Gastrointestinal tract (Lab 15)
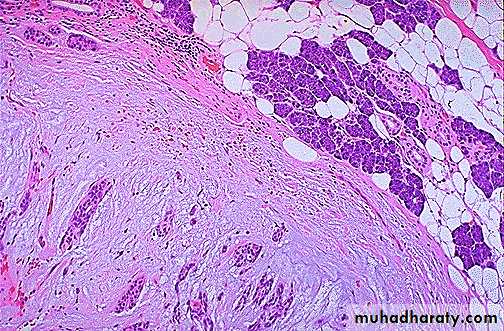
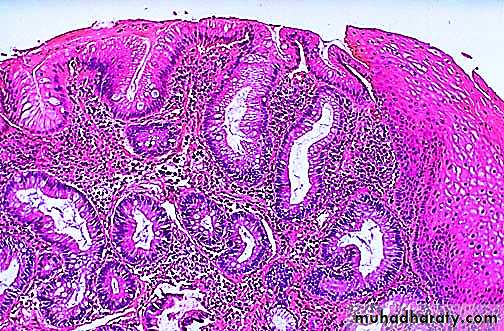
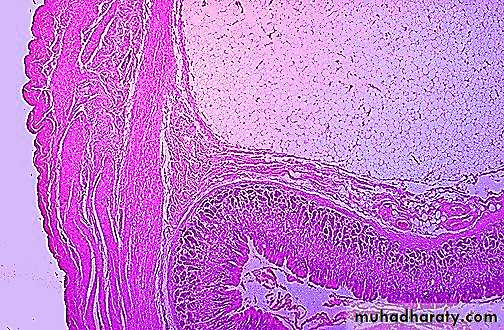
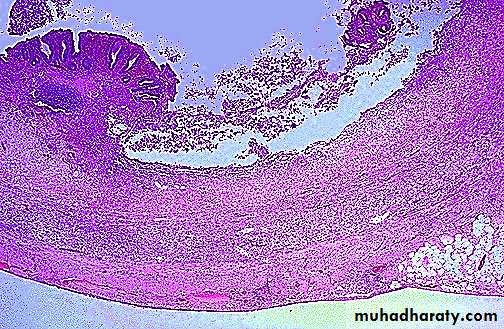
A pleomorphic adenoma of parotid gland is seen here at high magnification next to a portion of adjacent normal parenchyma at the upper right. The neoplasm is a mixed proliferation of both ductal epithelium and a chondroid/myxomatous stroma. Infrequently, a carcinoma can arise in a pleomorphic adenoma.Another cause for inflammation is a so-called "Barrett's esophagus" in which there is gastric-type mucosa above the gastroesophageal junction. Note the columnar epithelium to the left and the squamous epithelium at the right. This is "typical" Barrett's mucosa, because there is intestinal metaplasia as well (note the goblet cells in the columnar mucosa).
This is Barrett's esophagus with some dysplasia of the columnar epithelium. There is a long-term risk for adenocarcinoma. The short term problem is inflammation and/or ulceration.
The normal tan upper esophageal mucosa is at the far left. The distal esophagus is replaced by Barrett mucosa, producing a darker, slightly erythematous gross appearance. In the distal esophagus has arisen a large ulcerating adenocarcinoma that extends into the upper stomach. Adenocarcinomas can arise in Barrett esophagus.
At the lower end of the esophagus (which has been turned inside out at autopsy) are linear dark blue submucosal dilated veins known as varices. In patients with portal hypertension (usually micronodular cirrhosis from chronic alcoholism), the submucosal esophageal veins become dilated (form varices). These varices are prone to bleed.
A large varix runs nearly the entire length of the esophagus, shown inverted here. Bleeding points have been treated with sclerotherapy, which is injection of a chemical that causes sclerosis of the vein.
This irregular reddish, ulcerated exophytic mid-esophageal mass as seen on the mucosal surface is a squamous cell carcinoma. Risk factors for esophageal squamous carcinoma include mainly smoking and alcoholism in the U.S.
