Gastric Polyps
Hyperplastic polyps (the most frequent; 90%) are small, sessile and multiple in about 25% of cases. There is hyperplasia of the surface epithelium and cystically dilated glandular tissue.Increase size…..increases risk for cancer esp. If larger than 1.5 cm.
Gastric Adenoma( Adenomatous polyp)
50 – 60 yr.Males more
Almost always occur on a background of chronic gastritis with atrophy and intestinal metaplasia.
Risk for of adenocarcinoma related to the size of the lesion and is particularly elevated with lesions greater than 2 cm in diameter.
Overall, carcinoma may be present in up to 30% of gastric adenomas.
Gastric Adenocarcinoma
Geography: 20 times higher in Japan, Chile, Costa than USALower socioeconomic classes
partial gastrectomies
Decreasing in USA..??
Pathogenesis
• Helicobacter pylori Infection: this generally increases the risk five- fold.• Adenomatous polyps: 40% of adenomas harbor carcinomatous foci; also adjacent carcinoma is found in relation to adenomatous polyps in 30% of the cases
• 3. Environmental factors: when families migrate from high-risk to low-risk areas (or the reverse), successive generations acquire the level of risk that prevails in the new environments
• 4. Autoimmune gastritis, like H. pylori infection, increases the risk of gastric cancer
Gross features
The most common location of gastric carcinomas is the pyloric antrum (50%). A favored location is the lesser curvature.
Depth of invasion is the most important determinant of prognosis. Early gastric carcinoma is defined as "a lesion confined to the mucosa and submucosa." Advanced gastric carcinoma is a neoplasm extending into the muscular wall.
The three macroscopic growth patterns of gastric carcinoma, which may be evident at both the early and advanced stages, are:
1. Fungating (exophytic)
2. Flat or depressed
3.Ulcerative (excavated).
4.Uncommonly, a broad region of the gastric wall or the entire stomach is extensively infiltrated by malignancy, creating a rigid, thickened "leather bottle," termed linitis plastica.
Microscopic features
There are two main microscopic type of gastric carcinoma; intestinal and diffuse.The intestinal variant is composed of neoplastic glands with mucin in their lumina.
The diffuse variant is composed of mucus-containing cells, which do not form glands, but infiltrate the mucosa and wall as scattered individual and small clusters of cells, In this variant, mucin formation expands the malignant cells and pushes the nucleus to the periphery, creating"signet ring" morphology.
Sometimes, there is excessive mucin production that generates large mucin lakes (mucinous carcinoma).
Infiltrative tumors often evoke a strong desmoplastic reaction (fibrosis), in which the scattered cells are embedded; the fibrosis creates local rigidity of the wall.
Whatever the microscopic type, all gastric carcinomas eventually penetrate the wall to involve the serosa and spread to regional and more distant lymph nodes.
For obscure reasons, gastric carcinomas frequently metastasize to the supraclavicular (Virchow) node as the first clinical manifestation of an occult neoplasm
The tumor can also metastasize to the periumbilical region to form a subcutaneous nodule. This nodule is called a Sister Mary Joseph nodule .
Lymphoma
5% of all gastric malignancies
Most are MALTomas
Carcinoid Tumor
Arise from neuroendocrine organs (e.g. pancreas) and neuro-endocrine-differentiated gastrointestinal epithelia (e.g., G-cells).
A majority are in GIT(mostly SI) then lung & brochi.
May cause chronic atrophic gastritis, and Zollinger-Ellison syndrome
Can cause Carcinoid syndrome
Caused by vasoactive substances secreted by the tumor that cause cutaneous flushing, sweating, bronchospasm, colicky abdominal pain, diarrhea, & right-sided cardiac valvular fibrosis.Seen in 10% of patients & is strongly associated with metastatic disease.
Most common carcinoid in the GIT, particularly the small intestine.
