1

INTRODUCTION:
Growth monitoring involves
following changes in a child's
physical development, by regular
measurement of weight, and
sometimes of length. It is an
important tool in individual care,
for early detection of health and
nutrition problems in growing
children

INTRODUCTION:
In general, growth monitoring may provide
for earlier detection of the need for
intervention than one-time screening
measurements. Moreover, the trend
measurement can distinguish children of
adequate achieved size who are running
into problems.
4
HOW OFTEN SHOULD
CHILDREN BE
MONITORED?
Should be done once every month, up to age of 3
years and at least once in 3 months, thereafter.
Deceleration in linear growth at an early age has
been shown to be associated with increased risk of
subsequent mortality . Growth monitoring also has
the advantage of recording responses to
intervention.
5

WHY DO WE CONDUCT THE
GROWTH MONITORING
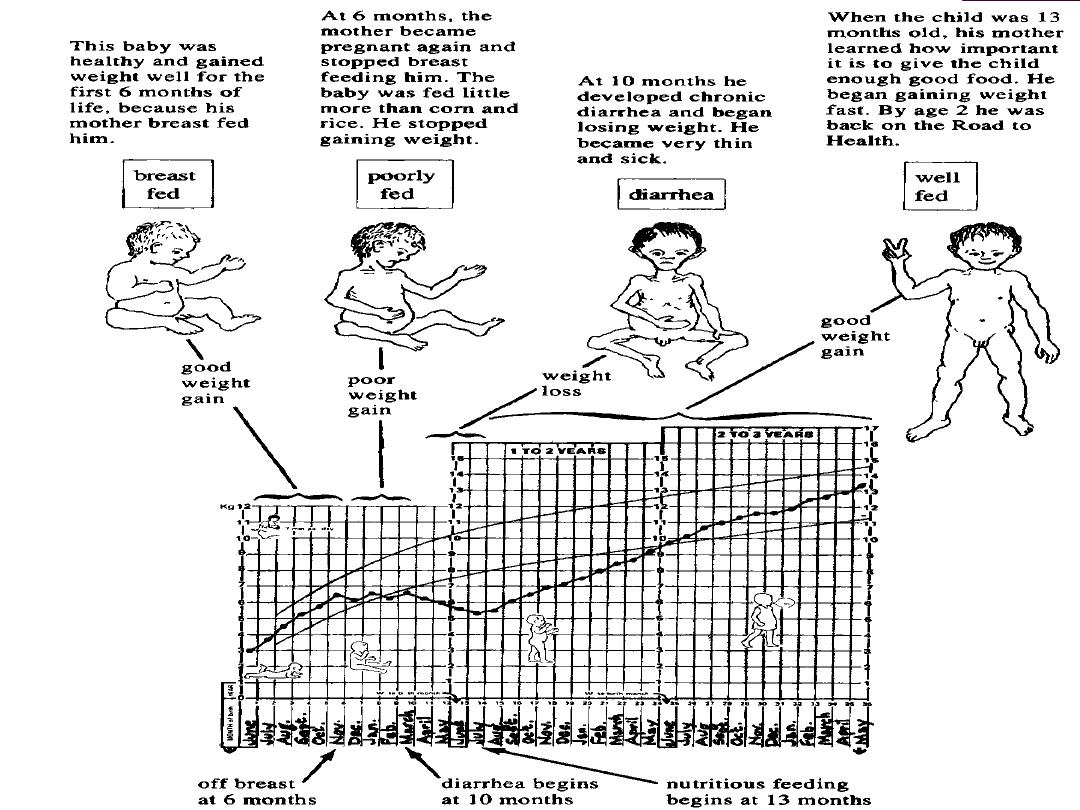
Any child must put on weight as he/she grows
older. Over time, we can tell whether that child is
developing normally or otherwise. The use of
growth monitoring extends beyond problem
detection. It has been used to provide a basis for
communicating with mothers and with health
workers, concerning child health and nutrition, and
to stimulate thinking about the causes of poor
growth and malnutrition.
This in turn has led to
action at the level of the household and of
the community itself .
6

WHO TO MEASURE?
Growth charts in particular have been used
for healthy children, under the normal
circumstances of growing up, in both
developed and developing countries. It is this
early and continued use which gives them a
particular advantage for prevention. Thus,
ideally all children should be regularly
weighed and the results kept on growth
charts. In practice, certainly all children
enrolling in health and nutrition programmes
should be issued growth charts, and mothers
motivated to ensure regular
7

