The Lower Urinary Tract:
Ureters:
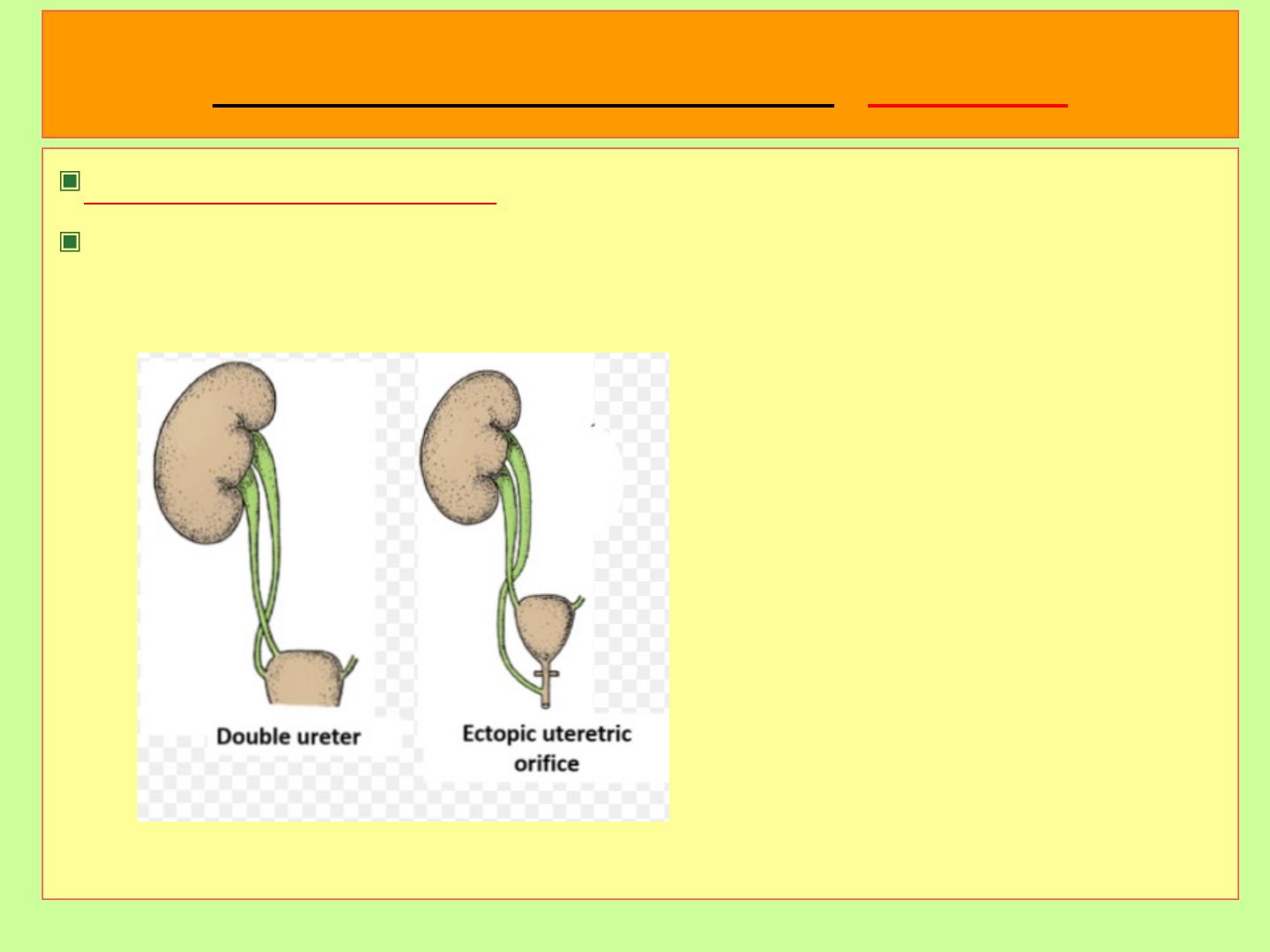
Congenital Anomalies:
Double ureters, uretropelvic junction obstruction, Diverticuli,
hydroureters which may be congenital or acquired.
inflammation of the urinary
bladder
• Inflammation of urinary bladder is called
cystitis
and it is
more common in females as compared to males. It is
usually due to:
• 1. Bacterial cause: E.coli, Proteus, Klebsiella,
Mycobacterium tuberculosis
• 2. Fungal cause: Candida albicans, seen with
immunosuppression
• 3. Hemorrhagic cystitis: Due to cytotoxic antitumor
drugs like cyclophosphamide and Adenovirus.