The single most important prognostic factor is location e.g. Tumors of the small intestine tend to be most aggressive, while those of the appendix are almost always benign.Gastrointestinal stromal tumor (GIST)
is the most common mesenchymal tumor of the abdomen, occurs most often in the stomach; it arises from benign pacemaker cells, also known as the interstitial cells of Cajal.A majority of tumors have activating mutations in either the c-KIT ( CD117) in 95% & is diagnostically useful
Small & large intestine
CONGENITAL ANOMALIES
duplication of the small intestine or colon;
malrotation of the entire bowel;
omphalocele (birth of an infant with herniation of abdominal contents into a ventral membranous sac related to umbilicus); heterotopia of pancreatic tissue or gastric mucosa;
atresia and stenosis; imperforate anus (due to failure of the cloacal diaphragm to rupture).
Meckel diverticulum
Results from failure of involution of the vitelline duct, which embryologically connects the lumen of developing gut to the yolk sac. The small pouch lies on the antimesenteric side of the bowel, usually 30 cm proximal to the ileo-cecal valve.It consists of mucosa, submucosa, and muscularis propria. The mucosal lining may be that of normal small intestine, but heterotopic gastric mucosa or pancreatic tissue are frequently found.
Meckel diverticula are present in 2% of the normal population, but most remain asymptomatic.
When peptic ulceration occurs in the small intestinal mucosa adjacent to the heterotopic gastric mucosa, intestinal bleeding or symptoms simulating those of an acute appendicitis may result. Other complications include intussusception, incarceration, or perforation.
Intestinal obstruction
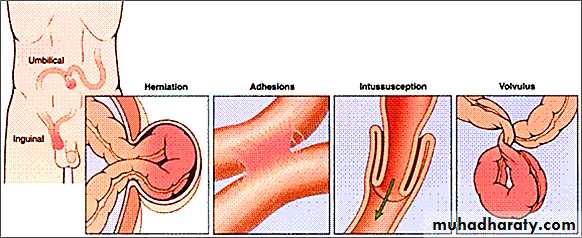
80% is mechanical:Hernias
Adhesions
Intussusception
Volvulus
20 % by
Tumor
Infarction
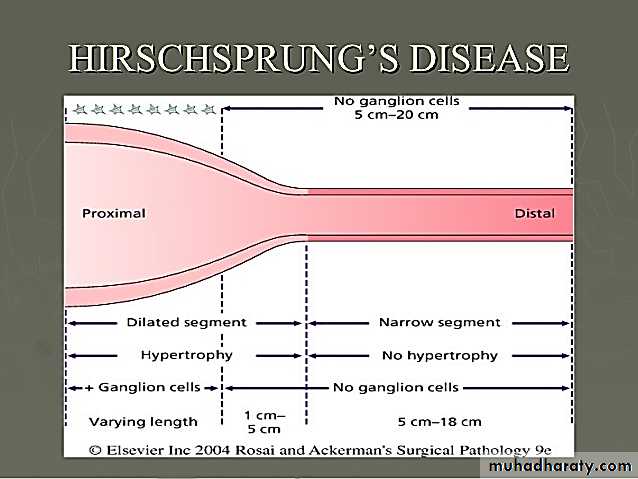
Hirschsprung Diseasecongenital aganglionic megacolon
1 of 5000Failure to pass meconium….intestinal obstruction
Defect in colonic innervations
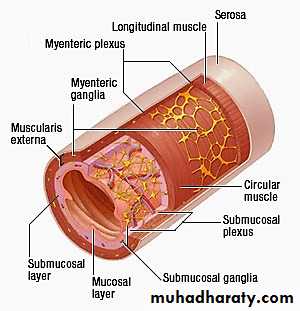
Lack of segment that lacks both the Meissner submucosal plexus and the Auerbach myenteric plexus (“aganglionosis”)…..distal obstruction & proximal dilatation
Always affect rectum but length is variable
Dx: biopsy
Abdominal Hernia
Abdominal herniation may occur through any weakness or defect in the wall of the peritoneal cavity, including inguinal and femoral canals, umbilicus, and sites of surgical scarring.Hernia sac
External herniation
Incarceration
Strangulation
Ischemic Bowel Disease
Mucosal
Mural infarction
Transmural
Causes
Atherosclerosis
Aortic aneurysm
Hypercoagulable states
Oral contraceptive use
Embolization of cardiac vegetations or aortic
atheromas.
