1
أ.د حسن سالم الجميلي باطن
يه الكورس الثاني
lec3
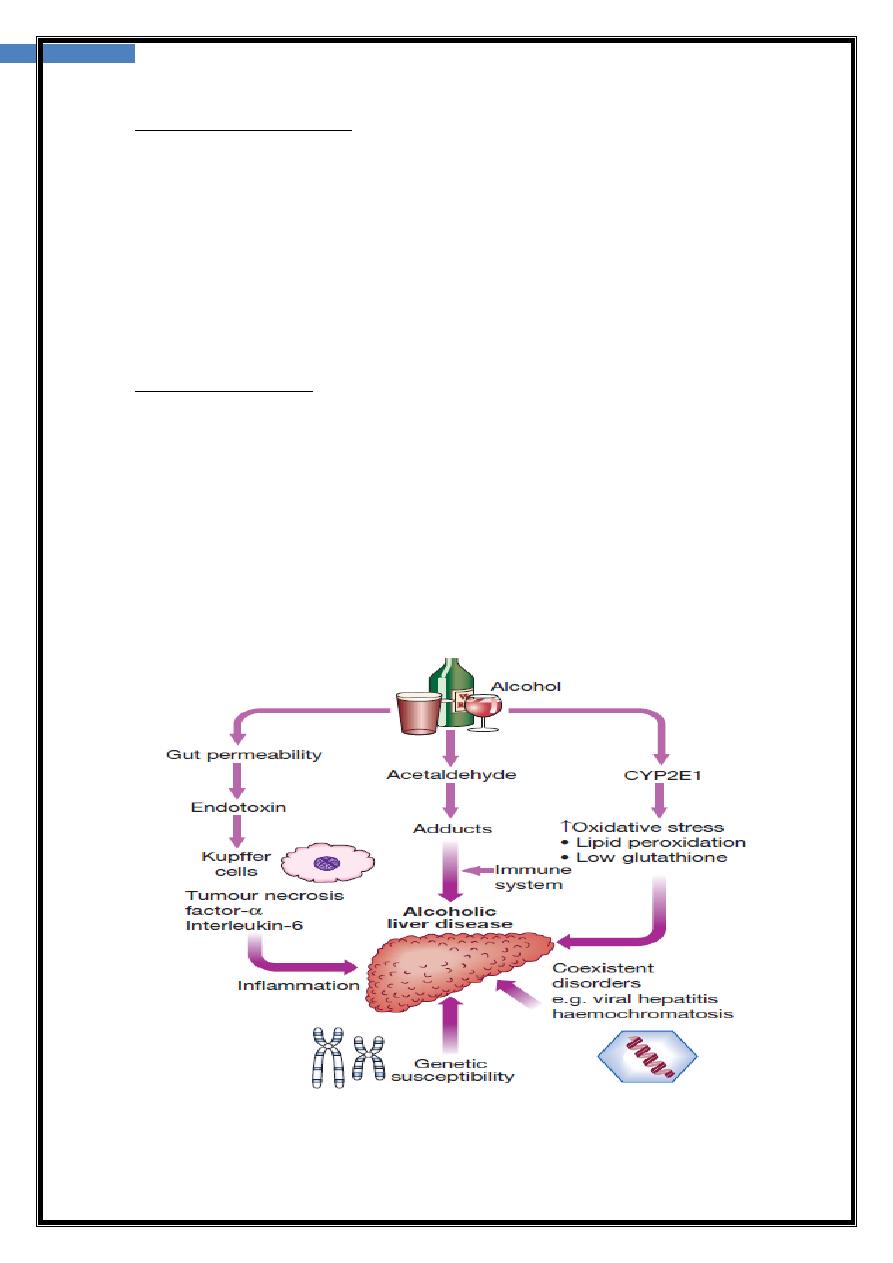
Alcohol liver disease
-most common causes of CLD worldwide
-unit of alcohol contains 8 g of ethanol.
-14 units/week in women and 21 units/week in men →safe.
-The risk threshold for developing ALD is variable but begins at 30 g/day of
ethanol. (3.75 unit)
-consumption of more than 80 g/day> 5 years →significant risk of advanced liver
disease.
-The average alcohol consumption of a man with cirrhosis is 160 g/day for over 8
years
:
risk factors for ALD are
•Drinking pattern.. Liver damage is more likely to occur in continuous rather than
intermittent The type of beverage does not affect risk.
