A FOCUS ON
PULPITISWHY???Is the PULP angry???
This subject???DEFFINITION: (dental pulpitis,is an orofacial, acquired, inflammatory pain condition.)
Dental pain is the most common symptom of diseased tooth pulp, often as a result of coronal caries of the tooth.
The mature human dental pulp is densely innervated with fibres that originate from the trigeminal ganglion. The normal pulp seems insensitive to exteroceptive
stimuli; however, in pathological states such as pulpitis (inflammation of the pulp), electrical, thermal, mechanical and chemical stimuli all produce a nociceptive response. Primary and permanent tooth pulps contain 70-90% C-fibres, and thin myelinated A delta fibres .
The majority of nerve fibres terminate in the coronal region of the pulp, forming a subodontoblast plexus, with 40% terminating in the dentinal tubules close to the odontoblast processes.
The International Association
for the Study of Pain (IASP).
The voltage-gated sodium-channel type IX alpha subunit, known as Nav1.7 and encoded by the gene SCN9A , is located in peripheral neurons and plays an important role in the action potential of these cells. Nav1.7 is concentrated preferentially in rodent small diameter neurons. The presence of Nav1.7 sodium channel has been demonstrated in sensory neurons in human dorsal root ganglia (DRG).
Immunoreactive nerve fibres in non-painful (left column)
and painful (right column) human tooth pulp sections, within the subodontoblastic plexus region. Staining with antibodies to Nav1.7 (Figures 1a and 1c) and neurofilament cocktail (Figures 1b
and 1d). Magnification × 40.
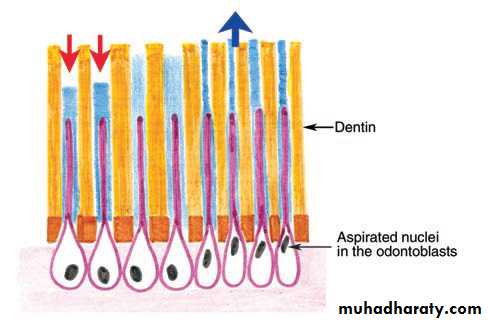
: Illustration of the movement of dentinal fluid inside dentinal Tubules in response to a hot stimulus (red arrow) and a cold stimulus (blue arrow).
With over 900 axons(huge nomber) known to enter the average human premolar tooth
less than half of these fibres that innervate the dental pulp (40%) terminate in dentinal tubules, close to the odontoblast process.the remaining fibres form the subodontoblastic plexus in the coronal aspect of the pulp tissue.
nerve fibers myelin staining within different regions of the human dental pulp. A and B. Confocal micrographs showing N52 (red) and myelin basic protein (MBP; green) staining relationships in the coronal region (A; longitudinal plane) and in nerve fiber bundles located in the center of the radicular area (B; cross-section). Both images show the presence of N52-identified nerve fibers that lack myelin (arrowhead) and fibers with myelin (arrow).
The nerve fibers without myelin are common in both pulpal regions but more so within the coronal region. The outline shown in A indicates the approximate position of the odontoblastic layer. Scale bar, 20 μm.
MTA & PULP CAPPING
Clinical procedures used to treat the pulp .Pulp exposures (A) were
cleaned with 2.5% NaOCl (B); after hemostasis was achieved(HOW??), MTA was applied (C), which was then covered with a light-curing glass ionomer (D). In the same appointment, a restoration was placed (E).
radiographic appearance of teeth included in MTA study.
A: Case 1 (tooth #19) showed no apical pathosis before pulp capping and at recall. B: Case 2 (tooth #30) testedpositive to cold initially and was treated with an MTA pulp cap. However, the tooth became
painful before the scheduled recall appointment and a root canal treatment was performed.
Calcium hydroxide MTA???
Calcium hydroxide remains the “gold standard” for direct pulp capping. It has the longest track record of clinical success,it is the most cost-effective and is the likely effective component in MTA.
It provides a well-sealed restoration immediately after pulp capping.
This will provide protection against ongoing leakage and bacterial contamination that can compromise the success of the
pulp cap.
CLINICAL photographs and periapical radiographs of tooth #29
Figure(A):the radiograph showing a large distal proximal caries close to the coronal pulp of tooth #29.Figure(B): Exhibits the intact occlusal surface of tooth #29. Figure(C): Reveals fresh residual pulp tissue after removal of caries and 2-3 mm of the exposed superficial pulp tissue layers and control of pulpal bleeding. Figures(D) through(F): Radiographs taken
one month (Figure D), three months (Figure E) and 10 months (Figure F) after initial
treatment showing a coronal filling of resin composite and MTA in tooth #29 and no apical
pathosis at the periapical area of tooth #29.
MTA REACTION
A: Low-power (original magnification 10×) microphotographshowing a thin reparative dentin bridge below MTA and no inflammation in the underlying residual pulp tissue. A short segment of superficial odontoblastic layer just below the dentin bridge was destroyed.