Shock
Systemic vasculitides e.g. WG,PAN,CMV infection
Cause may be arterial or venous obstruction.
Site:most common at the splenic flexure, sigmoid colon, and rectum; these are watershed zones where two arterial circulations terminate.
Angiodysplasia
It occurs most often in the cecum or right colonAfter the sixth decade of life.
Less than 1% in the adult population
May cause major episodes of lower intestinal bleeding; intestinal hemorrhage may be chronic and intermittent or acute and massive.
The pathogenesis is unknown.
Hemorrhoids
5% population (rare before 30)Causes:
Any increases in intra abdominal pressure
Constipation &straining
Pregnancy
Portal hypertension.
May be Internal or external
SOLITARY RECTAL ULCER SYNDROME
This is an inflammatory condition of the rectum resulting from motor dysfunction of the anorectal musculature, in particular impaired relaxation of the anorectal sling.The latter may create sharp angulation of the anterior rectal wall. Abrasion of the overlying rectal mucosa creates an oval ulcer and surrounding mucosal inflammation. Associated partial prolapse of the rectal mucosa is common. Patients experience rectal bleeding & mucus discharge
Diarrheal Diseases
Diarrhea is an increase in stool mass, frequency, or fluidity (typically to volumes > 200 mL/day.
Dysentery : Painful, bloody, small-volume diarrhea
Diarrhea can be classified into four major
Secretory: isotonic stool and persists during fasting.
Osmotic e.g. lactase deficiency due unabsorbed luminal solutes. Abates with fasting.
Malabsorptive: inadequate nutrient absorption is associated with steatorrhea and is relieved by fasting.
Exudative :due to inflammatory disease and characterized by purulent, bloody stools that continue during fasting.
THE MALABSORPTION SYNDROMES
Malabsorption is characterized by defective absorption of fats, fat-soluble and other vitamins, proteins, carbohydrates, electrolytes and minerals, and water.The most common clinical presentation is chronic diarrhea, and the hallmark of malabsorption is steatorrhea (excessive fecal fat content).
The malabsorptive disorders most commonly encountered are
• 1-Celiac disease• 2-Pancreatic insufficiency
• 3-Crohn disease
Pancreatic insufficiency
Primarily from chronic pancreatitis or cystic fibrosis, is a major cause of defective intraluminal digestion that leads to diarrhea and steatorrhea.
Celiac Disease
Celiac disease (gluten-sensitive enteropathy, GSE) is a chronic disease, in which there is a characteristic mucosal lesion of the small intestine and impaired nutrient absorption, which improves on withdrawal of wheat gluten from the diet.Pathogenesis
The fundamental disorder in celiac disease is sensitivity to gluten component called gliadin, which is a protein present in wheat and closely related grains (e.g. oat).
There is a T-cell mediated chronic inflammatory reaction, which develops as a consequence of a loss of tolerance to gluten.
Interplay between genetic predisposing factors, the host immune response, and environmental factors, is central to disease pathogenesis.
The small intestinal mucosa, when exposed to gluten, accumulates intraepithelial CD8+ T cells and large numbers of lamina propria CD4+ T cells, which are sensitized to gliadin.
Gliadin is deamidated by the enzyme transglutaminase; the resultant peptides are recognized by CD4+ T cells. This leads to secretion of interferon γ, which damages enterocytes.
