
Lec 8 Delayed puberty &infertility Dr. Nihad A. Aljeboori /Subspeciality diabetes &Endocrinoogy
Delayed puberty
Puberty is considered to be delayed if the onset of the physical features of sexual maturation
has not occurred by a chronological age that is 2.5 standard deviations (SD) above the
national average. In the UK, this is by the age of 14 in boys and 13 in girls. Genetic factors
have a major influence in determining the timing of the onset of puberty, such that the age of
menarche (the onset of menstruation) is often comparable within sibling and mother–
daughter pairs and within ethnic groups. However, because there is also a threshold for body
weight that acts as a trigger for normal puberty, the onset of puberty can be influenced by
other factors including nutritional status and chronic illness .
Clinical assessment
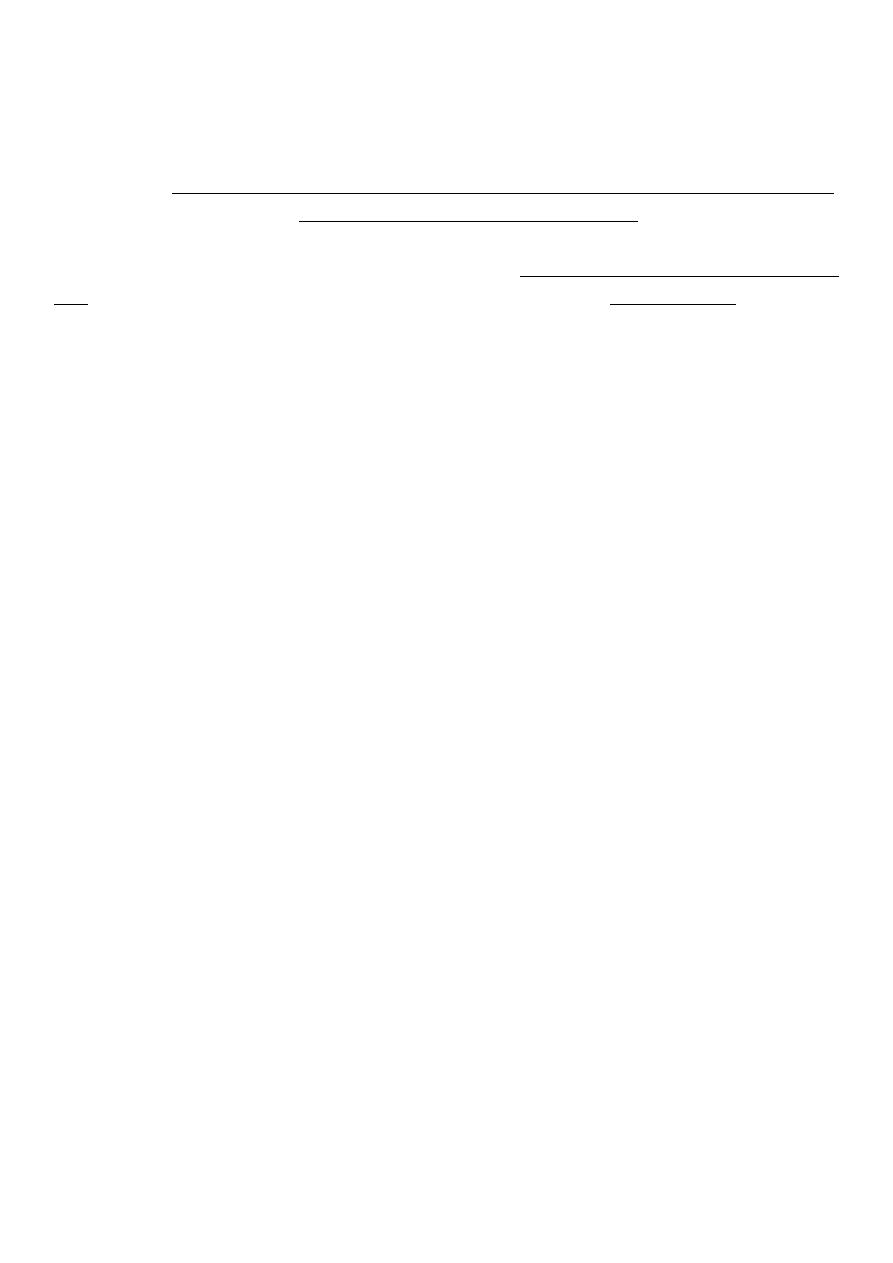
The differential diagnosis is shown in Box 18.20. The key issue is to determine whether the
delay in puberty is simply because the ‘clock is running slow’ (
constitutional delay of
puberty
) or because there is pathology in the hypothalamus/ pituitary (hypogonadotrophic
hypogonadism) or the gonads (hypergonadotrophic hypogonadism). A general history and
physical examination should be performed with particular reference to previous or current
medical disorders, social circumstances and family history. Body proportions, sense of smell
and pubertal stage should be carefully documented and, in boys, the presence or absence of
testes in the scrotum noted. Current weight and height may be plotted on centile charts, along
with parental heights. Previous growth measurements in childhood, which can usually be
obtained from health records, are extremely useful. Healthy growth usually follows a centile.