• 4. Radiation cystitis: Due to radiation exposure.
Clinical features
• Clinical features include:
1. Frequency – Requirement of urination every 15-20
minutes
2. Suprapubic pain – Pain in anatomical location of the
bladder
3. Dysuria - Painful or burning sensation or urination
This triad may be associated with fever and malaise.
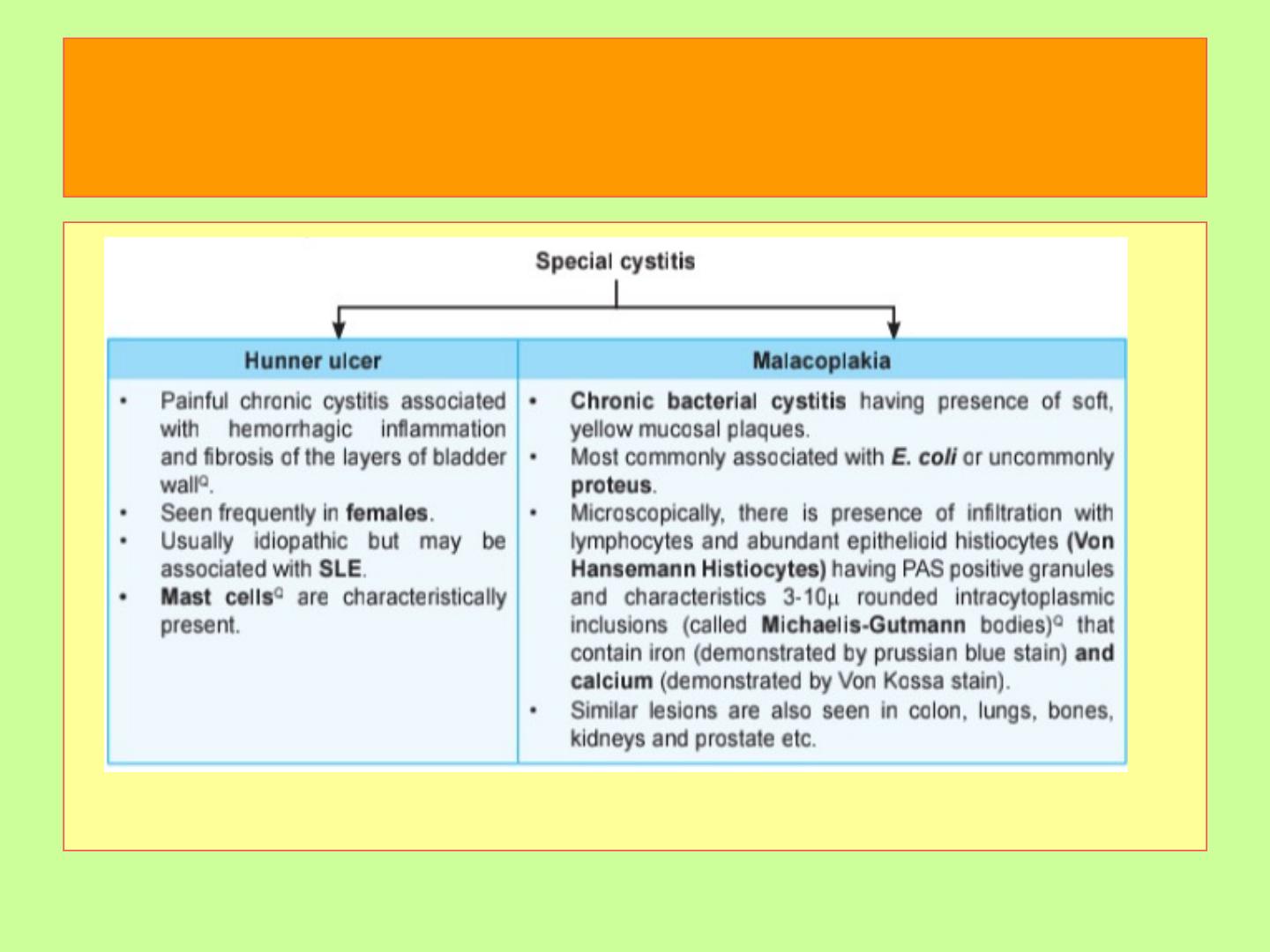
special forms of cystitis
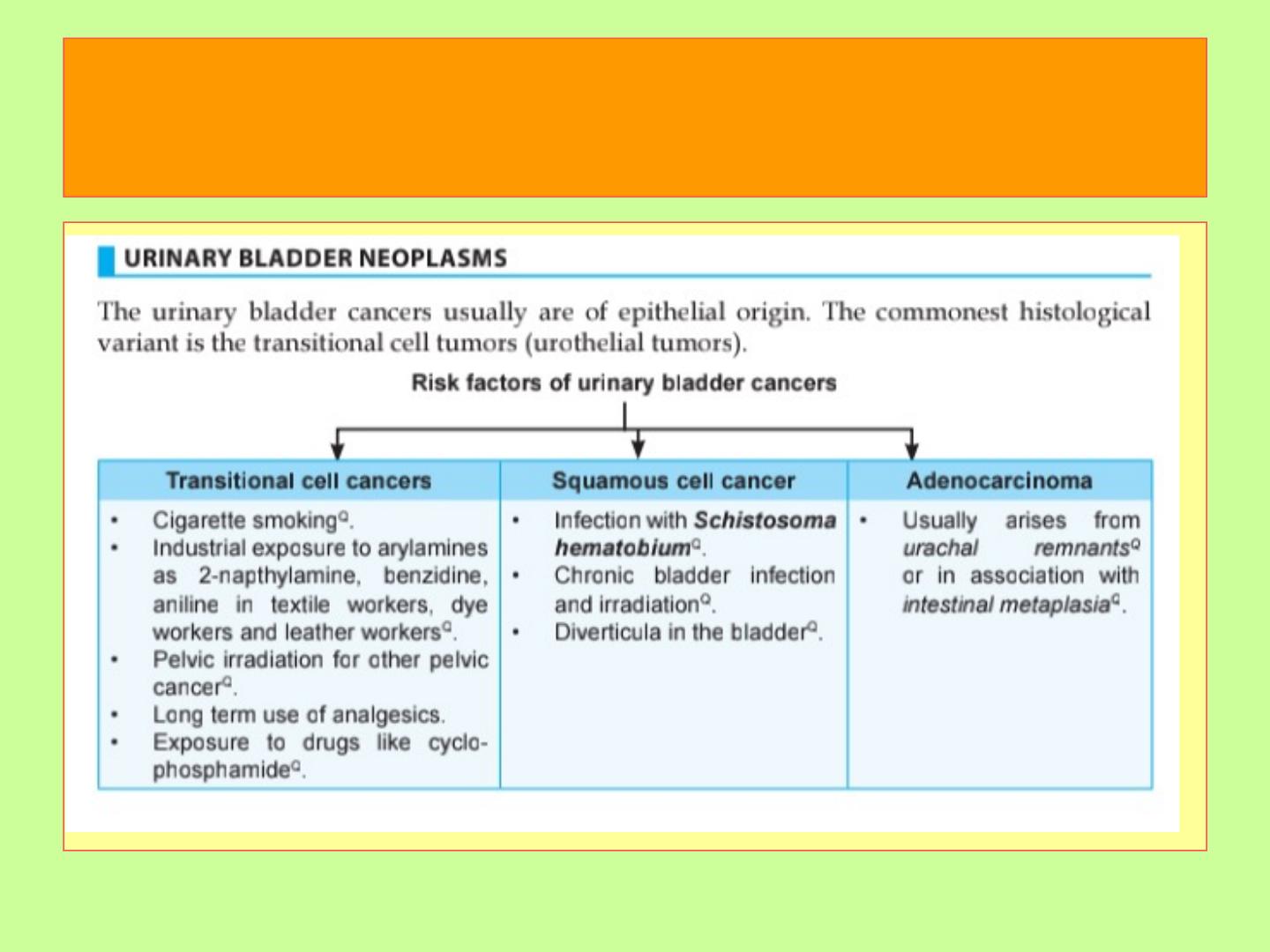
Urinary Bladder Neoplasms
•About 95% of them are of
epithelial
origin, the remainder being
mesenchymal.
•Most epithelial tumors are composed of
transitional
type.
Transitional cell tumours
•These represent about
90%
of all bladder tumors and range from
benign lesions to aggressive cancers.
•Many of these tumors are multifocal at presentation.
•Although most commonly seen in the bladder, they may be seen
in the pelvis, ureters, and urethra.