•Gender. increasing in women, his may be related to the
reduced volume of distribution of alcohol.
•Genetics. Alcoholism is more concordant in monozygotic than dizygotic twins.
Recently, the patatin-like phospholipase domain-containing 3 (PNPLA3) gene,
also known as adiponutrin, has been implicated in the pathogenesis of both ALD
and NAFLD .
•Nutrition. Obesity increases the incidence of liver-related mortality by over 5 fold
in heavy drinkers
2
أ.د حسن سالم الجميلي باطن
يه الكورس الثاني
lec3
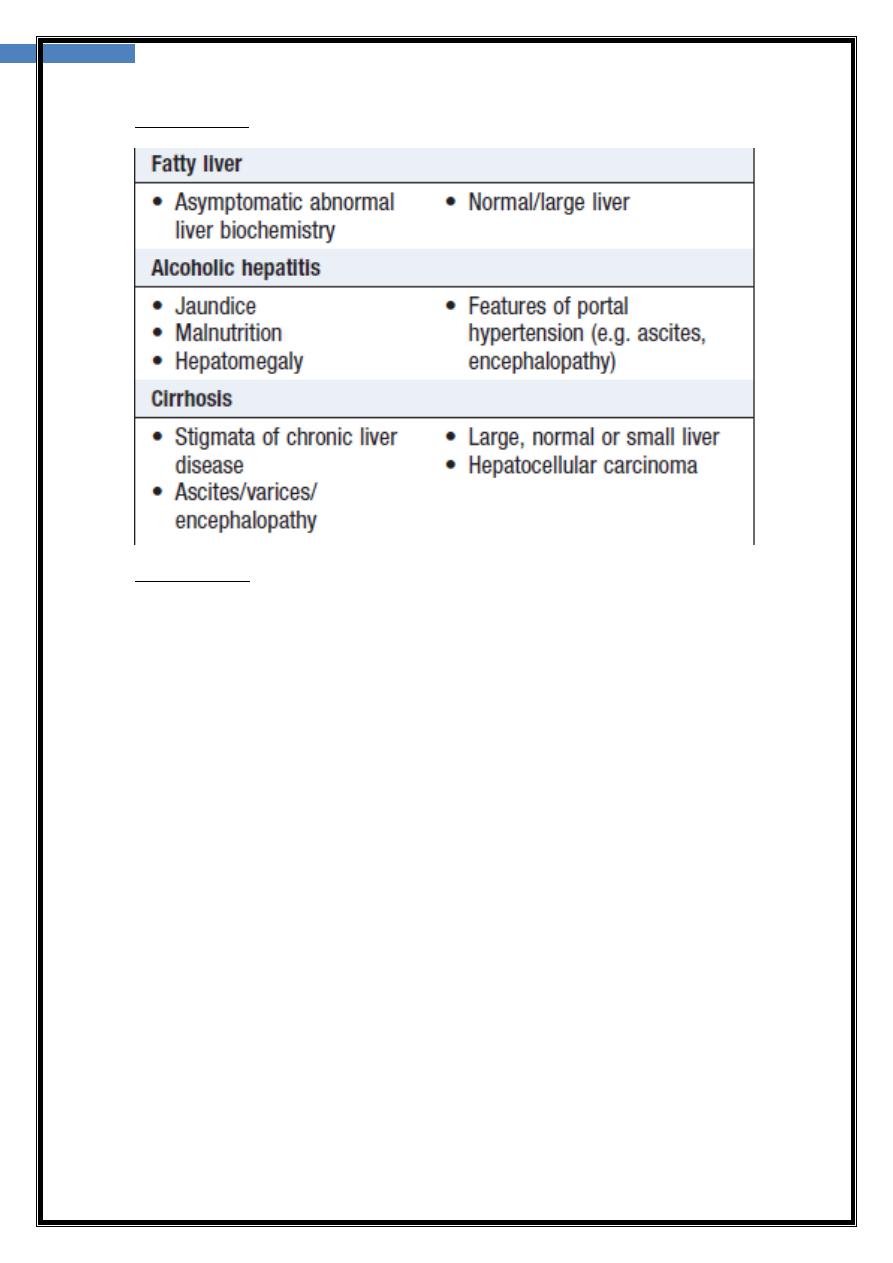
Clinical feature
Investigations
1-macrocytosis in the absence of anaemia,
2-↑GGT is not specific .
