LEARNING OBJECTIVES
•To understand:
• •Management of acute pancreatitis
• Assessment and Management of chronic
pancreatitis
• •Diagnosis and treatment of pancreatic
cancer

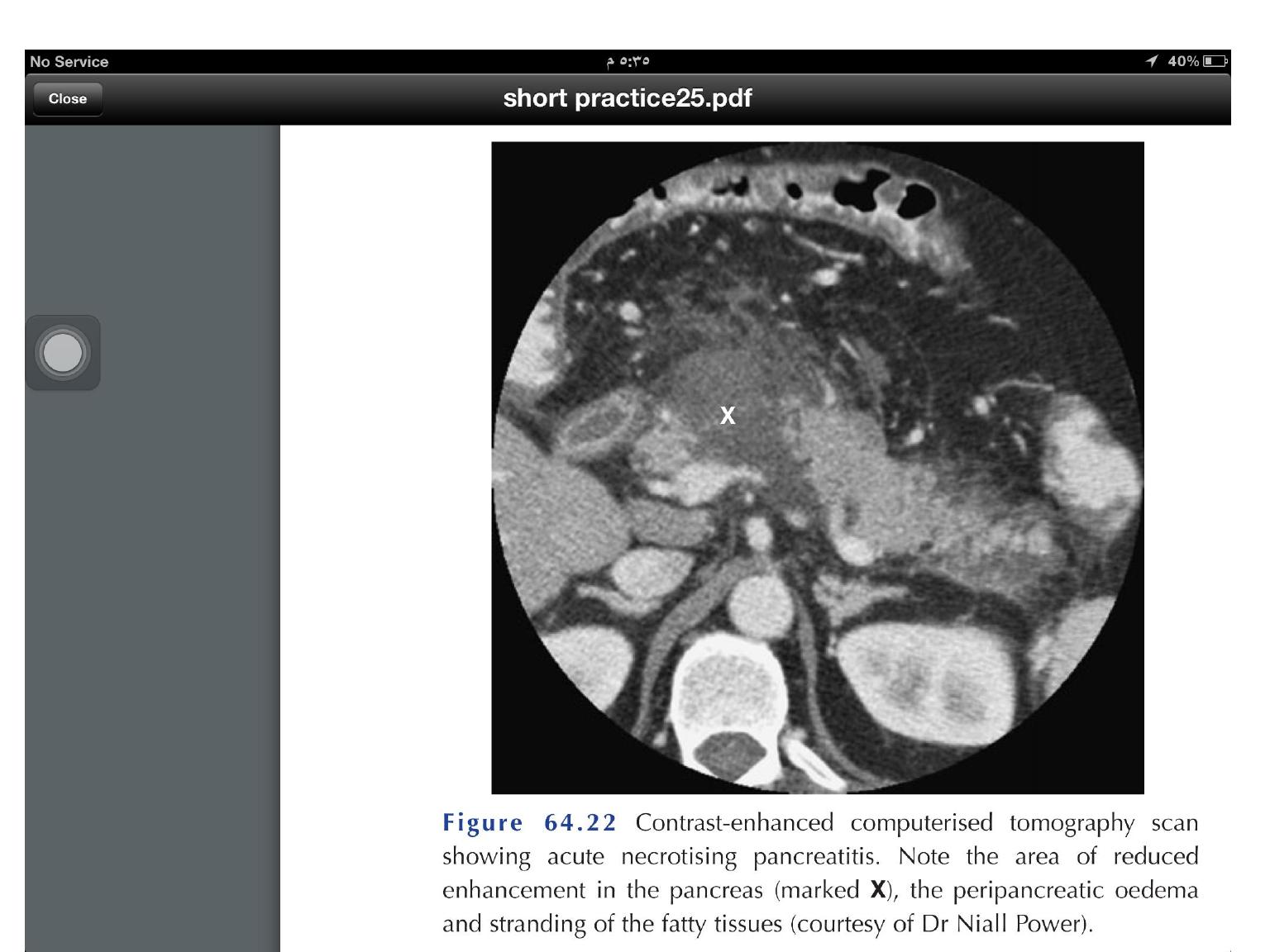
Two out of three of the following criteria must be
met for the diagnosis of acute pancreatitis
:
•Clinical (upper abdominal pain)
•Laboratory (serum amylase or lipase >3 upper limit
of normal
)
Imaging (CT, MR, ultrasound) criteria.
Diagnostic criteria