Usually, children with constitutional delay have always been small but have maintained a
normal growth velocity that is appropriate for bone age. Poor linear growth, with ‘crossing
of the centiles’, is more likely to be associated with acquired disease.
Lec 8 Delayed puberty &infertility Dr. Nihad A. Aljeboori /Subspeciality diabetes &Endocrinoogy
Constitutional delay of puberty
This is the most common cause of delayed puberty, but is a much more frequent explanation
for lack of pubertal development in boys than in girls. Affected children are healthy and have
usually been more than 2 SD below the mean height for their age throughout childhood.
There is often a history of delayed puberty in siblings or parents. Since sex steroids are
essential for fusion of the epiphyses, ‘bone age’ can be estimated by X-rays of epiphyses,
usually in the wrist and hand; in constitutional delay, bone age is lower than chronological
age. Constitutional delay of puberty should be considered as a normal variant, as puberty
will commence spontaneously. However, affected children can experience significant
psychological distress because of their lack of physical development, particularly when
compared with their peers.
Hypogonadotrophic hypogonadism
This may be due to structural, inflammatory or infiltrative disorders of the pituitary and/or
hypothalamus (see Box 18.54, p. 681). In such circumstances, other pituitary hormones, such
as growth hormone, are also likely to be deficient. ‘Functional’ gonadotrophin deficiency is
caused by a variety of factors, including low body weight, chronic systemic illness (as a
consequence of the disease itself or secondary malnutrition), endocrine disorders and
profound psychosocial stress. Isolated gonadotrophin deficiency is usually due to a genetic
abnormality that affects the synthesis of either GnRH or gonadotrophins. The most common
form is Kallmann’s syndrome, in which there is primary GnRH deficiency and, in most
affected individuals, agenesis or hypoplasia of the olfactory bulbs, resulting in anosmia or
hyposmia. If isolated gonadotrophin deficiency is left untreated, the epiphyses fail to fuse,
resulting in tall stature with disproportionately long arms and legs relative to trunk height
(eunuchoid habitus). Cryptorchidism (undescended testes) and gynaecomastia are commonly
observed in all forms of hypogonadotrophic hypogonadism.
Male hypogonadism
The clinical features of both hypo- and hypergonadotrophic hypogonadism include loss of
libido, lethargy with muscle weakness, and decreased frequency of shaving. Patients may
also present with gynaecomastia, infertility, delayed puberty, osteoporosis or anaemia of
chronic disease.
Mild hypogonadism may also occur in older men, particularly in the context of central
adiposity and the metabolic syndrome. Postulated mechanisms are complex and include
reduction in sex hormone binding globulin by insulin resistance and reduction in GnRH and
gonadotrophin secretion by cytokines or oestrogen released by adipose tissue. Testosterone
levels also fall gradually with age in men and this is associated with gonadotrophin levels
that are low or inappropriately within the ‘normal’ range. There is an increasing trend to
Lec 8 Delayed puberty &infertility Dr. Nihad A. Aljeboori /Subspeciality diabetes &Endocrinoogy
measure testosterone in older men, typically as part of an assessment of erectile dysfunction
and lack of libido.
Investigations
Male hypogonadism is confirmed by demonstrating a low fasting 0900-hr serum
testosterone level. The distinction between hypo- and hypergonadotrophic hypogonadism is
by measurement of random LH and FSH. Patients with hypogonadotrophic hypogonadism
should be investigated as described for pituitary disease on page 680. Patients with
hypergonadotrophic hypogonadism should have the testes examined for cryptorchidism or
atrophy, and a karyotype should be performed (to identify Klinefelter’s syndrome).