This is a more typical acute gastritis with a diffusely hyperemic gastric mucosa. There are many causes for acute gastritis: alcoholism, drugs, infections, etc.
A 1 cm acute gastric ulcer is shown here in the upper fundus. The ulcer is shallow and sharply demarcated, with surrounding hyperemia. It is probably benign. However, all gastric ulcers should be biopsied to rule out a malignancy.
Here are small, shallow gastric ulcerations known as "stress ulcers" because they can appear in patients with a variety of stressful conditions, including trauma, burns, sepsis, and shock. Anti-inflammatory drugs such as aspirin and non-steroidal anti-inflammatory drugs may play a role in their appearance.
Microscopically, the ulcer here is sharply demarcated, with normal gastric mucosa on the left falling away into a deep ulcer whose base contains infamed, necrotic debris. An arterial branch at the ulcer base is eroded and bleeding.
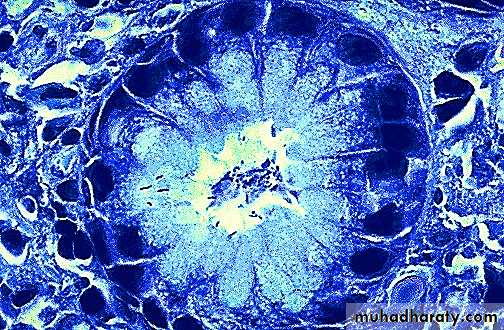
Chronic gastritis and peptic ulcer disease are often accompanied by infection with Helicobacter pylori. This small curved to spiral rod-shaped bacterium is found in the surface epithelial mucus of most patients with active gastritis. The rods are seen here with a methylene blue stain.
Here is a gastric ulcer in the center of the picture. It is shallow and is about 2 to 4 cm in size. This ulcer on biopsy proved to be malignant, so the stomach was resected as shown here.
This is an example of linitis plastica, a diffuse infiltrative gastric adenocarcinoma which turns the stomach into a shrunken "leather bottle" appearance.
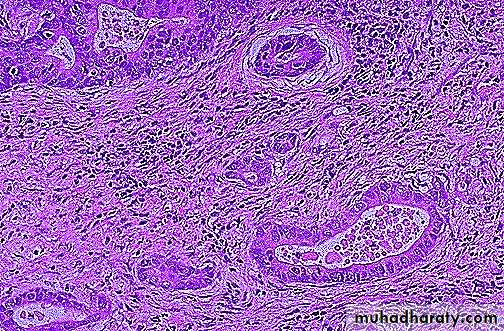
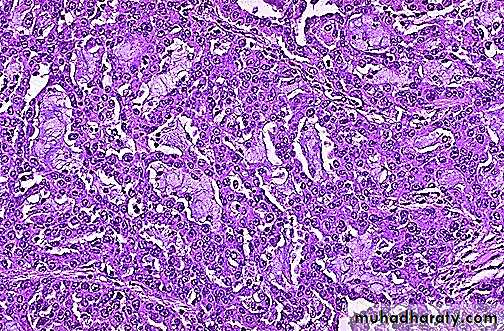
At higher magnification, the neoplastic glands of gastric adenocarcinoma demonstrate mitoses, increased nuclear/cytoplasmic ratios, and hyperchromatism. There is a desmoplastic stromal reaction to the infiltrating glands.