1- Genetic inheritance.
2-Nutrition.
3-Age.
4-Sex.
5-Physical surroundings.
6-Infection and infestations.
7-Economic factors.
A normal child may be defined as one whose
characteristics fall within the range of
measurements accepted as normal for the
majority of children in the same (or
reference)age group.
These limits of normal variation are assumed
to include two standard deviations above and
below the mean.
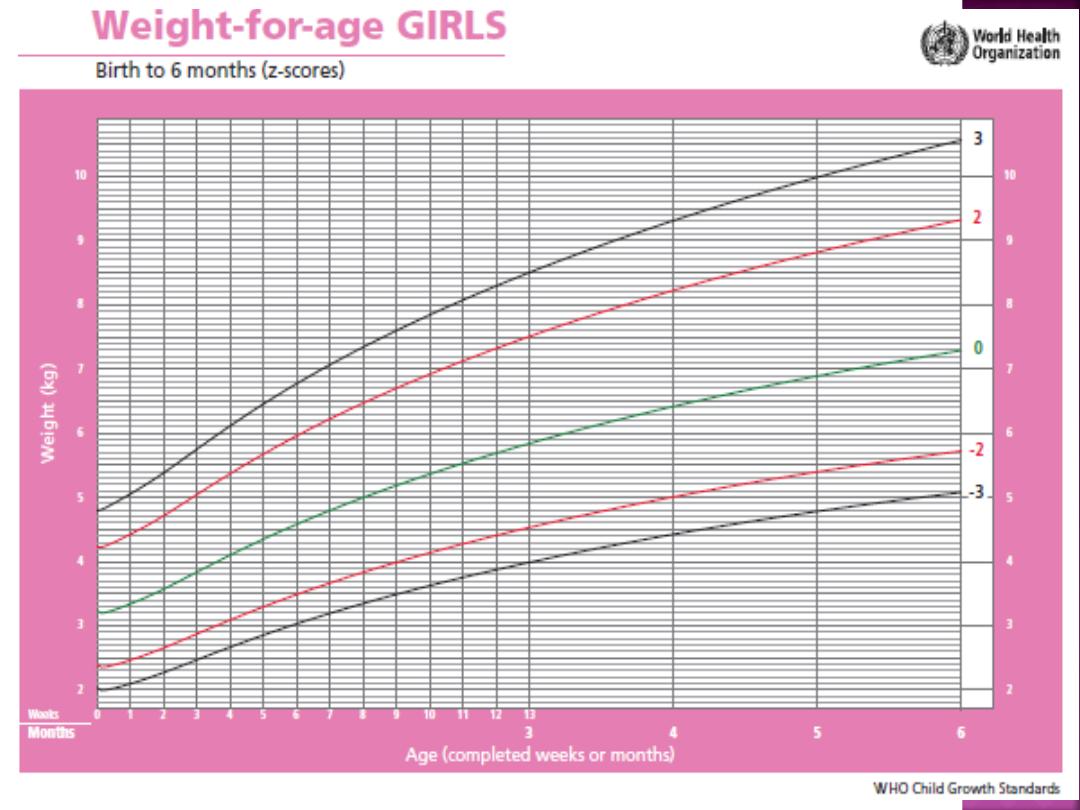
W.H.O.
GROWTH
STANDARDS
1 Length/height-for-age
2- Weight-for-age
3- Weight-for-length
4- Weight-for-height
5- Body mass index-for-age
6- Head circumference-for-age
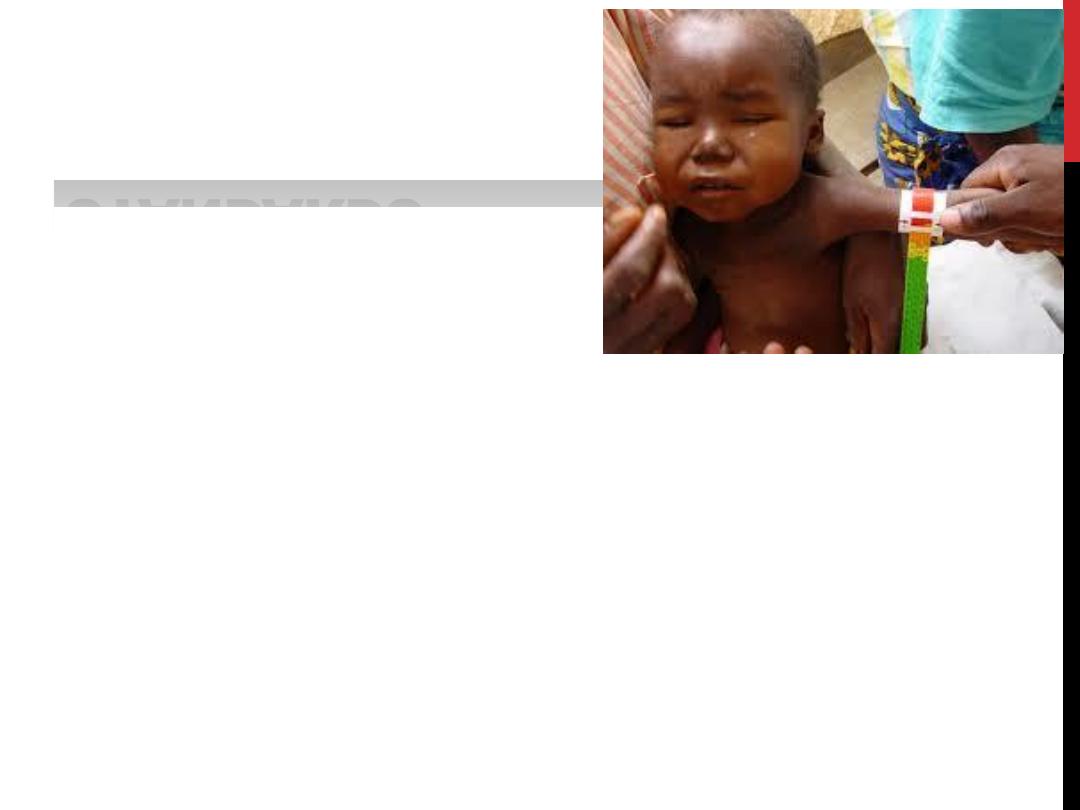
7- Arm circumference-for-age
