1
L9
DISEASES OF MUSCLE
D. Hazim
Myopathy is a muscle disease unrelated to any disorder of innervation or neuromuscular
junction.
These conditions have widely varying etiologies, including congenital or inherited, idiopathic,
infectious, metabolic, inflammatory, endocrine, and drug-induced or toxic.
Clinical Picture
Proximal, large muscles.
Steadily progressive , s.t. episodic
Symmetric
Preserved tone and tendon reflexes
No sensory\autonomic abnormality
Cardiac failure
Cardiac conduction abnormalities
Respiratory problems (sleep apnea)
Outline of investigations
Creatine phosphokinase (CK)
EMG-NCS
Muscle Biopsy (histo-biochemistry)
ECG
CXR
Underlying cause:
Genetic\metabolic screen and counseling
Inflammatory/Endocrine/Electrolytes etc..
Hereditary myopathies
Muscular dystrophies
Metabolic myopathies
Mitochondrial myopathies
channelopathy
Acquired myopathies
inflammatory myopathies
Endocrinologic
Drugs and toxins
MUSCULAR DYSTROPHIES
This is a group of inherited disorders characterised by progressive degeneration of groups of
muscles, sometimes with involvement of the heart muscle or conducting tissue, and other parts
of the nervous system
2
Myotonic dystrophy (DM1).
Duchenne.