However, the deeper odontoblastic layer was intact.
B: High-power (original magnification 50×) microphotograph revealing no inflammation and a small focus of dystrophic calcification (arrow) in the underlying residual pulp tissue.
Deeper section
C: Low-power (original magnification 10×) microphotographof a deeper tissue section showing a thicker reparative dentin bridge
below MTA and the nearly normal underlying residual pulp tissue.
D: High-power (original magnification 50×) microphotograph
exhibiting the reparative dentin bridge that is made up of osteodentin
and no inflammation in the underlying residual pulp tissue.
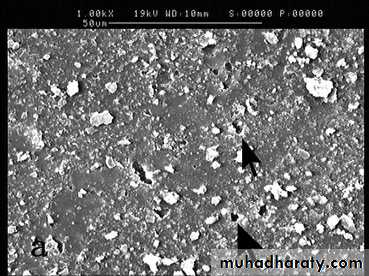
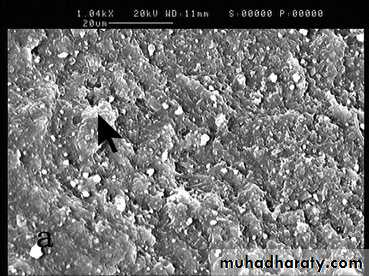
Sensitive dentin
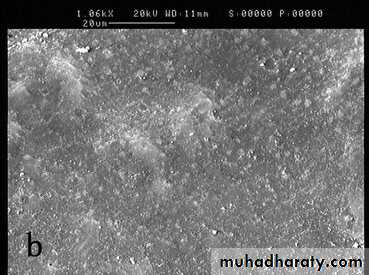
SEM Figure shows: There are several open dentin tubules on the sensitive dentin (marked with arrows) before the treatment
After treatment????With WHAT????
Most dentin tubules are occluded immediately after the application of treatment.Some dentinal tubules are re-opened one month after treatment
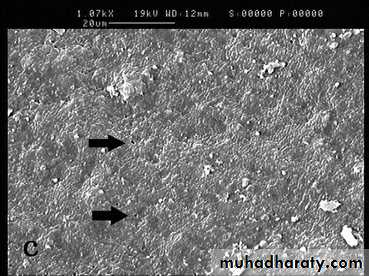
SENSITIVE DENTIN
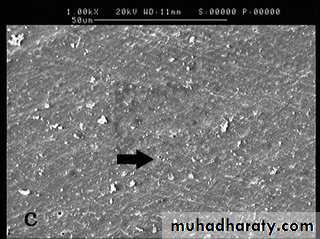
SEM Figure : another area of dentine. There are several open dentin tubules on the sensitive dentin (marked with arrows) before the treatment.Immediately & after one month
Microleakage comparing
Dye score zeroDye score three
Microleakage study
Score twoScore one
Effect of bleaching on pulp
a study showed that after two bleaching sessions, the use of light activation did not improve bleaching speed.Persistent tooth sensitivity and higher tooth sensitivity levels after 24 hours of bleaching were observed when LED/laser light activation was used.
Vital pulp therapies are biologically-based treatments in which the main objective is to save pulp health and vitality in carious or traumatic exposures.
These treatments include: indirect pulp capping, direct pulp capping (DPC),
and pulpotomies
(a) Preoperative periapical radiograph of a second mandibular left molar in a 14-year-old female patient. The tooth was sensitive to cold and percussion. Note the mesio-occlusal extensive caries and related coronal cavity, apical periodontal ligament (PDL) widening, and narrowradiolucent lesion. (b) Immediately after direct pulp capping withCEM(a water-based, tooth-colored cement containing lime(CaO), phosphorus oxide (P2O5), sulfur oxide (SO3), and silica (SiO2) as major elements) cement, placement of a glass ionomer base, and permanent coronal restoration. (c) Ten-month follow-up. (d) Fifteen-month follow-up. The tooth was functional without sensitivity to percussion. The PDL space regained its normal width, and the radiolucent lesion healed
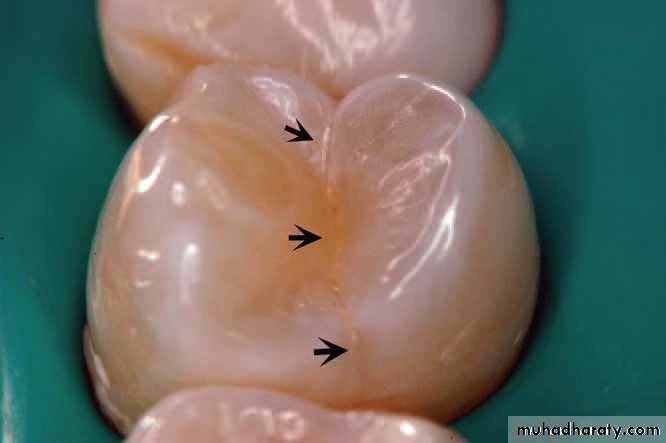
CRACKED TOOTH
The term cracked-tooth syndrome was first used by Dr Cameron in 1964 and was defined based on three clinical observations. First, a patient complained of pain upon application of cold or pressure
to a tooth that had been recently restored with a mesio-occlusal inlay, and there was relief of the pain a year later when the distal cusp broke off,
even though sensitive dentin was then exposed.