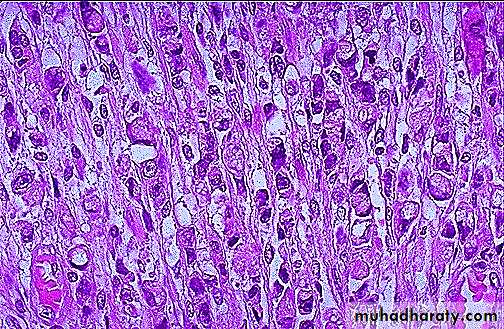
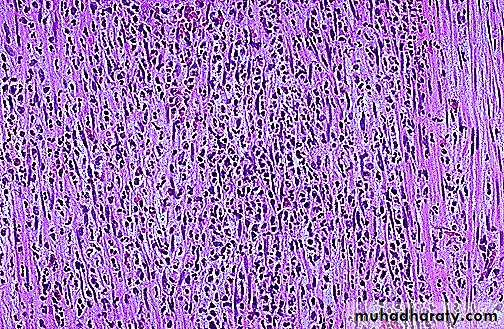
At high power, this gastric adenocarcinoma is so poorly differentiated that glands are not visible. Instead, rows of infiltrating neoplastic cells with marked pleomorphism are seen. Many of the neoplastic cells have clear vacuoles of mucin.
This is a signet ring cell pattern of adenocarcinoma in which the cells are filled with mucin vacuoles that push the nucleus to one side, as shown at the arrow.
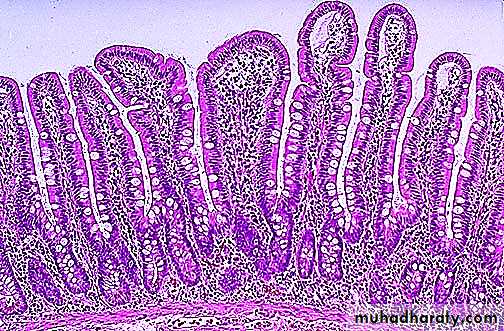
This is the normal appearance of small intestinal mucosa with long villi that have occasional goblet cells. The villi provide a large area for digestion and absorption.
The dark red infarcted small intestine contrasts with the light pink viable bowel. The forceps extend through an internal hernia in which a loop of bowel and mesentery has been caught. This is one complication of adhesions from previous surgery. The trapped bowel has lost its blood supply. The most common causes for bowel obstruction (in developed nations) are:
This is an example of cecal volvulus. Volvulus is a twisting of the bowel. Volvulus is most common in adults, where it occurs with equal frequency in small intestine (around a twisted mesentery) and colon (in either sigmoid or cecum which are more mobile). In very young children, volvulus almost always happens in the small intestine.
The small intestinal mucosa demonstrates marked hyperemia as a result of ischemic enteritis. Such ischemia most often results from hypotension (shock) from cardiac failure, from marked blood loss, or from loss of blood supply from mechanical obstruction (as with the bowel incarcerated in a hernia or with volvulus or intussusception). If the blood supply is not quickly restored, the bowel will infarct.
The mucosal surface of the bowel seen here shows early necrosis with hyperemia extending all the way from mucosa to submucosal and muscular wall vessels. The submucosa and muscularis, however, are still intact.
This small discreet yellow subserosal mass is a lipoma of the small intestine found incidentally at autopsy.
Microscopic examination reveals the lipoma at the upper right to be composed of cells essentially resembling mature adipose tissue. Benign tumors closely resemble the cell of origin.
Non-Hodgkin's lymphomas of the bowel do occur uncommonly. The multifocal irregular tan-to-brown masses seen here on the mucosal surface
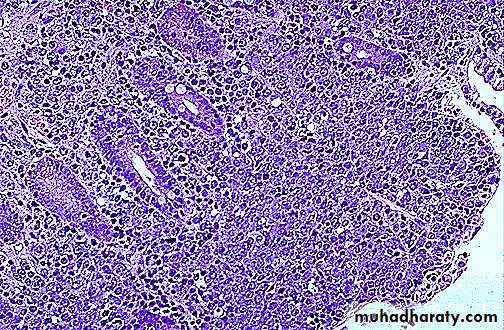
The large blue non-Hodgkin's lymphoma cells can be seen infiltrating through the mucosa.