8- Triceps skinfold-for-age
9- Subscapular skinfold-for-age
10- Growth velocity based on weight, length and head
circumference
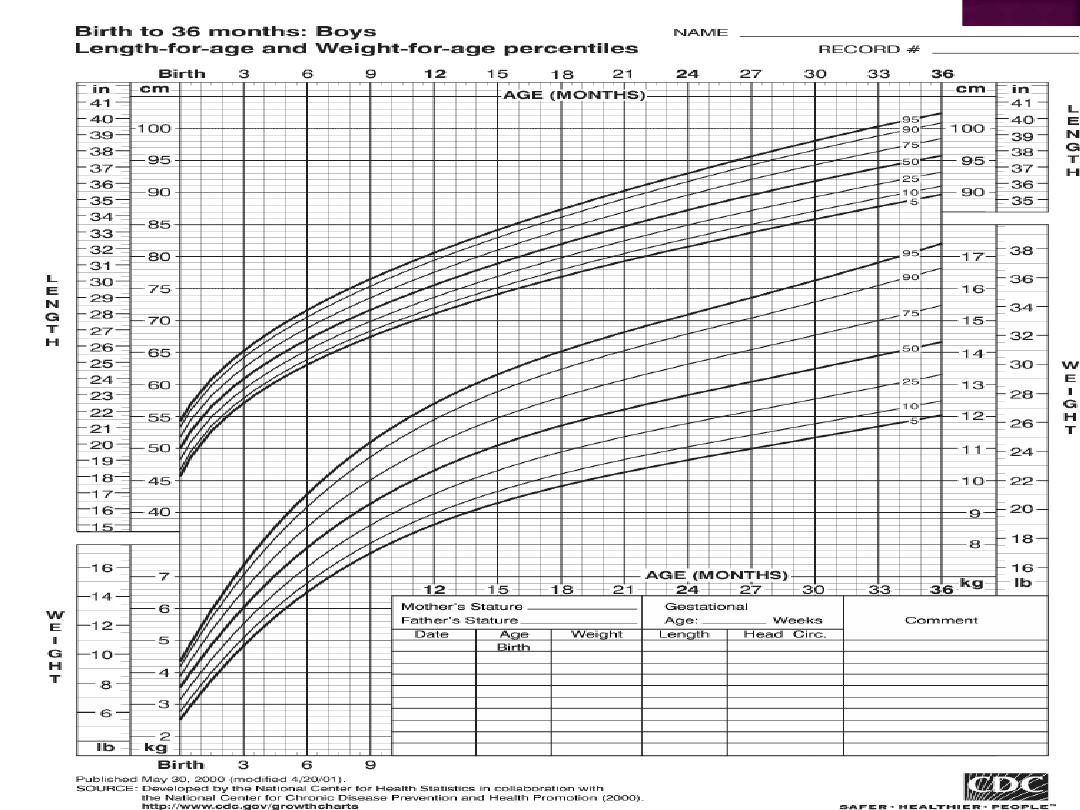
WEIGHT FOR
AGE
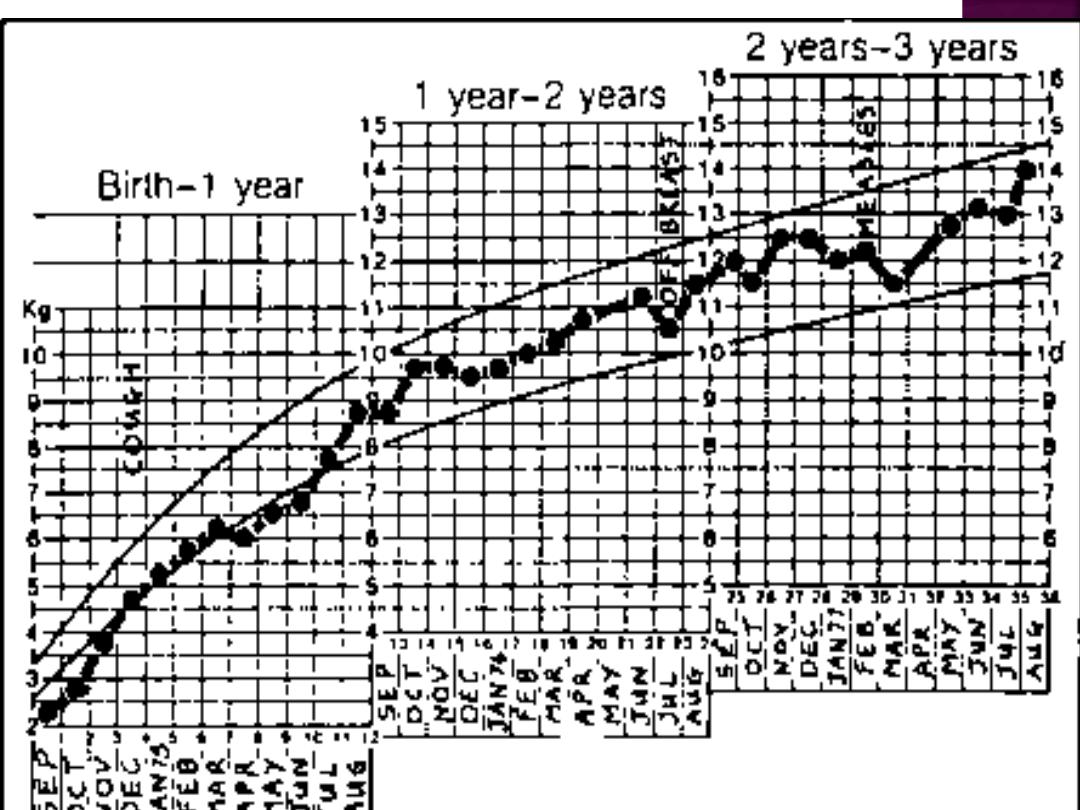
By far the commonest measurements are
those of weight. Target growth rates (often
called 'road to health') are generally based
on the WHO/NCHS reference values
measurement of weight and rate of gain in
weight, are the best single parameters for
assessing physical growth.
How often?
1- ideally monthly from birth to one year
2-every two months during the second year
3-every three months thereafter up to five
years of age.
A baby should gain at least 500 gm. wt. per