3-presence of jaundice may suggest alcoholic hepatitis. 4 -extent of liver damage
ofte requires a liver biopsy.
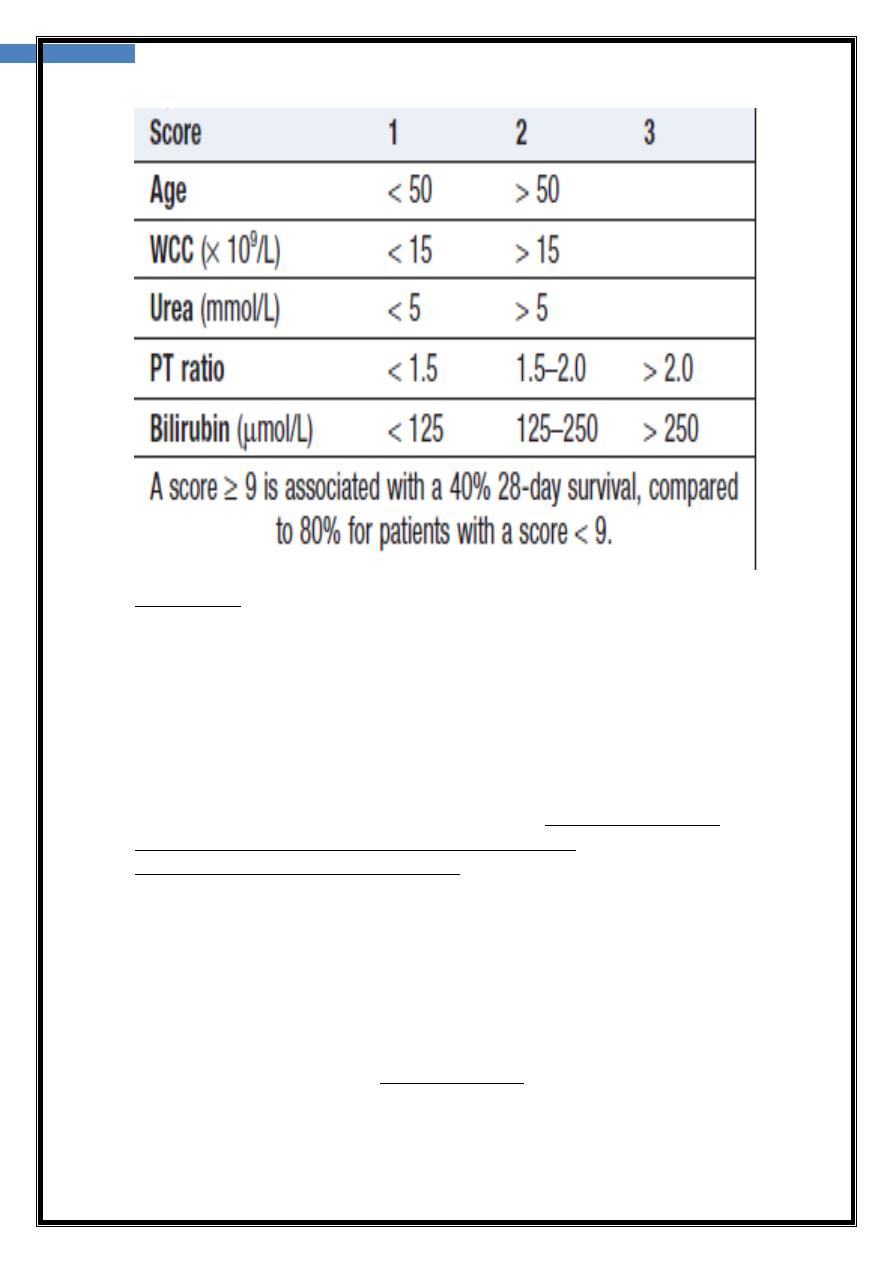
5-In alcoholic hepatitis, PT and bilirubin are used to
calculate a ‘discriminant function’ (DF), also known as
the Maddrey score, which enables the clinician to assess
prognosis (PT = prothrombin time; serum bilirubin in
μmol/L is divided by 17 to convert to mg/dL):
DF= [4.6 x Increase in PT in sec]+Bilirubin (mg/dL)
A value over 32 implies severe liver disease with a poor
▲
A second scoring system, the Glasgow score
3
أ.د حسن سالم الجميلي باطن
يه الكورس الثاني
lec3
Management
1-Cessation of alcohol consumption is the single most
important treatment and prognostic factor..