This is a Meckel's red ulcer is seen). Meckel's diverticula may contain ectopic gastric mucosa (whichdiverticulum from an adult that was excised because of blood loss from ulceration (a small can ulcerate surrounding mucosa with pain and bleeding) or ectopic pancreas (which is of no consequence unless it forms a mass large enough to predispose to intussusception).
Here is a congenital duplication of the bowel. This was an incidental finding in an adult. However, such anomalies are more likely to be found in association with other anomalies and be identified soon after birth (if not before). The duplicated segment is seen above the normal ileum. It is just a blind-ended segment.
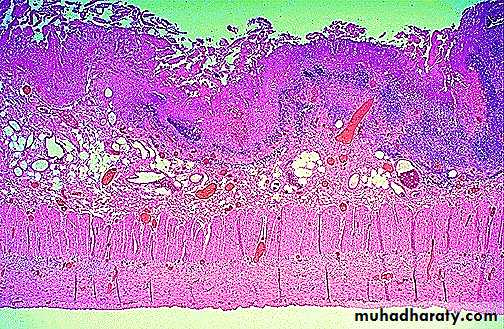
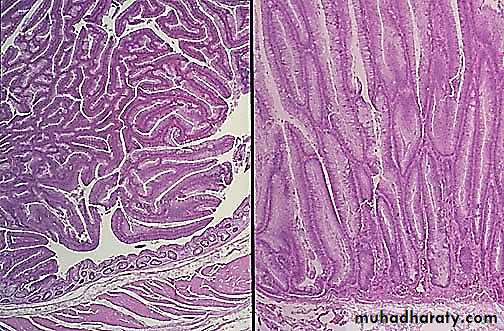
Normal small intestinal mucosa is seen at the left, and mucosa involved by celiac sprue at the right. There is blunting and flattening of villi with celiac disease, and in severe cases a loss of villi with flattening of the mucosa as seen here
This is an example of pseudomembranous enterocolitis. The mucosal surface of the colon seen here is hyperemic and is partially covered by a yellow-green exudate. The mucosa itself is not eroded. Broad spectrum antibiotic usage (such as clindamycin) and/or immunosuppression allows overgrowth of bacteria such as Clostridium dificile or S. aureus or fungi such as Candida to cause this appearance.
Microscopically, the pseudomembrane is seen to be composed of inflammatory cells, necrotic epithelium, and mucus in which the overgrowth of microorganisms takes place. The underlying mucosa shows congested vessels, but is still intact.
Here is the resected appendix from laparoscopic surgery. Note that there is some tan-yellow exudate, but the main features of this early acute appendicitis are edema and hyperemia.
Microscopically, acute appendicitis is marked by mucosal inflammation and necrosis.
Neutrophils extend into and through the wall of the appendix in a case of acute appendicitis. Clinically, the patient often presents with right lower quadrant abdominal pain. Rebound tenderness is noted on physical examination. An elevated WBC count is usually present.
Here is a small adenomatous polyp in the middle of the colon seen here. It has smooth surfaces and is discreet. These are common. Small ones are virtually always benign. Those larger than 2 cm carry a much greater risk for development of a carcinoma.
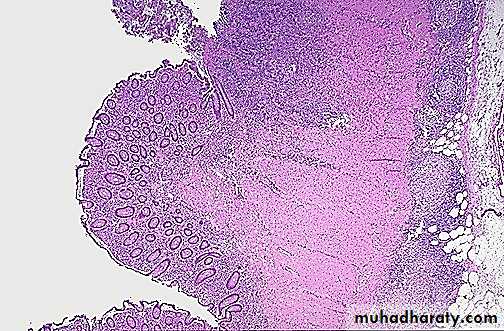
This is a small adenomatous polyp (tubular adenoma) seen microscopically to have more crowded, disorganized glands than the normal underlying colonic mucosa. Goblet cells are less numerous and the cells lining the glands of the polyp have hyperchromatic nuclei. However, it is still well-differentiated and circumscribed, without invasion of the stalk, and is benign.