month in the first three months of life,(that
is the minimum),the children who gain less
weight are malnourished , it is usual for
babies to gain 1 kg a month , especially in
the first 3 months.
On an average double their birth weight by 5
months and treble it by the end of first year
and quadruple by the age of two.
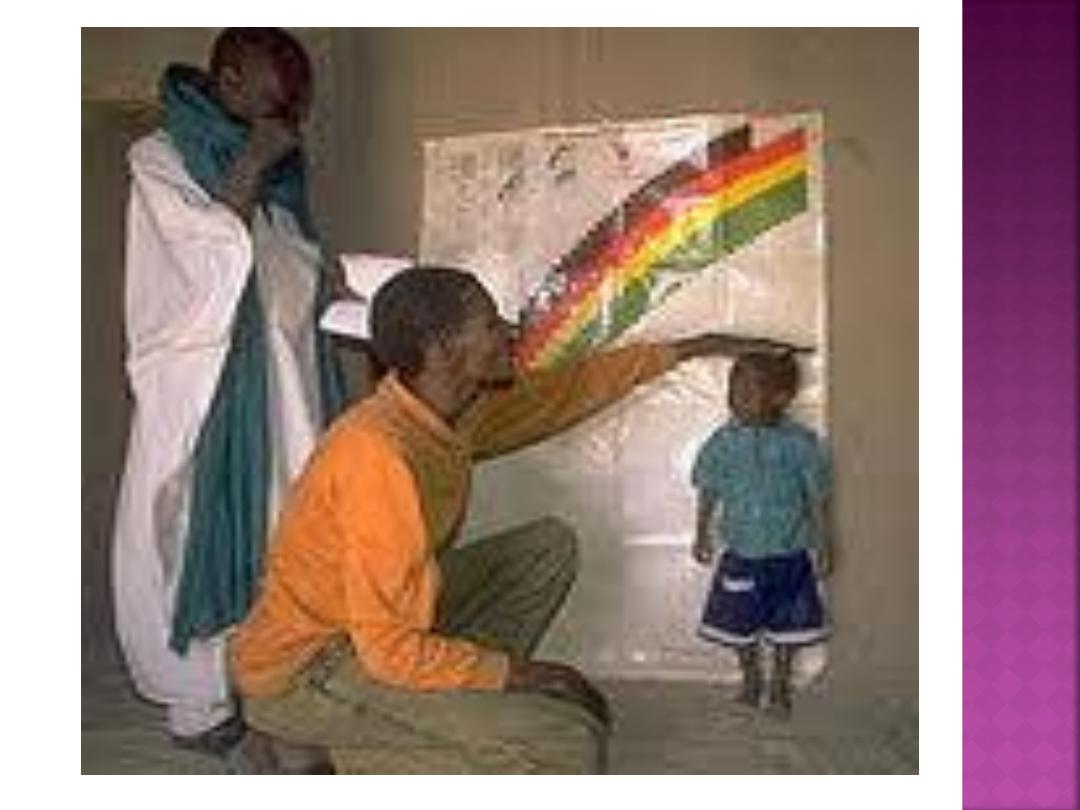
Height should be taken in a standing position
without foot wear ,If the height machine is
not available ,a measuring scale fixed to the
wall can be employed.
This arrangement is suitable for children 2
years and above.
The length of the baby at a birth is about
50cm ,it increased by about 25 cm during the
first year and by another 12cm during the
second year.


