
Female reproductive system
Normal menstrual cycle:
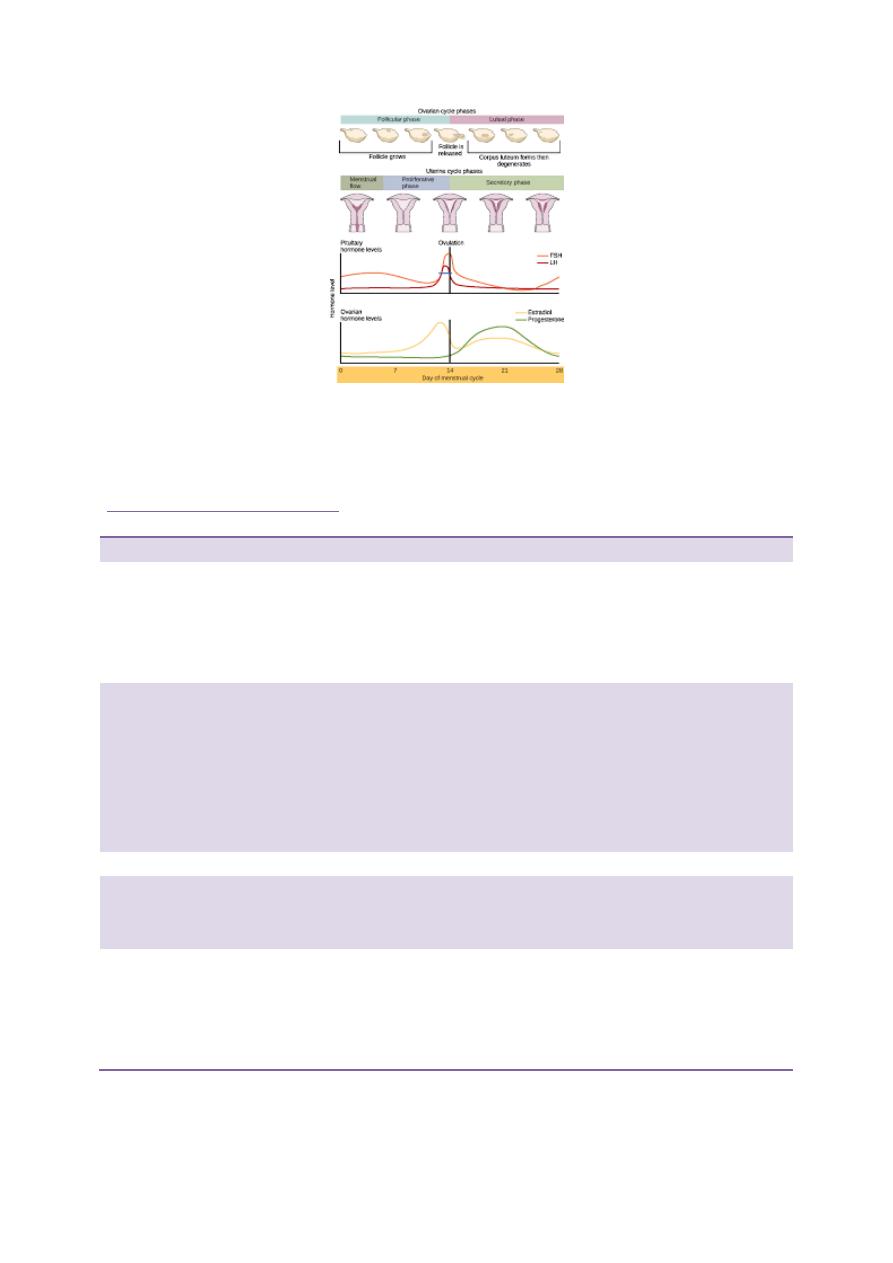
In the female, physiology varies during the normal menstrual cycle. FSH
stimulates growth and development of ovarian follicles during the first 14 days
after the menses. This leads to a gradual increase in oestradiol production from
granulosa cells, which initially suppresses FSH secretion (negative feedback)
but then, above a certain level, stimulates an increase in both the frequency and
amplitude of gonadotrophin-releasing hormone (GnRH) pulses, resulting in a
marked increase in LH secretion (positive feedback). The mid-cycle ‘surge’ of
LH induces ovulation. After release of the ovum, the follicle differentiates into a
corpus luteum, which secretes progesterone. Unless pregnancy occurs during
the cycle, the corpus luteum regresses and the fall in progesterone levels results
in menstrual bleeding. Circulating levels of oestrogen and progesterone in pre-
menopausal women are, therefore, critically dependent on the time of the cycle.