Becker.
Facioscapulohumeral (FSH).
Oculopharyngeal.
Emery-Dreifuss.
Clinical features
Onset is often in childhood, although some patients, especially those with myotonic
dystrophy, may present as adults.
Wasting and weakness are usually symmetrical,
no fasciculation ,
no sensory loss,
tendon reflexes are preserved until a late stage, except in myotonic dystrophy.
Differential diagnosis is based on the age at onset, the distribution of affected muscles and the
pattern of inheritance.
Many dystrophies include cardiomyopathy
Investigations
The diagnosis can be confirmed by specific molecular genetic testing, supplemented
with EMG and muscle biopsy if necessary.
Creatine kinase is markedly elevated in Duchenne muscular dystrophy, but is normal
or only moderately elevated in the other dystrophies.
Screening for an associated cardiac abnormality (cardiomyopathy or dysrhythmia) is
important.
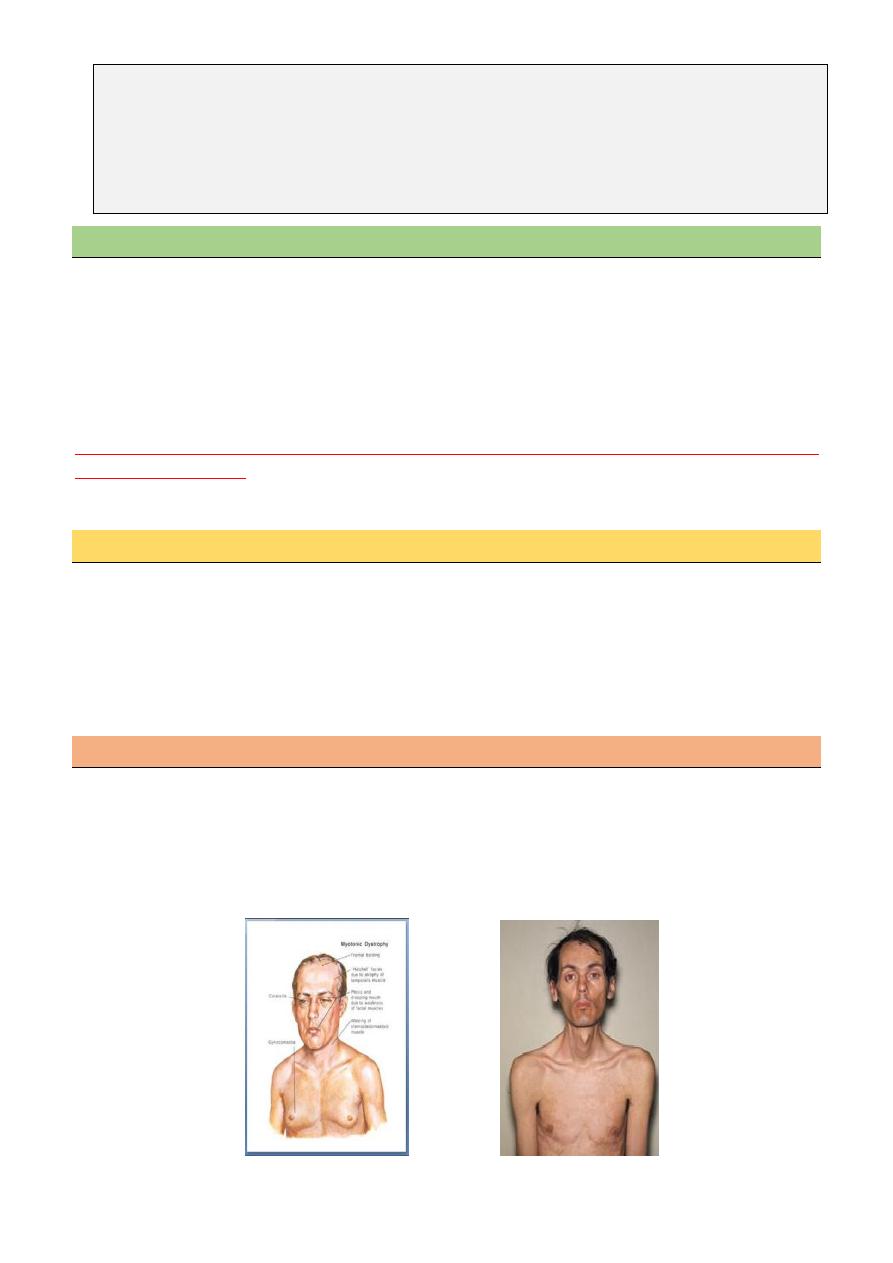
Myotonic dystrophy (DM1)
Autosomal dominant.
Affect any age.
Face (incl. ptosis), sternomastoids, distal limb, generalized later.
Myotonic, cognitive dulling, cardiac conduction abnormalities, lens opacities, frontal
balding, hypogonadism.
3
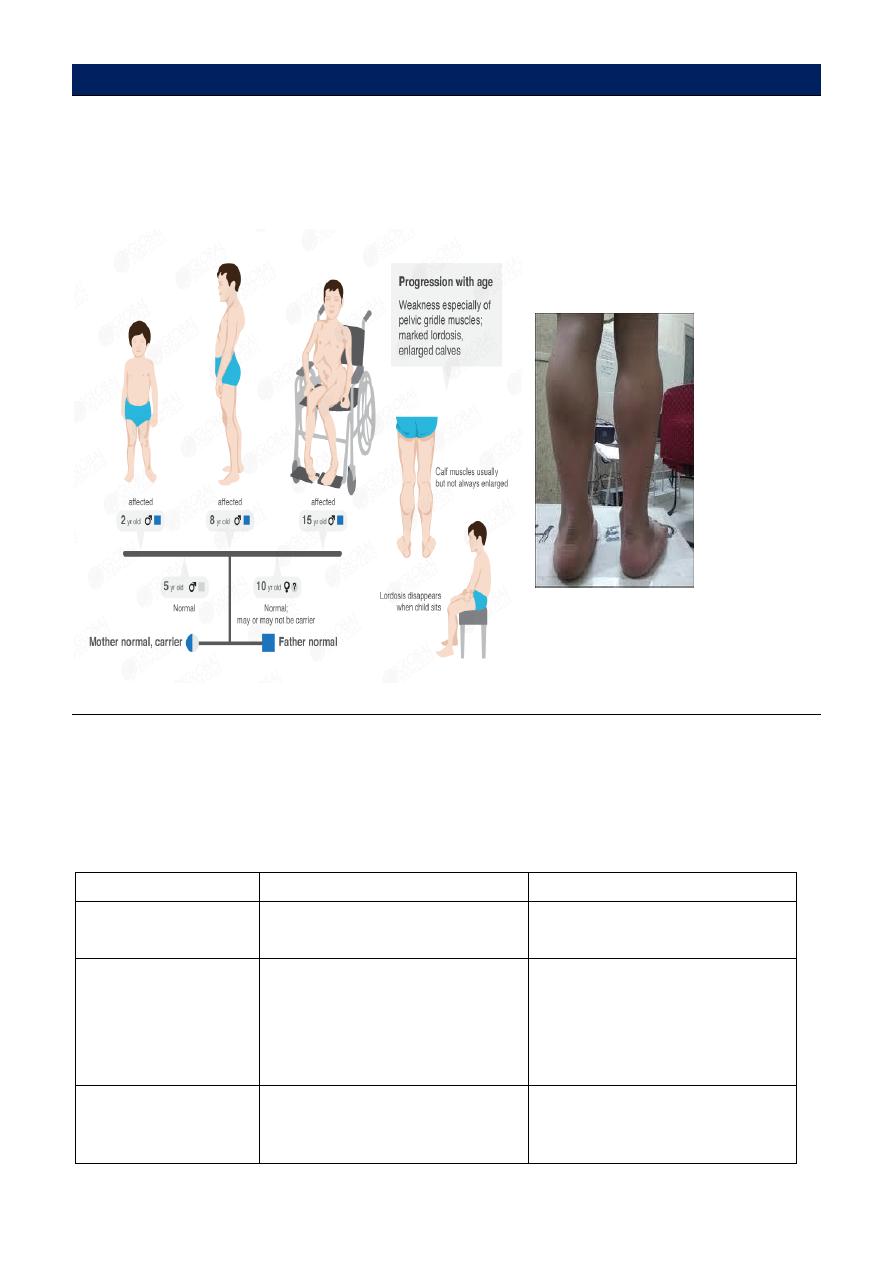