This adenomatous polyp has a hemorrhagic surface (which is why they may first be detected with stool occult blood screening) and a long narrow stalk.
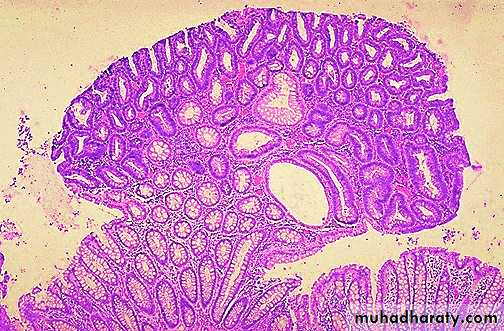
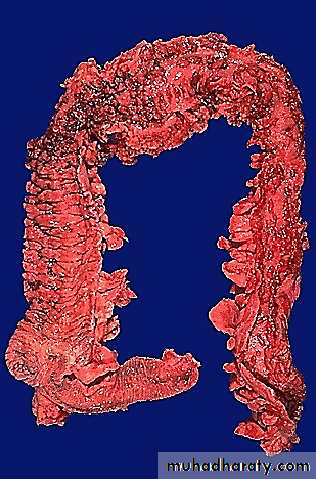
his is familial polyposis coli. The mucosal surface of the colon is essentially a carpet of small adenomatous polyps. Of course, even though they are small now, there is a 100% risk over time for development of adenocarcinoma, so a total colectomy is done, generally before age 20. Patients with this disorder inherit a faulty adenomatous polyposis coli (APC) gene.
Here are multiple adenomatous polyps of the cecum. A small portion of terminal ileum appears at the right. This is a patient with hereditary non-polyposis colon carcinoma (HNPCC) syndrome. Compared to adenomatous polyposis coli (APC), in HNPCC there are fewer polyps and an older age for development of carcinoma. The defect in HNPCC is the inheritance, in an autosomal dominant fashion, of a faulty DNA mismatch repair gene, and most HNPCC tumors demonstrate microsatellite instability (variations in dinucleotide repeat sequences).
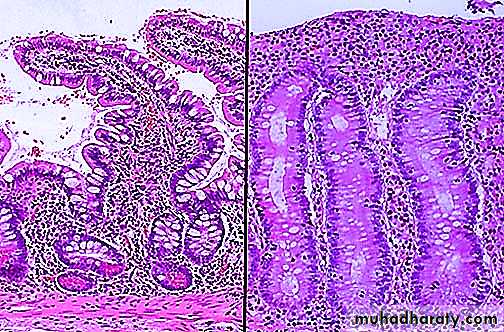
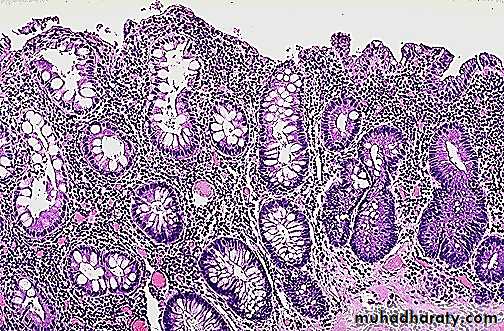
A microscopic comparison of normal colonic mucosa on the left and that of an adenomatous polyp (tubular adenoma) on the right is seen here. The neoplastic glands are more irregular with darker (hyperchromatic) and more crowded nuclei. This neoplasm is benign and well-differentiated, as it still closely resembles the normal colonic structure.