the second observation, some posterior teeth had abscessed with small shallow restorations and no periodontal disease; however, there was evidence of rarefactions at the apex. Upon extraction and examination with magnification, many of these teeth were found to have cracks extending from the mesial, distal, or both marginal ridges, and the patients had a previous history of pain.
The third observation came from three other cases where, after extraction of fractured teeth, patients shortly thereafter complained of
pain in another tooth. These latter suspect teeth were covered with crowns and complete fractures were prevented. Other authors had previously
described the incomplete fracture as ‘‘cuspal fracture odontalgia,’’ ‘‘fissured fractures,’’ and ‘‘greenstick fracture of the tooth crown.’’
(CTS) is described as an incomplete
fracture of a vital posterior tooth involving enamel
and dentin and possibly the dental pulp. It may
cause a complete fracture, reaching the dental pulp
and/or periodontal ligament.
CRACKED TOOTH
Initial view of the nonrestored tooth 24.Periapical radiograph of left maxillary premolars. No significant findings were present .
DIAGNOSIS
Bite test using a wooden wedge revealed pain in tooth 24.A crack was observed under transillumination . On the occlusal surface of tooth 24, from a mesial to distal orientation.
Treatment procedures
A stainless steel orthodontic band was cemented to confirm the diagnosis. The patient could bite without pain after this procedure.A cone beam computed tomography showing the crack in
a mesial-distal direction, involving the mesial, occlusal, and distal faces.Cracked tooth
Using a rubber dam, the crack was better visualized bygiving a contrasting color to background and keeping the tooth
dehydrated.
a): Transillumination was useful to confirm the defect removal during the cavity preparation, until no more cracks were visualized.
b): Completed MOD cavity preparation
Treatment completed
The tooth received a provisional restoration, and thepatient tested the tooth for 21 days.
After the symptoms were eliminated, a direct bonded
MOD composite restoration was performed
Pulp revascularization:which has emerged as a promising alternative with more advantages than the traditional treatment of apexification.
Initial condition of patient with fracture of both central incisors.
(a): Facial view. (b): Lateral view.
Clinical (a) and radiographic (b) evaluation of the fractured teeth.
Treatment procedure
Shade testing using uncured composite.Isolated operatory field and smoothed enamel margins with a ½ mm bevel.
Pulp revascularization
Conditioning the teeth with 35% phosphoric acid extending beyond the anticipated margin to prevent unattached composite resin.(a): Construction of palatal surface using the freehand technique.
(b): Palatal surfaces of right and left central incisors.
Based on the diagnosis, pulp revascularization using a tripple antibiotic paste (250 mg ciprofloxacin, 400 mg metronidazole, and 50 mg minocycline) was performed.
Access opening of root canal,
And the canal was carefully decontaminated with irrigant solutions : A-6% NaOCl, B-physiological solution, and C-2% chlorhexidine gel.
then
The triple antibiotic paste was inserted and left for 21 days. At the second visit, the medication was removed and a manual K-file
was introduced 2 mm beyond the working length to induce bleeding into the canal. A barrier of a restoration was placed on the blood clot, and the access opening was double sealed.
In the reported case, the patient was completely satisfied with the final results. The treatment achieved its objective of restoring function andesthetics of the fractured anterior teeth.
Final result of restorations.
(a): Front view. (b): Lateral view.
Radiographs after pulp revascularization (a) and after 18 months (b).
medium, deep and shallow
Pulp reactions after the application of dental adhesives and composites ,in medium, deep and shallow cavities do not occur if an intact dentin layer of 0.5 mm is present.This shows that dentin may be protective against material toxicity. The reason is that the permeability of dentin is related to dentin thickness , in which the diameter of dentinal tubules increases with decreasing distance to the pulp.
Furthermore, after cavity preparation, dentin is covered with a
smear layer, which further reduces its permeability.
CAVITIES???