Types of urinary bladder
neoplasms
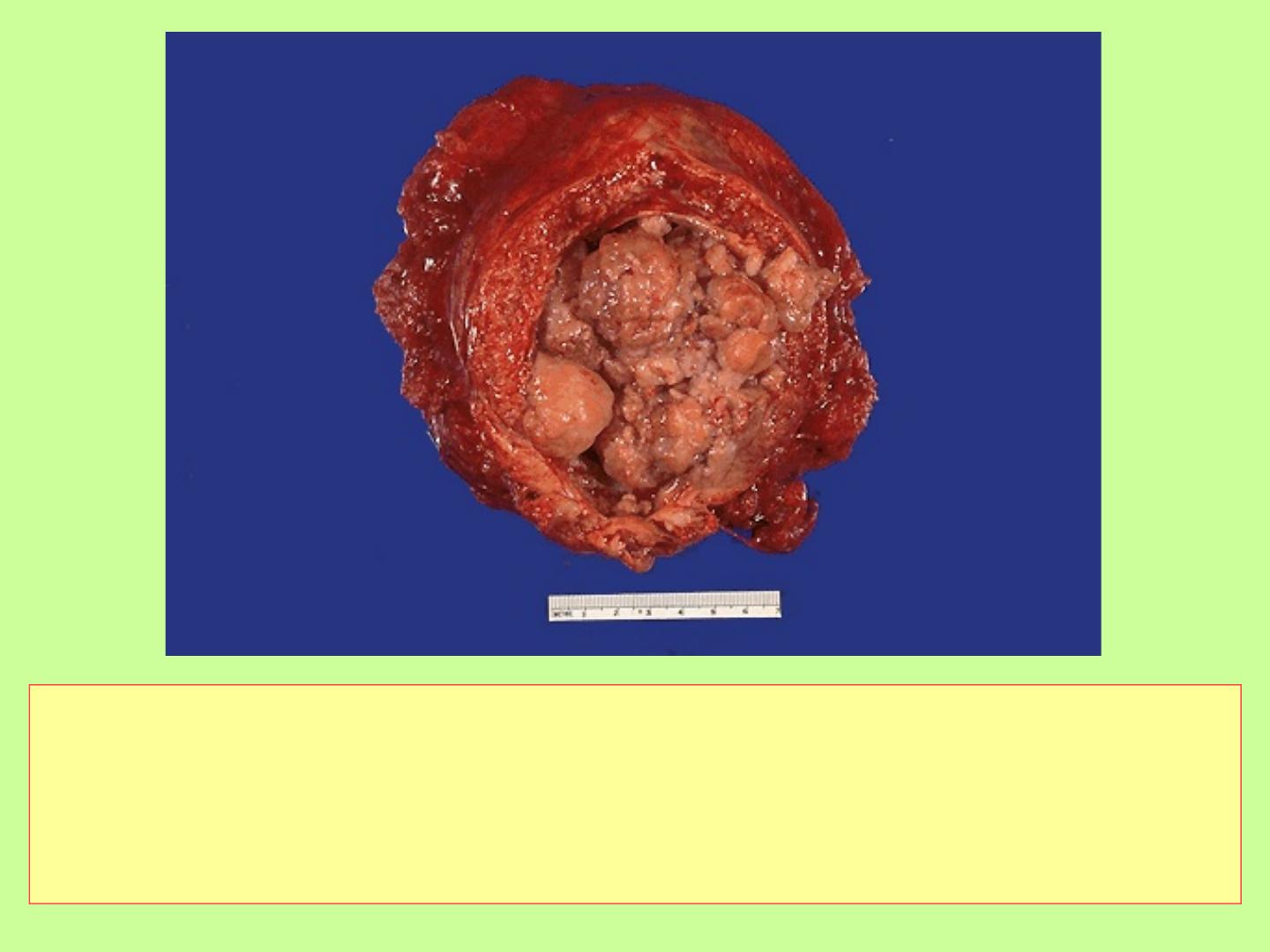
The gross patterns of TCC vary from purely papillary to nodular or
flat. The tumors may also be invasive or non. Papillary lesions
range in size between 1-5cm. They may be multicentric. most
tumours arise from the
lateral or posterior
walls at the bladder base
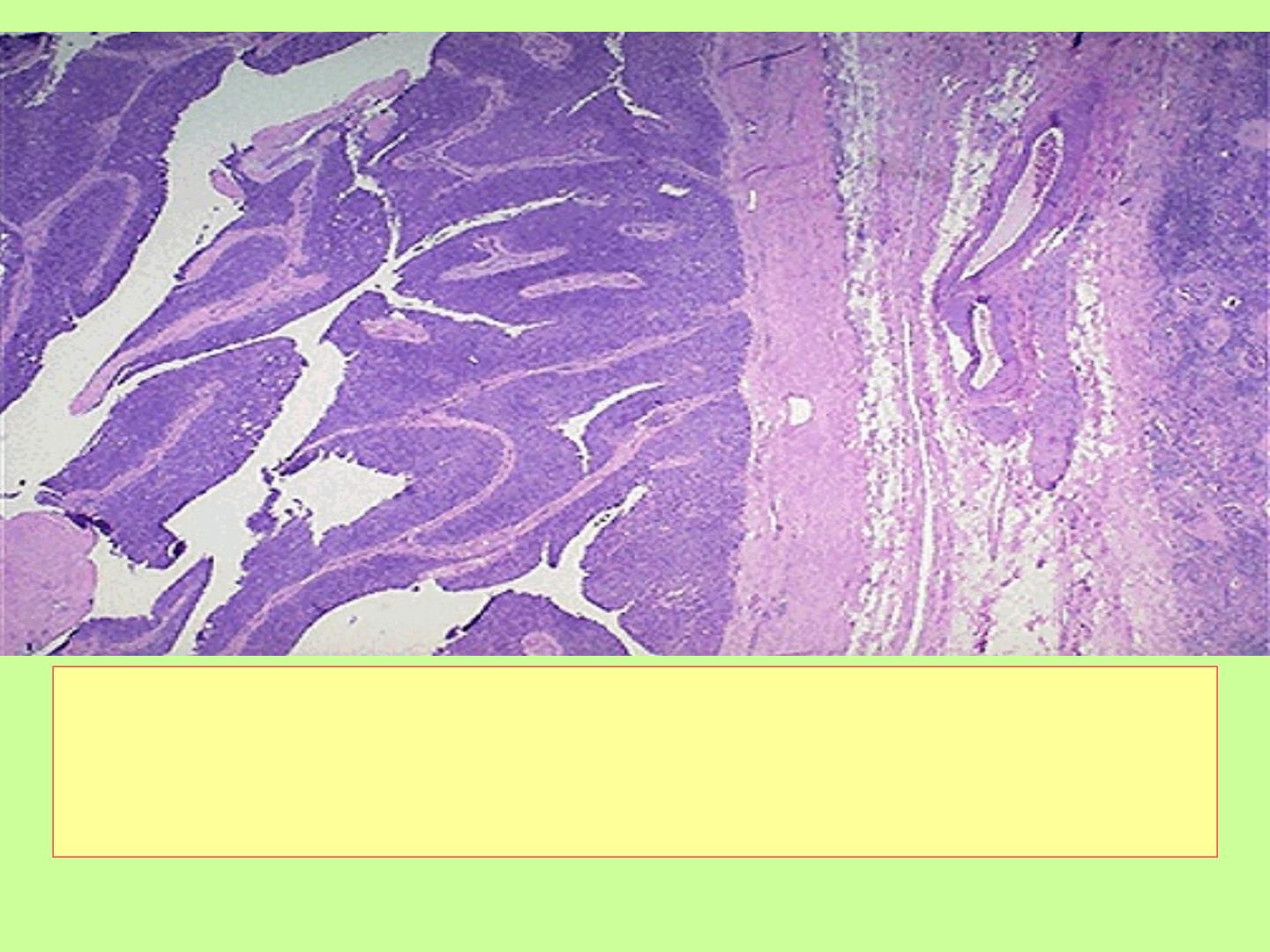
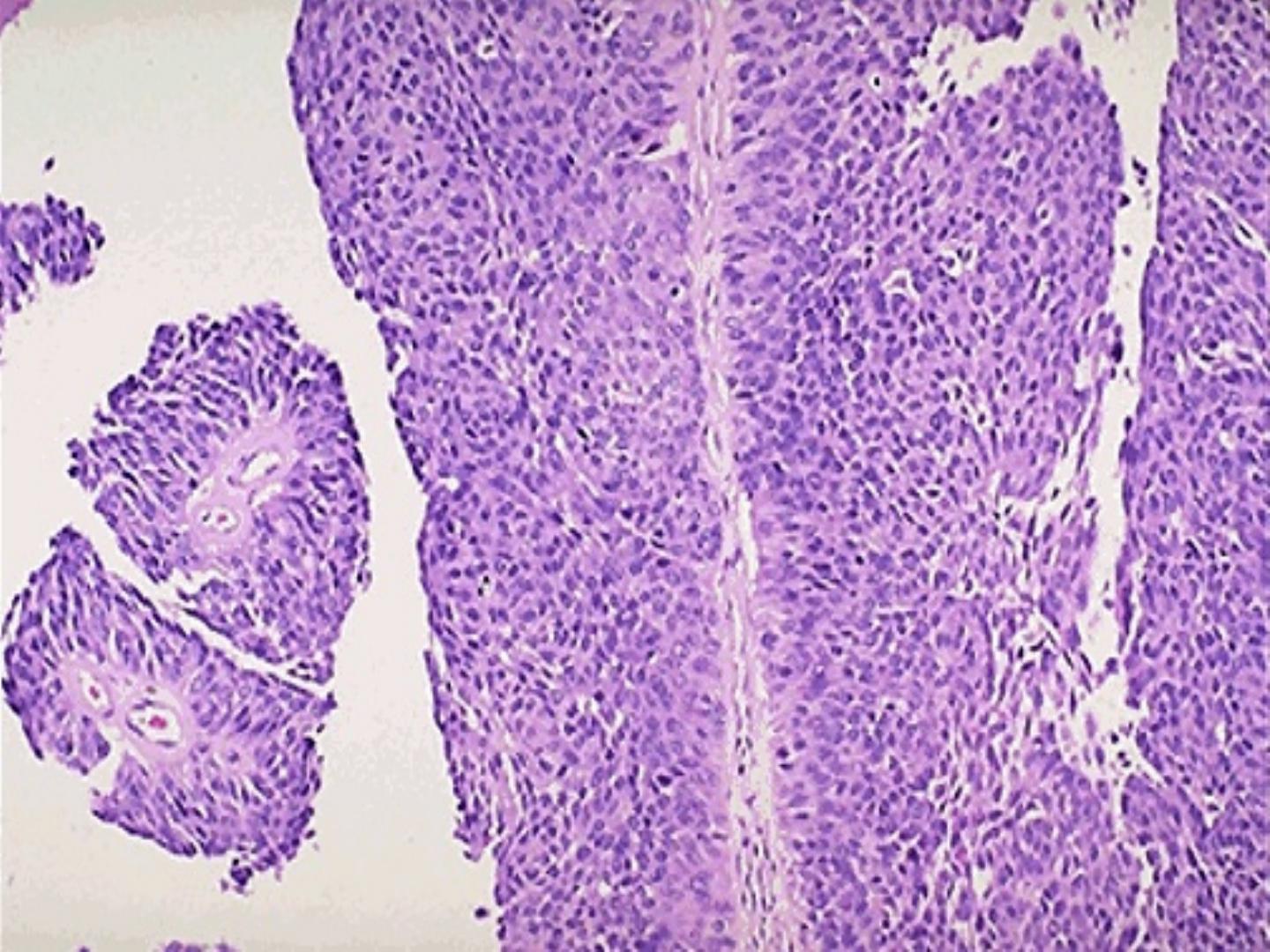
• A transitional cell carcinoma of the urothelium is
shown here at low power to reveal the frond-like
papillary projections of the tumor
Grading of the tumors
• A most recent classification was adopted by
the WHO in 2004,
