1
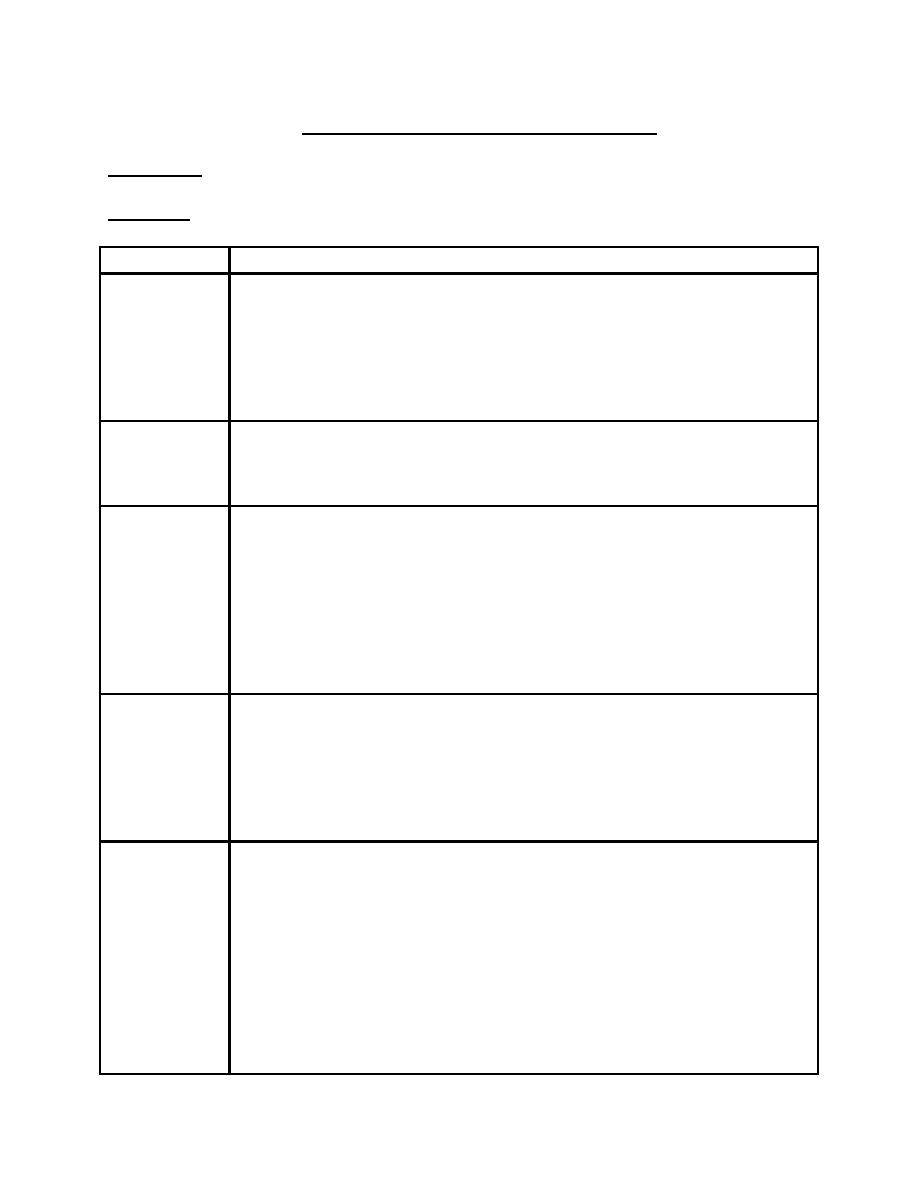
L5. Congestive Heart Failure (CHF)
Definition: Is inability of the heart to deliver adequate cardiac output to meet the body
metabolic needs.
Causes:
Age group
Causes
Fetus
1. Severe anemia e.g. hemolysis (severe Rh incompatibility), fetal-
maternal transfusion, hypoblastic anemia or parvovirus B19
infection.
2. Supraventricular or ventricular tachycardia.
3. Complete heart block as in maternal SLE.
4. Arteriovenous (A-V) malformations.
5. Myocarditis.
Premature
neonate
1. Fluid overload.
2. PDA
3. VSD
4. Bronchopulmonary dysplasia causing cor pulmonale.
Full term
neonate
1. Asphyxial cardiomyopathy.
2. A-V malformation.
3. Lt sided obstructive heart lesions e.g. coarctation of aorta, or
severe aortic stenosis.
4. Transposition of Great Arteries (TGA).
5. Severe anemia.
6. Supraventricular tachycardia.
7. Complete heart block.
8. Myocarditis.
Infant-Toddler
1. VSD (Lt-to-Rt shunt).
2. A-V malformation.
3. Metabolic or genetic cardiomyopathy.
4. Acute hypertension (hemolytic uremic syndrome).
5. Supraventricular tachycardia (SVT).
6. Kwasaki disease.
7. Myocarditis.
Child-
adolescent
1. Rheumatic fever.
2. Acute hypertension (glomerulonephritis)
3. Viral myocarditis.
4. Thyrotoxicosis.
5. Hemochromatosis.
6. Cancer therapy (radiation, doxorubicin)
7. Sickle cell anemia.
8. Endocarditis.
9. Arrhythmias.
10. Cor pulmonale e.g. cystic fibrosis and chronic air way obstruction
11. Cardiomyopathy.
2
Clinical features:
Infant: poor feeding, failure to thrive (FTT), tachypnea, tachycardia, diaphoresis
(sweating) with feeding and hepatomegaly.
Older children:
Symptoms: dyspnea, easy fatigability, and edema.
Clinical signs: tachycardia, gallop rhythm, weak pulse.