Pathological features
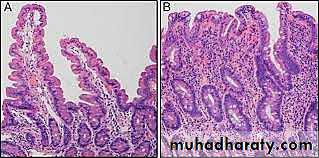
By endoscopy, the duodenal mucosa appears flat (normally shows mucosal folds).Biopsies demonstrate enteritis with partial or total loss of villi (partial villous atrophy or completely flat mucosa respectively)
The surface epithelium shows degeneration, loss of the microvillus brush border, and an increased number of intraepithelial lymphocytes.
The crypts exhibit increased mitotic activity and are hyperplastic, so that, despite villous atrophy, the overall mucosal thickness remains the same.
The lamina propria has an overall increase in plasma cells and lymphocytes.
Although the above changes are characteristic of celiac disease, they can be mimicked by other diseases, most notably tropical sprue.
Mucosal histology usually reverts to normal or near-normal following gluten exclusion from the diet.
Dermatitis herpetiformis (DH) is a characteristic itchy skin-blistering disease can occur in some patients with celiac disease.
•
Definitive diagnosis of celiac disease rests on
• 1-clinical documentation of malabsorption• 2-demonstration of the intestinal lesions by small bowel biopsy and
• 3-Definite improvement in both symptoms and mucosal histology on gluten withdrawal from the diet.
• 4-If there is doubt about the diagnosis, gluten challenge (reintroduction of gluten to the diet) followed by rebiopsy has been advocated.
• 5-Serologic tests, mentioned above, are used for screening or treatment follow-up.
Most patients with celiac disease who adhere to a gluten-free diet remain well indefinitely and ultimately die of unrelated causes. However, there is a long-term risk of malignant disease, which includes small intestinal non-Hodgkin lymphoma (moderate risk),
small intestinal adenocarcinoma, and esophageal squamous cell carcinoma (50- to 100-fold higher risk than the general population).
Tropical Sprue (Postinfectious Sprue)
This condition is a celiac-like disease that occurs almost exclusively in people living in or visiting the tropics.Malabsorption usually becomes apparent within days or a few weeks. The condition improves on treatment with broad-spectrum antibiotics. This supports an infectious etiology.
Intestinal lymphoma does not appear to be associated with this disorder (cf. celiac disease).
Whipple Disease
Whipple disease is a rare systemic disease that principally affects the intestine, central nervous system, and joints. It is caused by the bacterium Tropheryma whippelii. The bacteria proliferate preferentially within macrophages.Disaccharidase (Lactase) Deficiency
The disaccharidases, of which the most important is lactase, are located in the apical cell membrane of the absorptive epithelial cells. Congenital lactase deficiency is a very rare condition, but acquired lactase deficiency is common. Incomplete breakdown of the disaccharide lactose into its monosaccharides glucose and galactose leads to osmotic diarrhea from the unabsorbed lactoseAbetalipoproteinemia
This condition is a rare autosomal recessive inborn error of metabolism and characterized by a defect in the synthesis and export of lipoproteins from intestinal mucosal cells. The failure to absorb certain essential fatty acids leads to lipid membrane defects, The disease becomes manifest in infancy and is dominated by failure to thrive, diarrhea, and steatorrhea.
Infectious Diarrhea
Cholera:G-
Enterotoxin
Secretory diarrhea
Campylobacter jejuni
Most common bacterial enteric pathogen in developed countries and also causes traveler’s diarrhea.Non invasive
Shigella
Most common causes of bloody diarrhea
Infective dose as few as 100 organisms
Salmonella spp infection
Typhoid fever (S.Typhi & S.paratyphi)
Non typhoid causes food poisoning & gastroenteritis
Pseudomembranous colitis
AB therapy disrupts the normal microbiota and allows C. difficile to colonize and grow.Rotavirus
The most common cause of severe childhood diarrhea and diarrheal mortality worldwide.
The diarrhea is secondary to loss of mature enterocytes, resulting in malabsorption as well as secretion.
Parasitic and protozoal infections
Affect over half of the world’s population on a chronic or recurrent basis