The most useful ‘test’ of ovarian function is a careful menstrual history: if
menses are regular, measurement of gonadotrophins and oestrogen is not
necessary. In addition, ovulation can be confirmed by measuring plasma
progesterone levels during the luteal phase (‘day 21 progesterone’)
Cessation of menstruation (the menopause) occurs at an average age of
approximately 50 years in developed countries. In the 5 years before, there is a
gradual increase in the number of anovulatory cycles and this is referred to as
the climacteric. Oestrogen and inhibin secretion falls and negative feedback
results in increased pituitary secretion of LH and FSH (both typically to levels
above 30 IU/L (3.3 μg/L)). See the following figure
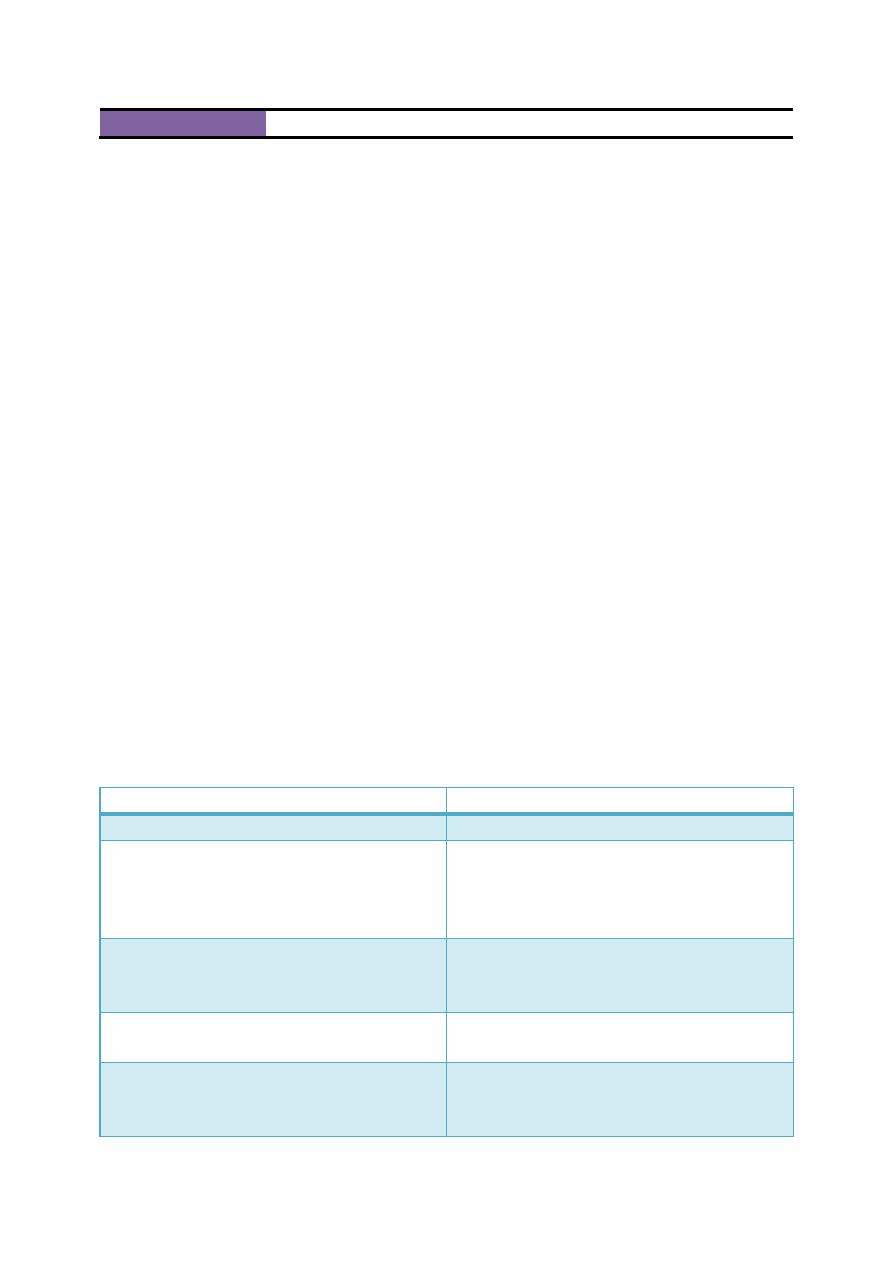
Classification of reproductive system diseases
Primary
Secondary
Hormone excess
Polycystic ovarian
syndrome
Granulosa cell tumour
Leydig cell tumour
Teratoma
Pituitary
gonadotrophinoma
Hormone deficiency
Menopause
Hypogonadism
Turner’s syndrome
Klinefelter’s syndrome
Hypopituitarism
Kallmann’s syndrome
(isolated GnRH
deficiency)
Severe systemic illness,
including anorexia
nervosa
Hormone hypersensitivity Idiopathic hirsutism
Hormone resistance
Androgen resistance syndromes Complete (‘testicular feminisation’) Partial
(Reifenstein’s syndrome) 5α-reductase type 2 deficiency
Non-functioning tumours
Ovarian cysts
Carcinoma
Teratoma
Seminoma

Delayed puberty:
Puberty is considered to be delayed if the onset of the physical features of
sexual maturation has not occurred by a chronological age that is 2.5 standard
deviations (SD) above the national average. In the UK, this is by the age of 14