Management
Testosterone replacement is clearly indicated in younger men with significant hypogonadism
to prevent osteoporosis and to restore muscle power and libido. Debate exists as to whether
replacement therapy is of benefit in mild hypogonadism associated with ageing and central
adiposity, particularly in the absence of structural pituitary/hypothalamic disease or other
pituitary hormone deficiency. In such instances, a therapeutic trial of testosterone therapy
may be considered if symptoms are present (e.g. low libido and erectile dysfunction), but the
benefits of therapy must be carefully weighed against the potential for harm. First-pass
hepatic metabolism of testosterone is highly efficient, so bioavailability of ingested
preparations is poor. Doses of systemic testosterone can be titrated against symptoms;
circulating testosterone levels may provide only a rough guide to dosage because they may

Lec 8 Delayed puberty &infertility Dr. Nihad A. Aljeboori /Subspeciality diabetes &Endocrinoogy
be highly variable . Testosterone therapy can aggravate prostatic carcinoma; prostate-specific
antigen (PSA) should be measured before commencing testosterone therapy in men older
than 50 years and monitored annually thereafter. Haemoglobin concentration should also be
monitored in older men, as androgen replacement can cause polycythaemia. Testosterone
replacement inhibits spermatogenesis; treatment for fertility is described below.
Infertility
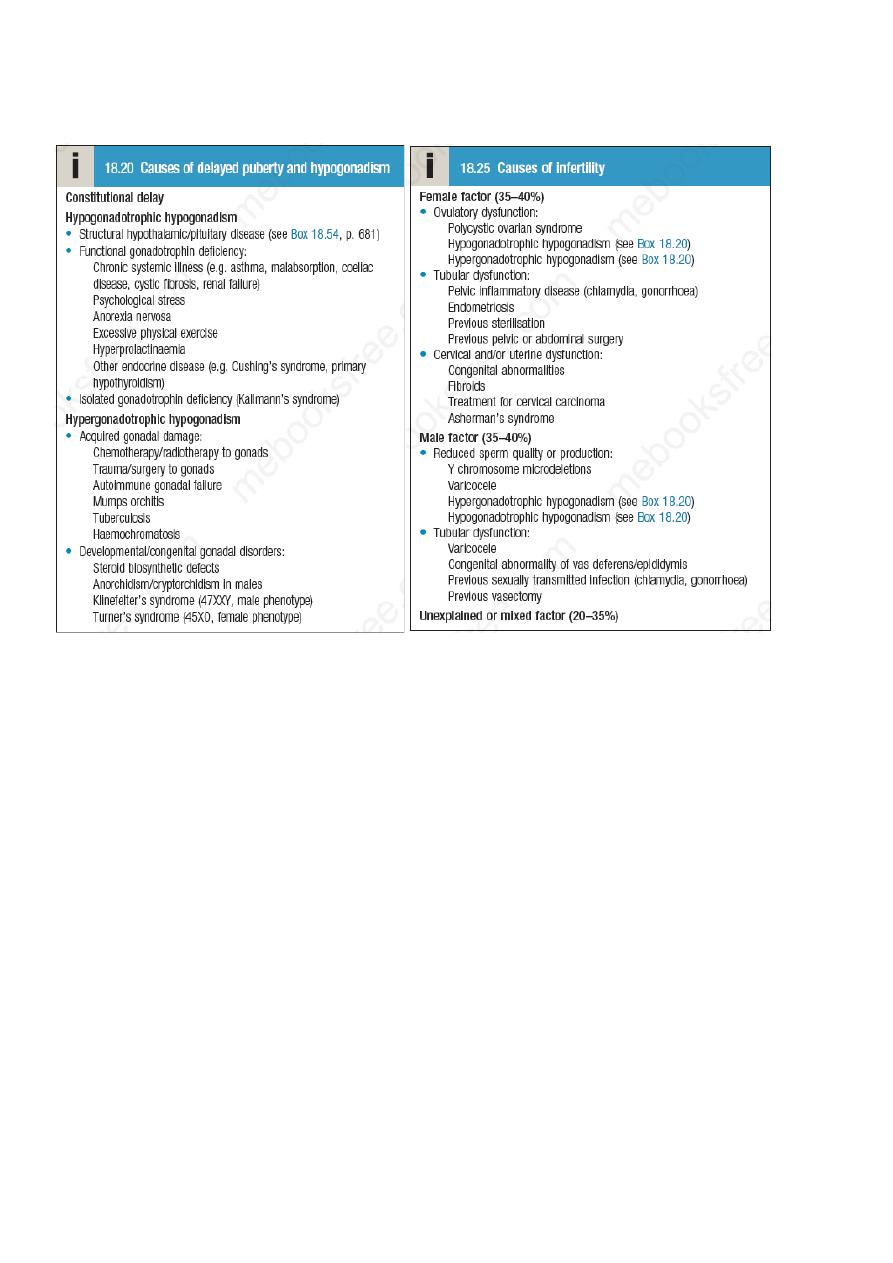
Infertility affects around 1 in 7 couples of reproductive age, often causing psychological
distress. The main causes are listed in Box 18.25. In women, it may result from anovulation
or abnormalities of the reproductive tract that prevent fertilisation or embryonic
implantation, often damaged Fallopian tubes from previous infection. In men, infertility may
result from impaired sperm quality (e.g. reduced motility) or reduced sperm number.