Height is a stable measurement of growth as
opposed to body weight .
Where as weight reflects only the present
health status of the child ,height indicates the
events in the past also.
The use of growth(height)centile chart is
valuable in studying the trend of height curve.
LOW HEIGHT FOR AGE IS KNOWN AS
NUTRITIONAL STUNTING OR DWARFING(it reflect
past or chronic malnutrition)
As weight-for-age is a composite index,
growth failure can be due to either a loss of
weight or a failure to gain in length, or both;
differentiating between these causes may be
problematic. Thus, in addition to weight,
measuring length would give more direct
information on linear growth. If length
measurements can be taken, then it would
be advisable to also monitor weight-for-
length.

Height and weight are interrelated, weight in
relation to height is now considered more
important than weight alone.
It helps to determine weather a child is within
range of “normal weight for his height”.
LOW WEIGHT FOR HEIGHT IS KNOWN AS
NUTRITIONAL WASTING OR
EMACIATION(acute malnutrition),it is
associated with an increased risk of
mortality and morbidity.
At birth the HC is about 35cm,it is about 2cm
more than the chest circumference, by 6-9
months the two measurements become
equal, after which the chest circumference
overtakes the head circumference.

The growth or” road-to-health” chart is a
visible display of a child physical growth and
development.
It is designed primarily for the longitudinal
follow-up(growth monitoring)of a child, so
that changes over time can be interpreted.

ARE STANDARDS
APPLICABLE TO ALL
CHILDREN?
The standards describe normal
child growth from birth to 5 years
under optimal environmental
conditions and can be applied to
all children everywhere,
regardless of ethnicity,
socioeconomic status and type of
feeding.
24
A growth chart has many potential uses:
1-For growth monitoring: which is of great
value in child health care.
2-Diagnostic tool: for identifying “high risk
children”.
3-Planning and policy making: to child health
care at the local and central levels.
4-Educational tool: because of it’s visual
character.
5-Tool for action: it helps the health workers
on the type of intervention that is needed.

6-Evaluation:it provide a good method to
evaluate the effectiveness of corrective
measures and the impact of a programme
for improving child growth and development.
7-Tool for teaching: of the importance of
adequate feeding .