in boys and 13 in girls. Genetic factors have a major influence in determining
the timing of the onset of puberty, such that the age of menarche (the onset of
menstruation) is often comparable within sibling and mother–daughter pairs and
within ethnic groups. However, because there is also a threshold for body
weight that acts as a trigger for normal puberty, the onset of puberty can be
influenced by other factors including nutritional status and chronic illness.
Causes:
1. Constitutional delay
2. Hypogonadotrophic hypogonadism
A/Structural hypothalamic/pituitary disease
B/Functional gonadotrophin deficiency:
Chronic systemic illness (e.g. asthma, malabsorption, coeliac disease, cystic
fibrosis, renal failure)
Psychological stress
Anorexia nervosa
Excessive physical exercise
Hyperprolactinaemia
Other endocrine disease (e.g. Cushing’s syndrome, primary hypothyroidism)
C/Isolated gonadotrophin deficiency (Kallmann’s syndrome)
3. Hypergonadotrophic hypogonadism
• Acquired gonadal damage: Chemotherapy/radiotherapy to gonads
Trauma/surgery to gonads
Autoimmune gonadal failure

Mumps orchitis
Tuberculosis
Haemochromatosis
4. Developmental/congenital gonadal disorders:
Steroid biosynthetic defects
Anorchidism/cryptorchidism in males
Klinefelter’s syndrome (47XXY, male phenotype)
Turner’s syndrome (45XO, female phenotype)
Investigations
Key measurements are LH and FSH, oestradiol (in girls).
Chromosome analysis should be performed if gonadotrophin concentrations are
elevated.
If gonadotrophin concentrations are low, then the differential diagnosis lies
between constitutional delay and hypogonadotrophic hypogonadism.