Azoospermia or oligospermia is usually idiopathic but may be a consequence of
hypogonadism. Microdeletions of the Y chromosome are increasingly recognised as a cause
of severely abnormal spermatogenesis. In many couples, more than one factor causing
subfertility is present, and in a large proportion no cause can be identified .
Clinical assessment
A history of previous pregnancies, relevant infections and surgery is important in both men
and women. A sexual history must be explored sensitively, as some couples have intercourse
infrequently or only when they consider the woman to be ovulating, and psychosexual
difficulties are common. Irregular and/or infrequent menstrual periods are an indicator of
anovulatory cycles in the woman, in which case causes such as PCOS should be considered.
In men, the testes should be examined to confirm that both are in the scrotum and to identify
any structural abnormality, such as small size, absent vas deferens or the presence of a
varicocele.
Investigations
Investigations should generally be performed after a couple has failed to conceive despite
unprotected intercourse for 12 months, unless there is an obvious abnormality like
amenorrhoea. Both partners need to be investigated. The male partner needs a semen
analysis to assess sperm count and quality. Home testing for ovulation (by commercial urine
dipstick kits, temperature measurement, or assessment of cervical mucus) is not
recommended, as the information is often counterbalanced by increased anxiety if
interpretation is inconclusive. In women with regular periods, ovulation can be confirmed by
an elevated serum progesterone concentration on day 21 of the menstrual cycle. Transvaginal
ultrasound can be used to assess uterine and ovarian anatomy. Tubal patency may be
examined at laparoscopy or by hysterosalpingography (HSG; a radio-opaque medium is
injected into the uterus and should normally outline the Fallopian tubes). In vitro

Lec 8 Delayed puberty &infertility Dr. Nihad A. Aljeboori /Subspeciality diabetes &Endocrinoogy
assessments of sperm survival in cervical mucus may be done in cases of unexplained
infertility but are rarely helpful.
Management
Couples should be advised to have regular sexual intercourse, ideally every 2–3 days
throughout the menstrual cycle. It is not uncommon for ‘spontaneous’ pregnancies to occur
in couples undergoing investigations for infertility or with identified causes of male or
female subfertility. In women with anovulatory cycles secondary to PCOS , clomifene,
which has partial anti-oestrogen action, blocks negative feedback of oestrogen on the
hypothalamus/pituitary, causing gonadotrophin secretion and thus ovulation. In women with
gonadotrophin deficiency or in whom anti-oestrogen therapy is unsuccessful, ovulation may
be induced by direct stimulation of the ovary by daily injection of FSH and an injection of
hCG to induce follicular rupture at the appropriate time. In hypothalamic disease, pulsatile
GnRH therapy with a portable infusion pump can be used to stimulate pituitary
gonadotrophin secretion (note that non-pulsatile administration of GnRH or its analogues
paradoxically suppresses LH and FSH secretion). Whatever method of ovulation induction is
employed, monitoring of response is essential to avoid multiple ovulation. For clomifene,
ultrasound monitoring is recommended for at least the first cycle. During gonadotrophin
therapy, closer monitoring of follicular growth by transvaginal ultrasonography and blood
oestradiol levels is mandatory. ‘Ovarian hyperstimulation syndrome’ is characterised by
grossly enlarged ovaries and capillary leak with circulatory shock, pleural effusions and
ascites. Anovulatory women who fail to respond to ovulation induction or who have primary
ovarian failure may wish to consider using donated eggs or embryos, surrogacy and
adoption. Surgery to restore Fallopian tube patency can be effective but in vitro fertilisation
(IVF) is normally recommended. IVF is widely used for many causes of infertility and in
unexplained cases of prolonged (> 3 years) infertility. The success of IVF depends on age,
with low success rates in women over 40 years. Men with hypogonadotrophic hypogonadism
who wish fertility are usually given injections of hCG several times a week (recombinant
FSH may also be required in men with hypogonadism of pre-pubertal origin); it may take up
to 2 years to achieve satisfactory sperm counts. Surgery is rarely an option in primary
testicular disease but removal of a varicocele can improve semen quality. Extraction of
sperm from the epididymis for IVF, and intracytoplasmic sperm injection (ICSI, when single
spermatozoa are injected into each oöcyte) are being used increasingly in men with
oligospermia or poor sperm quality who have primary testicular disease. Azoospermic men
may opt to use donated sperm but this may be in short supply
