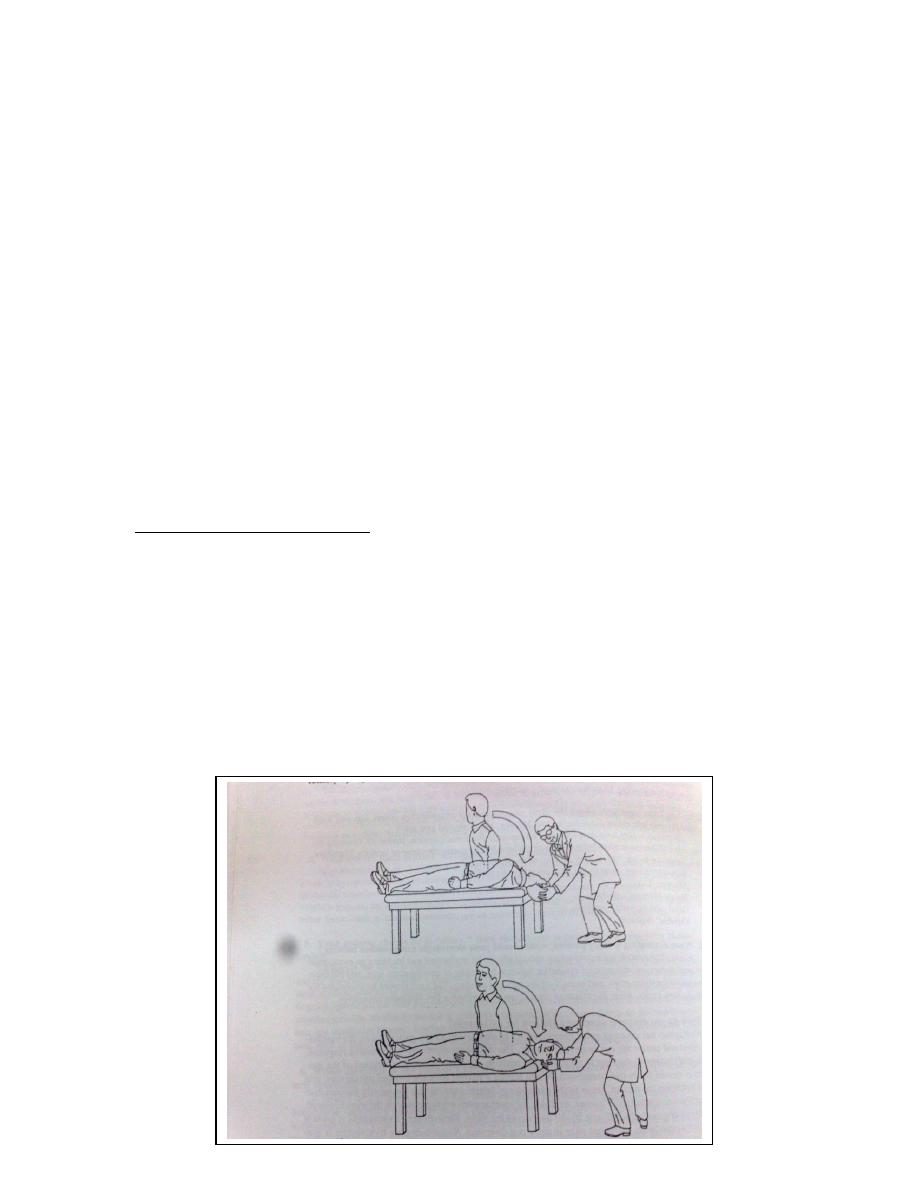
Dix-Hallpike positional test:
It is done when vertigo is related to specific movements. The patient sit
erect upon a couch in such a position that, when lying down, the head will
slightly overhang the end of the couch. The head is turned to one side and
the patient is asked to fix his gaze on a distant point. The examiner hold the
patient's head and the patient is then laid down quickly, the head assuming a
position just below the horizontal. The test is repeated with the head
turned in the opposite direction. Characteristic finding include torsional
nystagmus indicating benign paroxysmal positional vertigo of posterior
semicircular canal.

12
Vestibular function tests:
1. Rotatory chair tests: The disadvantage it stimulates both canals
simultaneously.
2. Caloric test: In this test each labyrinth can be tested separately.
Syringing the ear with hot or cold water induces convection currents within
the lateral SCC and therefore stimulates them with resulting vertigo and
nystagmus.
The patient lies with the head at an angle of 30 degree above the
horizontal, which brings the lateral SCC into a vertical plane. The ears are
irrigated in turn with water at 30 C then at 44 C (7 C above and below body
temperature. Nystagmus commonly last for about 2 minutes from the
beginning of stimulation. Canal paresis is present if the duration of
nystagmus is reduced for both hot and cold tests. Canal paresis is suggestive
of a lesion in the peripheral vestibular apparatus.
3. Electronystagmography (ENG) and videonystagmography (VNG):
4. Dynamic posturography.