A plain X-ray of the wrist and hand may be compared with a set of standard
films to obtain a bone age.
Full blood count, renal function, liver function, thyroid function and coeliac
disease autoantibodies should be measured, but further tests may be
unnecessary if the blood tests are normal and the child has all the clinical
features of constitutional delay.
If hypogonadotrophic hypogonadism is suspected, neuroimaging and further
investigations are required.
Management
Puberty can be induced using low doses of oral oestrogen in girls (e.g.
ethinylestradiol 2 μg daily)
Hirsutism:
refers to the excessive growth of terminal hair (the thick,
pigmented hair usually associated with the adult male chest) in an androgen-
dependent distribution in women (upper lip, chin, chest, back, lower abdomen,
thigh, forearm) and is one of the most common presentations of endocrine
disease. It should be distinguished from hypertrichosis, which is generalised
excessive growth of vellus hair (the thin, non-pigmented hair that is typically
found all over the body from childhood onwards).
Approach to patients with hirsuitism
Causes
Clinical features
Ix
Rx
Idiopathic
Often familial
Mediterranean or
Asian background
Normal
Cosmetic
Antiandrogens
PCOS
Obesity
Oligomenorrhoea
or secondary
amenorrhoea
Infertility
LH:FSH ratio >
2.5:1
Minor elevation of
androgens
Mild
hyperprolactinaemia
Wt loss
Cosmetic
measures
Anti-androgens
(Metformin,
glitazones may
be useful
Congenital
adrenal
hyperplasia
(95% 21-
hydroxylase
deficiency
Pigmentation
History of salt-
wasting in
childhood,
ambiguous
genitalia, or
adrenal crisis
when stressed
Jewish
background
Elevated
androgens* that
suppress with
dexamethasone
Abnormal rise in
17-OH-
progesterone with
ACTH
Glucocorticoid
replacement
Exogenous
androgen
administration
Athletes
Virilisation
Low LH and FSH
Analysis of urinary
androgens may
detect drug of
misuse
Stop misuse
Androgen-
secreting
tumour of ovary
or adrenal
cortex
Rapid onset
Virilisation:
clitoromegaly,
deep voice,
balding, breast
atrophy
high androgens*
that do not suppress
with dexamethasone
Low LH and FSH
CT or MRI usually
demonstrates a
tumour
Sx
Cushing’s
S&S of Cushing’s Ix of Cushin’s
Rx of Cushing’s
syndrome
Polycystic ovarian syndrome
Polycystic ovarian syndrome (PCOS) affects up to 10% of women of
reproductive age. It is a heterogeneous disorder often associated with obesity,
for which the primary cause remains uncertain. Genetic factors probably play a
role, since PCOS often affects several family members. The severity and
clinical features of PCOS vary markedly between individual patients but
diagnosis is usually made during the investigation of hirsutism or
amenorrhoea/oligomenorrhoea . Infertility may also be present There is no
universally accepted definition but it has been recommended that a diagnosis of
PCOS requires the presence of two of the following three features:
• Menstrual irregularity
• Clinical or biochemical androgen excess
• Multiple cysts in the ovaries (most readily detected by transvaginal
ultrasound)
Women with PCOS are at increased risk of glucose intolerance and some
authorities recommend screening for type 2 diabetes and other cardiovascular
risk factors associated with the metabolic syndrome.
Mechanisms*
Manifestations
Pituitary dysfunction
High serum LH High serum prolactin
Anovulatory menstrual cycles
Oligomenorrhoea
Secondary amenorrhoea
Cystic ovaries
Infertility
Androgen excess
Hirsutism
Acne
Obesity
Hyperglycaemia
Elevated oestrogens
Insulin resistance
Dyslipidaemia
Hypertension

Management
1. Wt loss
2. Metformin
3. Antiandrogens
4. Estrogen
5. Local measures