2-Nutrition :enteral feeding via a fine-bore nasogastric tube may be needed in
severely ill patients
3-Corticosteroids
These are of value in patients with severe alcoholic
hepatitis (Maddrey’s discriminative score > 32) and
increase survival. Sepsis is the main side-effect of steroids,anexisting sepsis and
If the bilirubin has not
varicealhaemorrhage are the main contraindications.
fallen 7 days after starting steroids, the drugs are unlikely
to reduce mortality and should be stopped
4-Pentoxifylline :anti-TNF action, may
be beneficial in severe alcoholic hepatitis. It reduces the incidence of hepatorenal
failure and its use is not complicated by sepsis
5-Liver transplantation.
Many programmes require a 6-month period of abstinence from alcohol before a
patient is considered for transplantation. The outcome of transplantation for
ALD is good and, if the patient remain abstinent, there is no risk of disease
has a poorer outcome and is
alcoholic hepatitis
recurrence. Transplantation for
seldom performed
4
أ.د حسن سالم الجميلي باطن
يه الكورس الثاني
lec3
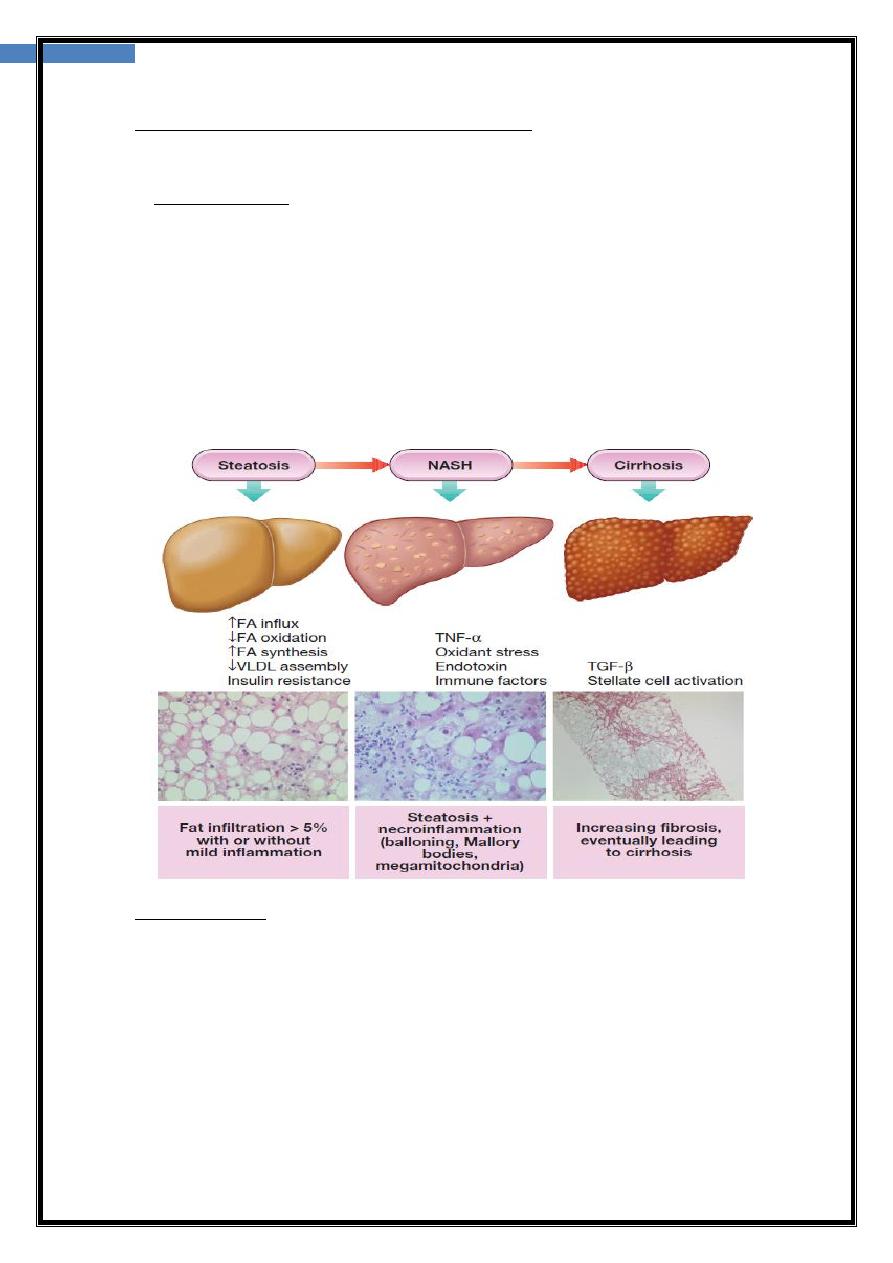
LCOHOLIC FATTY LIVER DISEASE
A
-
NON
a spectrum of liver disease :simple fatty infiltration (steatosis), fat and
inflammation (nonalcoholic steatohepatitis, NASH) and cirrhosis, in the absence
for women
consumption (typically a threshold of < 20 g/day
excessive alcohol
of
and < 30 g/day for men is adopted.