If the Lt-sided heart failure is predominant, there is tachypnea, orthopnea, wheezing and
pulmonary edema.
If the Rt-sided heart failure is predominant, there is hepatomegaly, edema and
distended neck veins.
Investigations:
1. CXR: is not specific but absence of cardiomegaly usually rules out diagnosis of CHF.
2. ECG: is not specific but it useful for assessment of heart chambers (Lt, Rt, or
biventricular hypertrophy) and for detection of some underlying causes e.g.
arrhythmias or ischemia.
3. Echocardiography: It diagnostic, it assess the chamber sizes, myocardial function,
and detection of congenital heart diseases if present.
4. Blood gas analysis: shows hypoxia and metabolic or respiratory acidosis in sever
CHF.
5. Serum electrolytes levels especially serum sodium level because infants with CHF
often have hyponatremia due to water retention which decrease more with chronic
diuretic therapy
Treatment:
A. Removal of underlying cause, if possible.
B. General measures:
1. Rest: child allowed for rest during the day time and adequate sleep at night, but
strict bed rest is not necessary.
2. Position: patient sleep in semi-upright position (45 degree).
3. Oxygen supplementation especially in presence of pulmonary edema.
4. Diet: infant with CHF usually have FTT due to increased metabolic demands and
decrease intake, so the caloric intake should increase to 24 calories\oz but not
more because it will cause diarrhea and increase solute load on already
compromised kidneys.
N\G tube may be beneficial in infants or children with poor feeding because of
dyspnea or gastro-esophageal reflux (GER).
Low-sodium formula is not recommended because it poorly tolerated and may
exacerbate diuretic-induced hyponatremia. Breast milk is ideal low sodium diet.
C. Preload-reducing agents (diuretics):
They interfere with renal reabsorption of water and sodium, so they reduce the
pulmonary and cardiac fluid overload.
1. Furosemide (Lasix):is the most common diuretic used in pediatrics. It potent
diuretic because it inhibits sodium and chloride reabsorption in distal tubules and
loop of Henle.
3
Dose: Acute treatment 1-2 mg\kg\24hr I.V. until clinical improvement, then
chronic treatment with 1-4mg\kg\day in 1-4 doses orally.
Side effects: hypokalemia, so the patient required oral potassium chloride
supplementation or potassium-sparing agent (spironolactone) with furosemide.
2. Spironolactone (aldactone): it aldosterone inhibitors, it enhance potassium
retention eliminating the need for oral potassium chloride supplementation which
is poorly tolerable.
Dose: 2mg\kg\day orally in 2 divided doses.
3. Chlorothiazide: is less potent than furosemide because it affect electrolyte
reabsorption in the renal tubules only.
Dose: 10-40 mg\kg\day in 2 divided doses.
Potassium chloride or spironolactone is must be administer with chlorothiazide
because of its hypokalemic effect.
D. Afterload reducing agents (angiotensin converting enzyme inhibitors (ACEI)
and angiotensin II receptor blockers:
They decrease ventricular afterload by decreasing peripheral vascular resistance
(arterial dilatation) to improve myocardial performance.
They also decrease systemic venous tone (venodilatation) which significantly
decrease the preload.
They are not used in patients with Lt ventricular out flow obstruction as in aortic
stenosis because it reduce the coronary perfusion. These agents include.
1. Nitroprusside: it should be given by IV infusion in the intensive care units(ICU)
only for critically ill patients and for short time only due to its serious side effects.
Side effects:
1. Sever hypotension due to its arterial and venous dilation effect.
2. Cyanide poisoning, because it metabolized in the body to cyanide which
detoxified in the liver into thiocyanate and excreted in the urine. With large
dose of Nitroprusside, cyanide toxicity will occurs causing fatigue, nausea,
disorientation, acidosis and muscle spasms.
2. ACEI (captopril and enalpril): they have the following effects:
1. Arterial dilation by blocking angiotensin II production, so they are afterload
reducers.
2. Causing venodilatation so they reduce the preload.
3. They have aldosterone inhibitor effect, so the control salt and water retension.
Doses:
Captopril: 0.3-6mg\kg\day in 3 divided doses orally.
Enalpril: 0.05-0.5 mg\kg\day in 1-2 doses orally.
Side effects: hypotension, hyperkalemia, pruritic maculopapular rash,
neutropenia, renal toxicity and chronic cough.
4
E. Digoxin:
Is the mainstay in treatment of CHF, although the combination of diuretics and ACEI
significantly reduce need to digoxin or even is no longer use in some centers.
Dose: 0.01
– 0.04 mg\kg\day according to the patients age.
Rapid digitalization is achieved within 36hr by given half of the total dose (IV)
immediately then 1\4 of the total dose after 12hr and then the last 1\4 after the next
12hr.
Important cautions with digoxin administration:
1. ECG should be done before each of 3 doses of digoxin and digoxin should stop if
new rhythm disturbance developed.
Prolonged P-R interval alone is not an indication for digoxin stopping, but indicate
delay the next dose or decrease the dose according to the patient status.
Minor ST segment or T-wave changes are commonly noted with digoxin
administration and should not affect the digitalization regimen.
2. Close monitoring of serum electrolytes especially in concomitant use of diuretics
because hyperkalemia and hypercalcemia increase digoxin toxicity.
3. Digoxin is better to be avoided in patients with myocarditis if possible or given in half
of the total dose only because it increase the risk of arrhythmias in these patients.
Factors increase digoxin toxicity:
1. Hypokalemia.
2. Hypomagnesemia.
3. Hypercalcemia.
4. Myocarditis.
5. Prematurity.
6. Renal failure.