1. Urothelial papilloma.
2. Urothelial neoplasm of low malignant
potential.
3. Papillary urothelial carcinoma, grade I.
4. Papillary urothelial carcinoma, grade II.
5. Papillary urothelial carcinoma, grade III.

Pathologic Staging Of Bladder Carcinoma
Noninvasive, papillary Ta
Carcinoma in situ Tis
Lamina propria invasion T1
Muscularis propria invasion T2
Microscopic extravesicle invasion T3a
Grossly apparent extravesicle invasion T3b
Invades adjacent structures T4
Clinical course
• Bladder tumors classically produce
painless
hematuria
.
• Frequency, urgency and dysuria may be experienced
as well.
• When ureteral orifice is involved, pyelonephritis or
hydronephrosis may follow.
• The risk of recurrence and progression is related to
several factors; tumor size, stage, grade,
multifocality, prior recurrence rate, and associated
dysplasia and/or carcinoma in situ in the surrounding
mucosa.
Mesenchymal Tumors
• Benign, collectively are rare, the most common is
leiomyoma
.
• Malignant, sarcomas are extremely rare. The most
common in infancy and childhood is embryonal
Rhabdomyosarcoma
. In adults,
Leiomyosarcoma
is
the predominant one.
Secondary Tumors
:
• Are most often as direct extension from
adjacent organs.
• Lymphoma may also involve the bladder as
part of systemic disease.