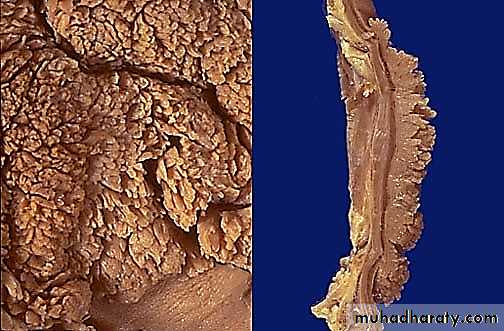
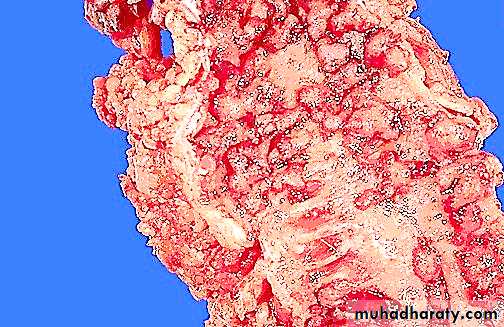
The gross appearance of a villous adenoma is shown above the surface at the left, and in cross section at the right. Note that this type of adenoma is sessile, rather than pedunculated, and larger than a tubular adenoma (adenomatous polyp). A villous adenoma averages several centimeters in diameter, and may be up to 10 cm.
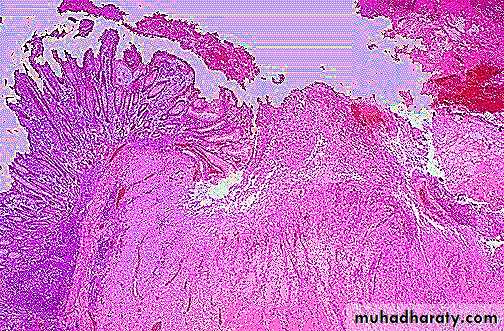
Microscopically, a villous adenoma is shown at its edge on the left, and projecting above the basement membrane at the right. The cauliflower-like appearance is due to the elongated glandular structures covered by dysplastic epithelium. Though villous adenomas are less common than adenomatous polyps, they are much more likely to have invasive carcinoma in them (about 40% of villous adenomas).
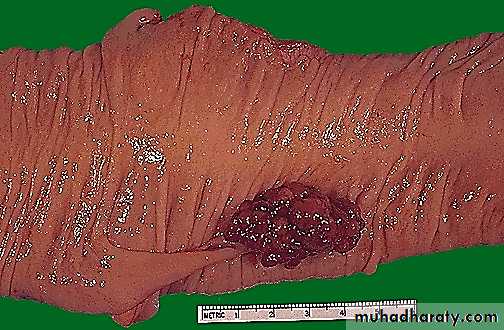
An adenocarcinoma of the colon appears above the label at the left. There is a heaped up margin of tumor at each side with a central area of ulceration.
The encircling mass of firm adenocarcinoma in this colon at the left is typical for adenocarcinomas arising in the descending colon. A change in stool or bowel habits can be created by the mass effect.
Here is another example of an adenocarcinoma of colon. This cancer is more exophytic in its growth pattern. Thus, one of the complications of a carcinoma is obstruction (usually partial).
Microscopically, a moderately differentiated adenocarcinoma of colon is seen here. There is still a glandular configuration, but the glands are irregular and very crowded. Many of them have lumens containing bluish mucin.
Seen here is a mucocele of the appendix in which the lumen is markedly dilated. It was filled with a clear, viscous mucoid material.These probably represent true neoplasms, most often a mucinous cystadenoma
Several diverticula are seen along the length of the descending colon. Focal weaknesses in the bowel wall and increased lumenal pressure contribute to the formation of diverticula.
At low magnification, a colonic diverticulum has a central lumen with surrounding mucosa, while the wall (lacking a muscularis) is attenuated. The narrow neck of the diverticulum may become eroded.
Seen here is the anus and perianal region with prominent prolapsed true (internal) hemorrhoids. Hemorrhoids consist of dilated submucosal veins which may thrombose and rupture with hematoma formation
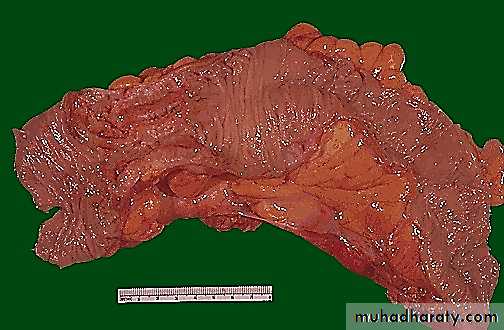
This is another example of Crohn's disease involving the small intestine. Here, the mucosal surface demonstrates an irregular nodular appearance with hyperemia and focal superficial ulceration.