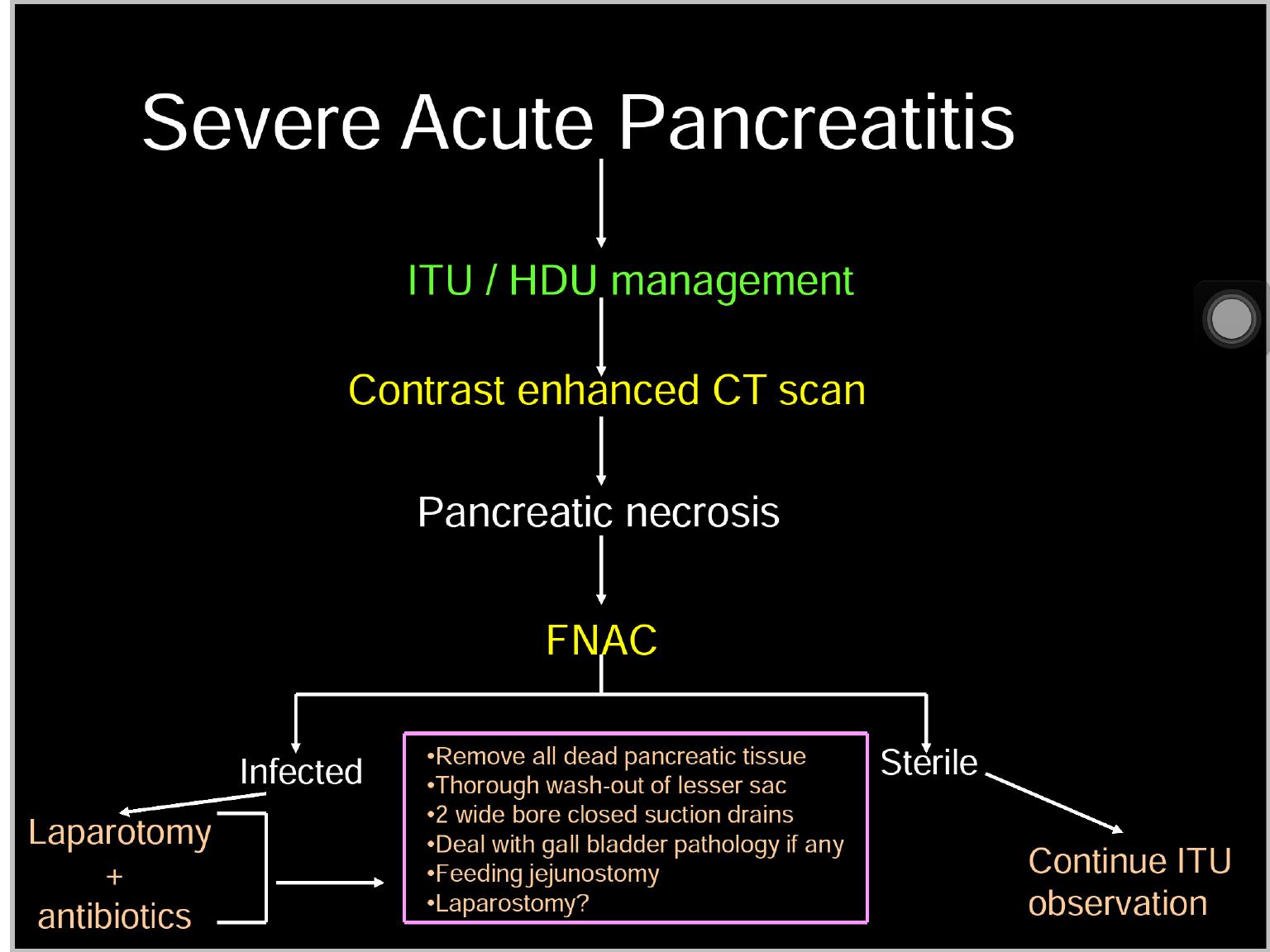
The main goal of initial treatment is to
prevent complications of severe pancreatitis
by reducing pancreatic secretory stimuli and
correction of fluid and electrolyte
abnormalities
.