Duchenne
X-linked; deletions in dystrophin gene.
First 5 years.
Proximal and limb girdle.
Pseudohypertrophy of calves.
Cardiomyopathy.
Other variants of dystrophinopathy
Becker muscular dystrophy:
Is a mild form of dystrophinopathy, Patient may live many decades with mild to
moderate symptoms.
Onset usually is after 12 years of age.
Progressive weakness of girdle muscles
type
Duchenne
Becker
Onset
Before 5 years
Early childhood to adult
Clinical Features
Progressive weakness of girdle
muscles
Unable to walk after age 12
Progressive weakness of girdle
muscles
Able to walk after age 15
Mental impairment
Common
Uncommon
4
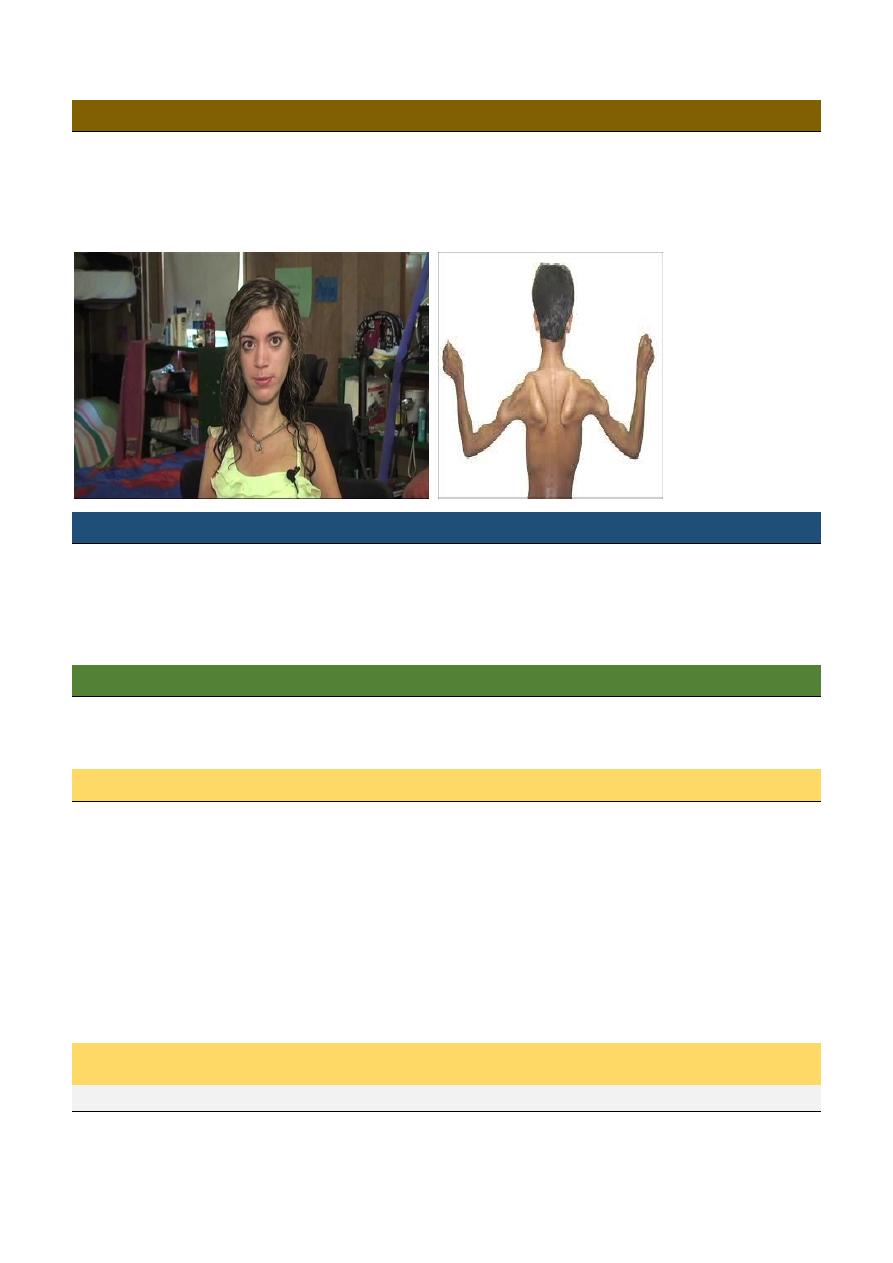
Facioscapulohumeral (FSH)
Autosomal dominant.
7-30 years.
Face and upper limb girdle.
Winging of scapula.
Emery-Dreifuss
4-5 years
Humero- peronal, proximal limb girdle later
Contractures develop early.
Cardiac involvement leads to sudden death
CHANNELOPATHIES
Inherited abnormalities of the sodium, calcium and chloride ion channels in striated muscle
produce various syndromes of familial periodic paralysis, Myotonia and malignant hyperthermia
Hypokalemic periodic paralysis
A muscle
calcium
or sodium channel disorder
autosomal dominant
Attacks are precipitated by a period of exercise followed by rest or by carbohydrate
loading. Attacks typically develop in the early hours of the morning and may last
hours to days.
Serum potassium is typically low at the onset but may normalize quickly.
Patients with hypokalemic paralysis will notice improvement with potassium
ingestion but worsening with glucose.
Thyroid disorder mainly hyperthyroidism can associated with the disease.
Hyperkalemic periodic paralysis
Sodium channel
In hyperkalemic periodic paralysis, (hyperPP) patients typically experience recurrent attacks
of muscle weakness
5
Precipitants include rest following exercise, cold, potassium ingestion or stress.
Attacks may vary in severity from mild weakness to total paralysis, The duration of
attacks is usually less than 2 hours.
Many attacks are brief and do not require treatment.
If necessary, acute attacks can be terminated by ingestion of carbohydrate or inhaled
salbutamol.
Preventative treatment with acetazolamide or a thiazide diuretic may be required.
Drug induced myopathy
Corticosteroids
Chloroquine
Amiodarone
β-blockers
Statins
Vincristine
Zidovudine
Opiates
Mubark A. Wilkins