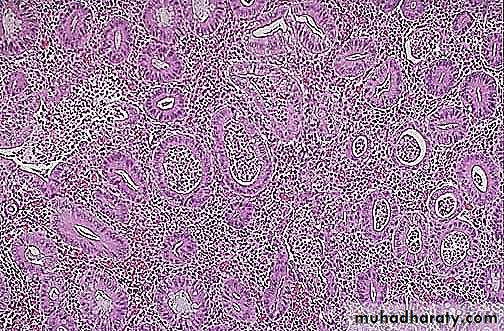
Microscopically, Crohn's disease is characterized by transmural inflammation. Here, inflammatory cells (the bluish infiltrates) extend from mucosa through submucosa and muscularis and appear as nodular infiltrates on the serosal surface with pale granulomatous centers.
One complication of Crohn's disease is fistula formation. Seen here is a fissure extending through mucosa at the left into the submucosa toward the muscular wall, which eventually will form a fistula. Fistulae can form between loops of bowel, bladder, and skin. With colonic involvement, perirectal fistulae are common.
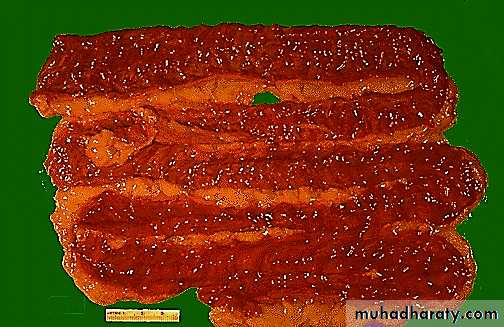
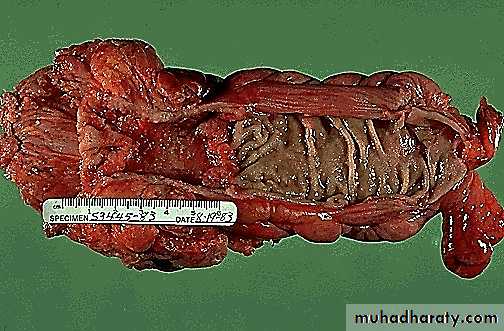
This gross appearance is characteristic for ulcerative colitis. The most intense inflammation begins at the lower right in the sigmoid colon and extends upward and around to the ascending colon. At the lower left is the ileocecal valve with a portion of terminal ileum that is not involved. Inflammation with ulcerative colitis tends to be continuous along the mucosal surface and tends to begin in the rectum. The mucosa becomes eroded, as in this photograph, which shows only remaining islands of mucosa called "pseudopolyps".
At higher magnification, the pseudopolyps can be seen clearly as raised red islands of inflamed mucosa. Between the pseudopolyps is only remaining muscularis.
Microscopically, the inflammation of ulcerative colitis is confined primarily to the mucosa. Here, the mucosa is eroded by an ulcer that undermines surrounding mucosa.
The colonic mucosa of active ulcerative colitis shows "crypt abscesses" in which a neutrophilic exudate is found in glandular lumens. The submucosa shows intense inflammation. The glands demonstrate loss of goblet cells and hyperchromatic nuclei with inflammatory atypia.
Crypt abscesses are a histologic finding more typical with ulcerative colitis. Unfortunately, not all cases of inflammatory bowel disease can be classified completely in all patients.
Over time, there is a risk for adenocarcinoma with ulcerative colitis. Here, more normal glands are seen at the left, but the glands at the right demonstrate dysplasia, the first indication that there is a move towards neoplasia.