GROWTH CHART HAS BEEN DESCRIBED AS A
PASSPORT TO CHILD HEALTH CARE.
It is a pathological state resulting from
relative or absolute deficiency or excess of
essential nutrients.
This could be detected by :
CLINICAL MANIFESTATIONS.
BIOCHEMICAL TESTS.
ANTHROPOMETRIC MEASURMENTS.
PHYSIOLOGICAL TESTS.
1-UNDERNUTRITION(MARASMUS AND
KWASHIORKOR).
2-OVERNUTRITION(e.g.OBESITY).
3-SPECIFIC DEFICIENCY:(VAD,IDA).
4-NUTRITIONAL IMBALANCE
.
Protein–energy malnutrition (or protein–calorie
malnutrition) refers to a form of
where there is inadequate
intake.
Types include:
(protein malnutrition predominant)
(deficiency in calorie intake)
Marasmic Kwashiorkor (marked protein
deficiency and marked calorie insufficiency signs
present, sometimes referred to as the most
severe form of malnutrition)
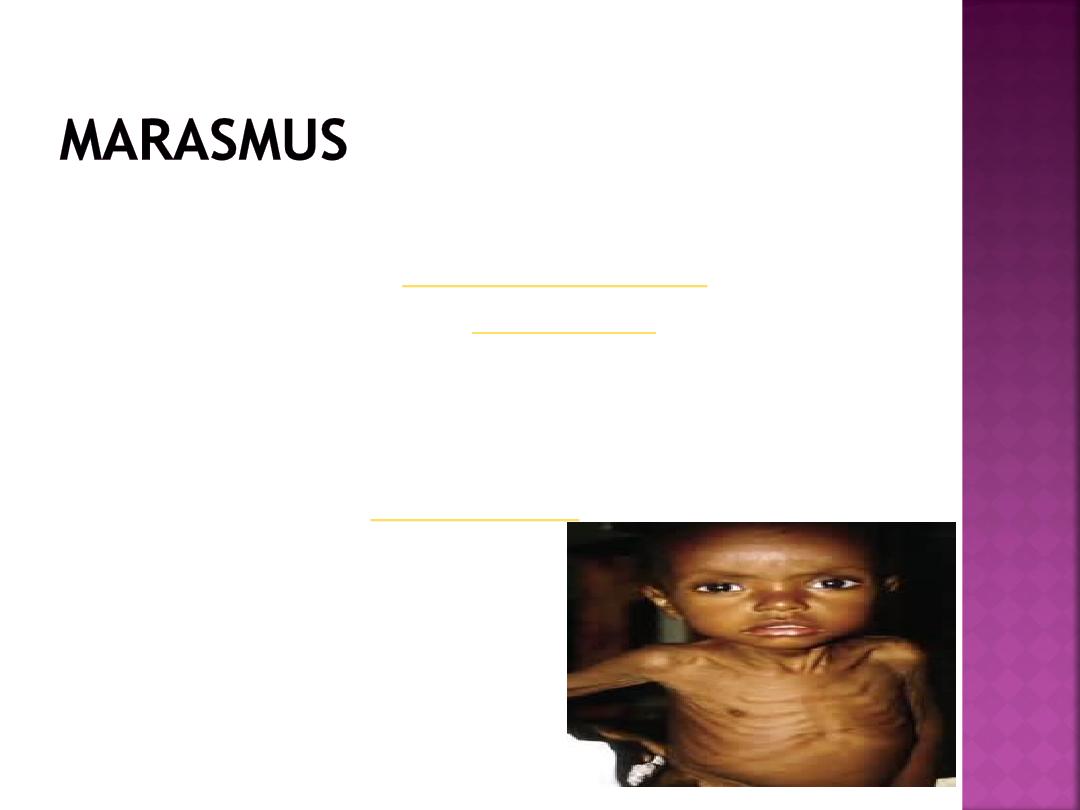
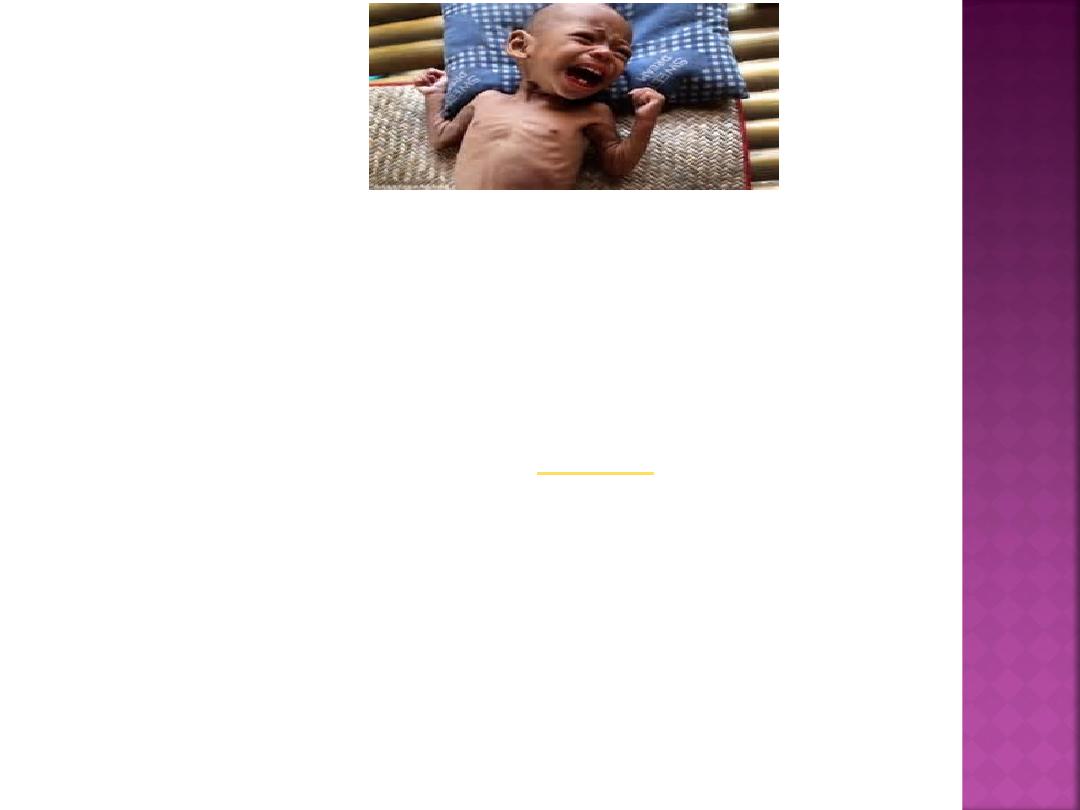
Marasmus is a form of severe malnutrition
characterized by
. A child
with marasmus looks
. Body weight
is reduced to less than 60% of the normal
(expected) body weight for the age.
Marasmus occurrence increases prior to age
1year, whereas
increases after 18 months.