Resuscitation with intravenous (IV) fluids,
analgesics, and antiemetics are the initial
treatments even before diagnosis is made
.
IV hydration with crystalloids is essential )Ringer’s
lactate solution is recommended), and an effort to
keep urinary output above 30 mL/hour is
necessary to avoid potential kidney damage
.
Aggressive resuscitation (e.g., 1 litre bolus of
crystalloid followed by a continuous infusion rate
of 3 mL/kg/hour) is important within the first 24
hours
.
The patient should be catheterised to
monitor urinary output in severe cases of
acute pancreatitis
.
The most commonly used drugs for pain
control are opioids
.
Fentanyl or morphine can be used, either
for breakthrough pain or as patient-
controlled analgesia (PCA
.)
Ketorolac, a non-steroidal anti-
inflammatory drug (NSAID), can be used in
patients with intact renal
function
.
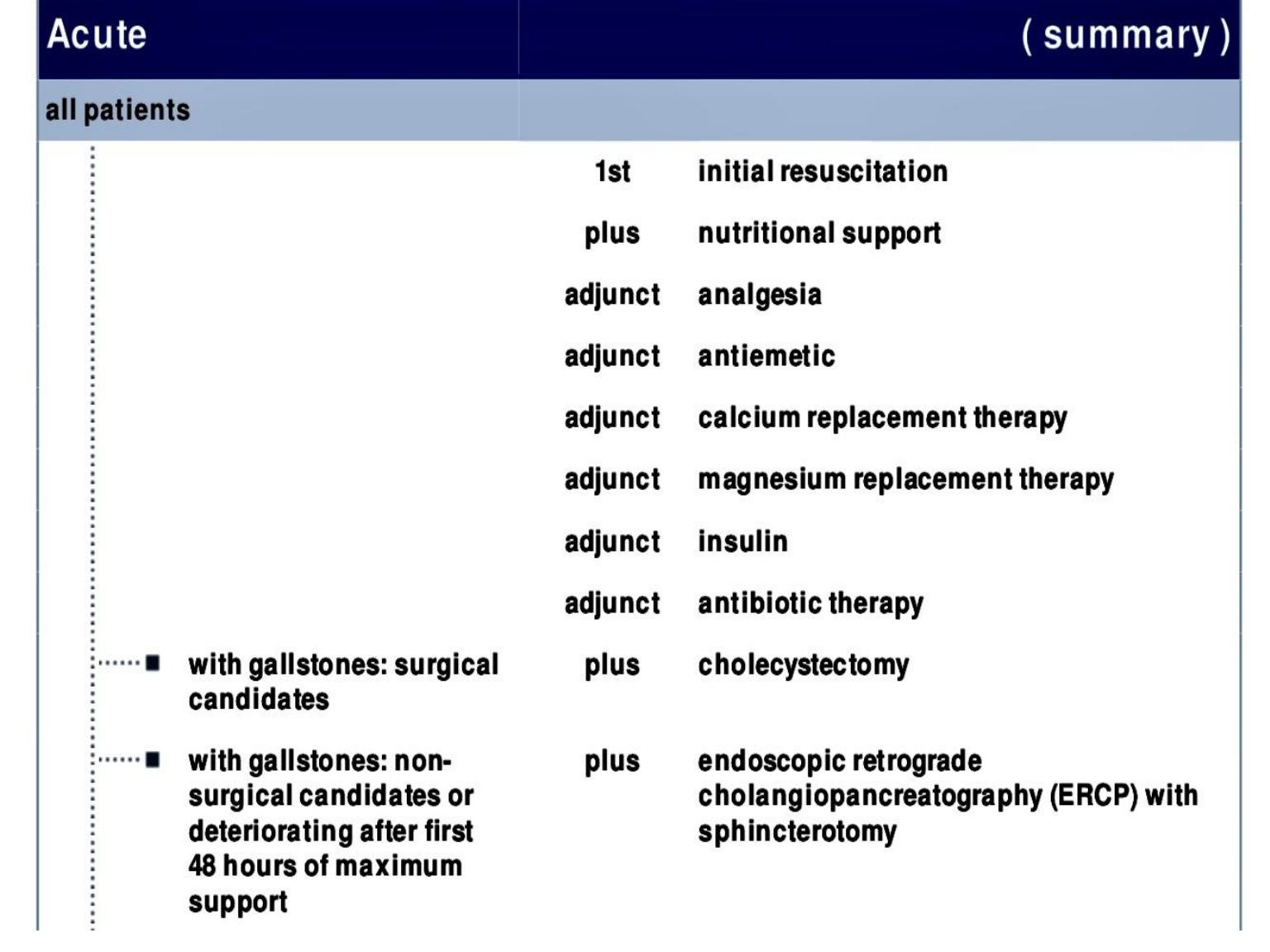

The majority of patients with acute pancreatitis will
improve within 3 to 7 days of conservative
management
.
The cause of pancreatitis should be identified,
and a plan to prevent recurrence should be
initiated before the patient is discharged from
hospital
.
In gallstone pancreatitis, a cholecystectomy
should be performed before discharge in mild
cases and a few months after the discharge date in
patients with severe symptoms
.
In patients who are not candidates for surgery,
endoscopic retrograde cholangiopancreatography
(ERCP) must be considered
.
Pancreatic cancer

•Pancreatic cancer is the fourth highest
cause of cancer death .
•There is no simple screening test;
however, patients with an increased
inherited risk of pancreatic cancer should
be referred to specialist units for screening
and counselling.

•Risk factors for the development of
pancreatic cancer
.
•Demographic factors
•Age (peak incidence 65–75 years)
•Male gender
•Black ethnicity
•Environment/lifestyle
•Cigarette smoking
•Genetic factors and medical conditions
•Family history

•At the time of presentation,
more than 85 per cent
of
patients with ductal adenocarcinoma are unsuitable for
resection because the disease is too advanced
.
•If imaging shows that the tumour is potentially
resectable, the patient should be considered for
surgical resection, as that offers the only chance of a
cure
.
•Tumours of the ampulla have a good prognosis.

•The standard resection for a tumour of the
pancreatic head or the ampulla is a
pylorus-
preserving pancreatoduodenectomy (PPPD .)
•This involves removal of the duodenum and
the pancreatic head, including the distal part of
the bile duct.
•The original pancreatoduodenectomy as
proposed by Whipple included resection of the
gastric antrum.

•For tumours of the body and tail, distal
pancreatectomy with splenectomy is the standard.
•Total pancreatectomy is warranted only in
situations where one is dealing with a multifocal
tumour.

•The median survival
•of patients with unresectable, locally
advanced, non-metastatic pancreatic cancer
is between six and ten months
• and
•in patients with metastatic disease, it is two
to six months.