Induction of Tertiary Dentin Formation:
The concept of inducing biomineralization is not new, since pulp capping with Ca(OH)2 was introduced by Herrmann as nearly as 1928. Apparently, signaling molecules that induce tertiary dentin formation, such as transforming growth factor–b1, are present in dentin and can be released through the application of Ca(OH)2 or exposed on the dentin surface by ethylenediamine tetraacetic acid (EDTA). Signaling molecules activate responsive cells (pulpal stem cells), which are present in specific niches in the pulp tissue. These cells migrate to the site of pulp exposure, where they differentiate into secondary odontoblasts and form tertiary dentin.THE TISSUE REGENERATION CONCEPT
Tissue regeneration can be achieved using methods of tissue engineering, as described byLanger and Vacanti, with the following components:
1) a matrix/scaffold, 2) signaling molecules and 3) responsive cells (stem cells or progenitor cells).
Langer R, & Vacanti JP (1993) Tissue engineering Science 260(5110) 920-926.
The term ‘stem cells‘ for undifferentiated cells in certain areas of the tissues (niches) is not correct for such cells in the dental pulp. The term progenitor cells is more appropriate, since such cells in the dental pulp, which have the potential to develop into secondary odontoblasts, already
show a certain degree of specialization. However, the term ‘‘pulpal stem cells’’ is often used in the literature
DENTAL PULP STEM CELLSDPSC
Signaling molecules, are present in dentin and can be released (eg, by treatment with EDTA). dentin surfaces can be activated and signaling molecules are exposed on the dentin surface, potentially inducing the differentiation of pulp stem (progenitor) cells contacting dentin to become secondary odontoblasts (contact differentiation).
Stem cells are present not
only in the pulp tissue but also in periapical niches and in inflamed apical tissues as well as in the
evoked intracanal blood influx from periapical tissues.
DPSCCELL HOMING
According to the tissue engineering concept, a matrix/scaffold is needed, into which signaling molecules and stem cells are incorporated.two concepts have been discussed in the literature: one is the isolation of stem cells with in vitro expansion for reimplantation; the other is a primarily cell-free concept, which relies on the immigration of resident stem cells into a matrix scaffold as a result of the presence of signaling
molecules (cell homing).
Both concepts rely on a
suitable matrix/scaffold that can be regarded as a:
dental material, which must have properties different from commonly used dental materials.
The possibility of pulp regeneration has been shown in several studies. One of the first was presented by the group of J. No¨r, who placed dentin slices filled with a solid poly-L-lactic acidmatrix containing human pulp-derived stem cells and vascular endothelial growth factor subcutaneously into mice.Cordeiro MM, Dong Z, Kaneko T, Zhang Z, Miyazawa M, Shi S, Smith AJ, & No¨r JE (2008) Dental pulp tissue engineering with stem cells from exfoliated deciduous teeth Journal of Endodontics 34(8) 962-969.
revascularized/revitalized tooth
DPSC
Clinical success was only determined by radiographs and vitality testing. One case allowed for later histologic evaluation: a pulp revascularization protocol had been applied to an immature permanent incisor with irreversible pulpitis and without apical lesion.The tooth fractured 3.5 weeks later and had to be extracted. Histology showed a loose connective tissue similar to pulp and a layer of flattened odontoblast-like cells lined along the predentin. One can speculate whether this new tissue was due to regeneration or was a remnant of the original pulp.
A) Dentin cylinders show formation of connective tissue after pretreatment with EDTA, while no resorptions are observed.(B) A pulp-like tissue has formed and blood vessels are visible. Cells are in close contact to dentinal wall and showed a flat morphology .
The modern patient who seeks information from many easily available sources will ask his dentist for advice.
Therefore, the successful dentist of the future will not only be the expert who knows all relevant diseases and how to prevent or treat them .
But will also be someone who possesses the argumentative competence to effectively communicate with a well-informed
patient and to participate in public discussions.
AS A CONCLUSION
The dental clinician should not rely solely on the type of pain to determine a diagnosis. Other nonodontogenic types of pain, as well as psychological pain, may obfuscate the correct diagnosis. Type of pain has not been correlated with the histopathologic condition of the pulp.The stimulus itself may indicate the type of pain, but does not indicate the changes occurring in the pulp tissue or the stage of inflammation occurring.
incidences of post-obturation pain and flare-ups following the single visit procedures, especially in communities where
patients default after the first appointment at which pain is relieved
. However, single visit endodontic therapy has been shown to
be a safe and effective alternative to multiple visit treatment
comparison of incidence between single and multiple endo visit procedures
Emergency pulpotomy in relieving acute dental pain
remove of the coronal portion of the pulp using a round carbide bur. Haemostasis was achieved by pressing a sterile cotton pellet against the site of amputation for 2–3 minutes. The pulp chamber was irrigated with 2.5% sodium hypochlorite and was dried with a sterile dry cotton pellet.A sterile cotton pellet moistened with eugenol solution was then placed against the remaining pulp tissue. The access cavity was sealed with reinforced zinc oxide eugenol cement and
the occlusion checked. All the clinical work was done by JWN.
Very effective especially on premolars.
Thank you
For your attention