It can be distinguished from kwashiorkor in
that kwashiorkor is protein deficiency with
adequate energy intake whereas marasmus is
inadequate energy intake in all forms,
including protein. Protein wasting in
kwashiorkor may lead to
The prognosis is better than it is for
kwashiorkor but half of severely
malnourished children die due to
unavailability of adequate treatment.
Marasmus is caused by a severe deficiency of
nearly all nutrients, especially protein and
carbohydrates
The malnutrition associated with marasmus leads
to extensive tissue and muscle wasting, as well
as variable edema. Other common
characteristics include dry skin, loose
hanging over the buttocks (
) and (
),
etc. There is also drastic loss of
(body fat) from normal areas of fat deposits like
and
.
–
typically they are hungry.
The face is wrinkled looks like worried old man.
The hair usually normal colour ,may be sparse.
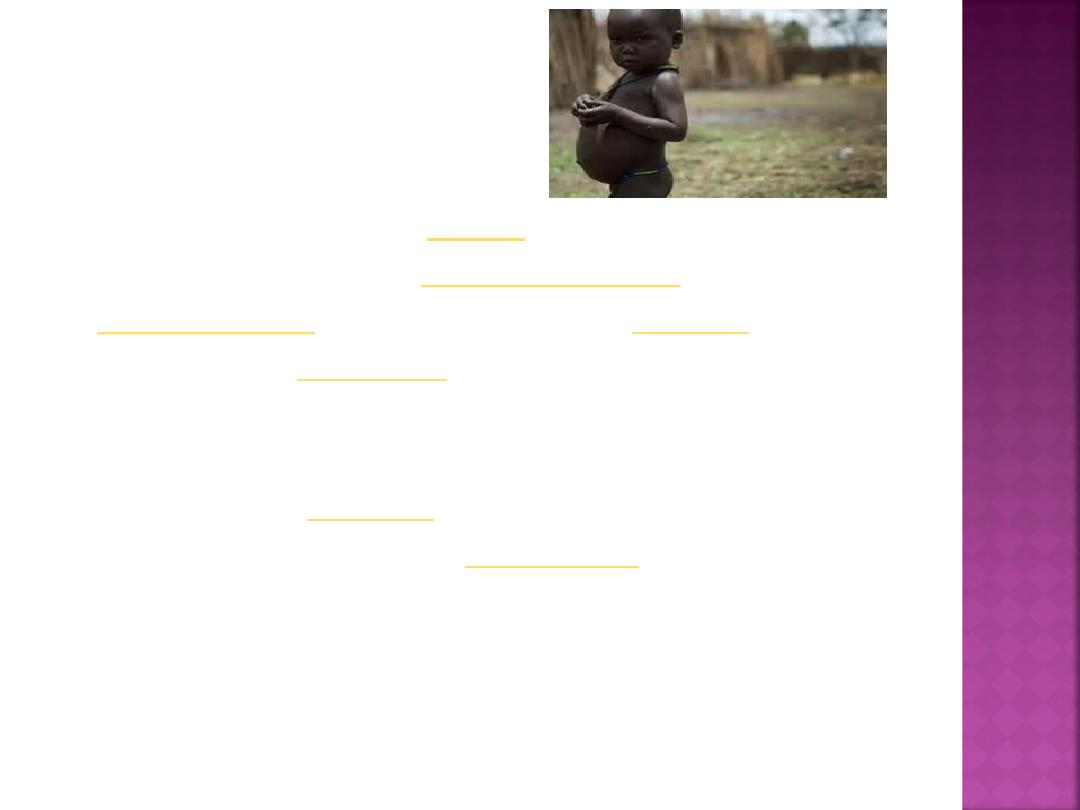
Kwashiorkor
Kwashiorkor is an
and more serious
form of childhood
characterized by
, ulcerating dermatosis,
and an enlarged liver with fatty infiltrates.
Sufficient calorie intake, but with
insufficient
consumption,
distinguishes it from
. Kwashiorkor
cases occur in areas of famine or poor food
supply. Cases in the developed world are
rare.

The defining sign of kwashiorkor in a
malnourished child is pedal edema (swelling
of the ankles and feet). Other signs include a
distended
, an enlarged liver with
fatty infiltrates, thinning hair, loss of teeth,
skin depigmentation and
. Children
with kwashiorkor often develop irritability
and
(no interest to food ,no
appetite).
The hair is pale , brownish , thin and break
easily.


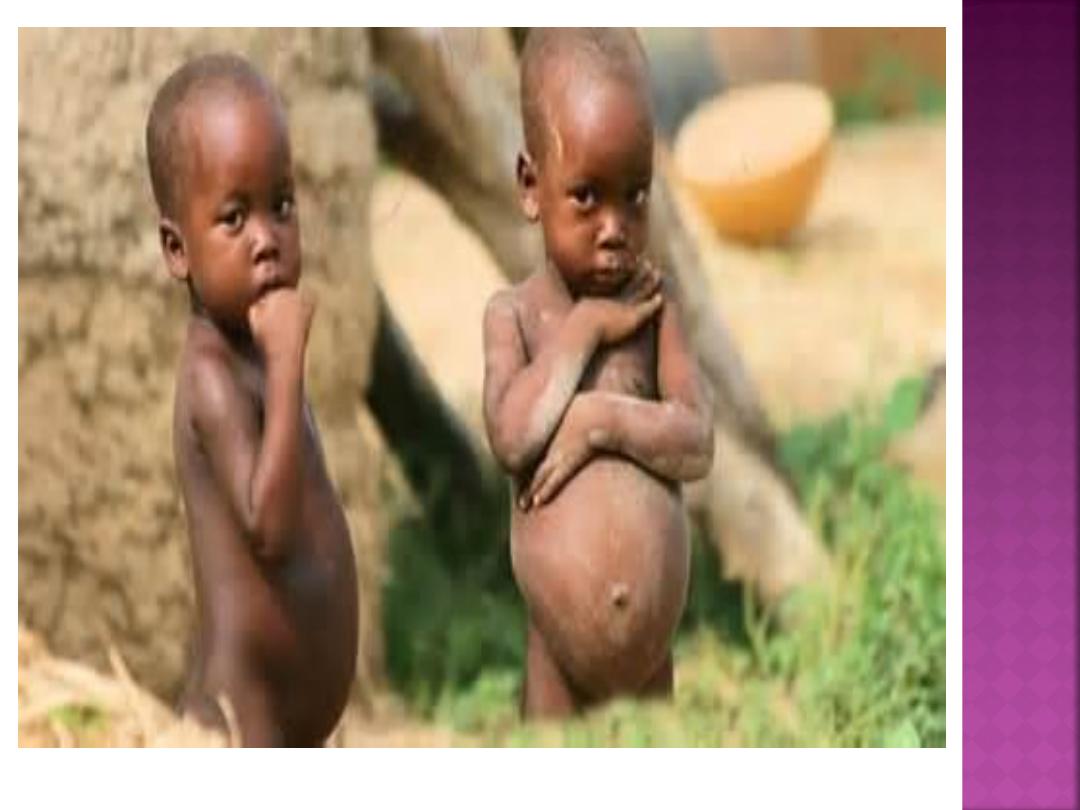
Kwashiorkor is a form of malnutrition due to
a deficiency in protein.
The typical swollen abdomen is due to two
causes: ascites because of
(low oncotic pressure), and enlarged fatty
liver.
A-health promotion:
1-Measures directed to pregnant and
lactating women(education,distribution of
supplements).
2-Promotion of breast feeding.
3-Development of low cost weaning food(the
child should be made to eat more food at
frequent intervals).
4-Measures to improves family diets.

5-Nutrition education-promotion of correct
feeding practices.
6-Home economics.
7-Family planning and spacing of births.
8-Family environment.

B-SPECIFIC PROTECTION:
1-The child’s diet must contain protein and
energy-rich foods milk,eggs,fresh fruits
should be given if possible.
2-Immunization.
3-Food fortification.
1-Periodic surveillance.
2-Early diagnosis of any lag in growth.
3-Early diagnosis and treatment of infection
and diarrhea.
4-Development of programmes for early
rehydration of children with diarrhea.
5-Development of supplementary feeding
programmes during epidemics.
6-Deworming of heavily infested children.
1-Nutritional rehabilitation services.
2-Hospital treatment.
3-Follow-up care.