▲
NAFLD is strongly associated with obesity, dyslipidaemia, insulin resistance
and type 2 DM, and so may be considered to be the hepatic manifestation of the
‘metabolic syndrome’
▲
NAFLD to be present in 94% of obese patients (body mass index (BMI) > 30
kg/m2), 67% of overweight patients (BMI > 25 kg/m2) and 25% of normal-
weight patients. The overall prevalence of NAFLD in patients with type 2 diabetes
ranges from 40% to 70%.
Clinical features
1- asymptomatic an incidental biochemical abnormality during routine blood
test
2-fatigue and mild right upper quadrant discomfort
3- patients with progressive NASH may present late in the natural history of the
disease with complications of cirrhosis and portal hypertension, such as
varicealhaemorrhage, or HCC.
4-The average age of NASH patients is 40–50 years (50–60 y) for NASH–cirrhosis.
5-Most patients with NAFLD have insulin resistance and exhibit features of the
metabolic syndrome.
5
أ.د حسن سالم الجميلي باطن
يه الكورس الثاني
lec3
ase progression
independent risk factors for dise
1- age over 45 years 2- presence of diabetes
3- obesity (BMI > 30 kg/m2) 4- hypertension.
-NAFLD is also associated with PCOS, obstructive sleep apnoea&
small-bowel bacterial overgrowth
Investigations
1-exclusion of excess alcohol consumption and other liver diseases (viral,
autoimmune and other metabolic causes),
2-confirming the presence of NAFLD, discriminating simple steatosis from NASH
and determining the extent of any hepatic fibrosis that is present.
-Biochemical tests
↑
ALT and AST are modest, and usually less than twice the upper limit
-Characteristic AST : ALT ratio of <1 seen in NASH while (AST : ALT > 1) as
disease progresses towards cirrhosis
-non-specific elevations of GGT, low-titreANA in 20–30% of patients and ↑ferritin
-Ultrasound is assessment of hepatic fat content, as the liver appears
‘bright’ due to increased echogenicity; however, sensitivity
is limited when fewer than 33% of hepatocytes are steatotic.
Alternatives include CT, MRI.
-Liver biopsy
‘gold standard’ investigation for diagnosis and assessment of degree of
important to note that hepatic fat content tends to diminish as
inflammation It is
diagnosed in the setting of
-
cirrhosis develops and so NASH is likely to be under
, where it is thought to be the underlying cause is readily
ed liver disease
advanc
identified (so-called ‘cryptogenic cirrhosis’). of 30–75% of cases in which no
specific aetiology
Management
pharmacological treatment
-
Non
weight loss and improve insulin sensitivity through dietary changes and physical
exercise.
Pharmacological treatment
♠
No pharmacological agents are currently licensed specifically
for NASH therapy. Treatment directed at coexisting metabolic disorders, such as
dyslipidaemia and hypertension.
♠
Specific insulin-sensitising agents, in particular glitazones,
may help selected patients.
♠
positive results with high-dose vitamin E (800 U/day) but high doses may be
associated with an increased risk of prostate cancer, which has limited its use
6
أ.د حسن سالم الجميلي باطن
يه الكورس الثاني
lec3
PREGNANCY AND THE LIVER
♠
It is critical to obtain information relating to liver disease risk factors and pre-
pregnancy liver status to establish whether any abnormality was present before
pregnancy.
♠
In general, the earlier in pregnancy that liver abnormality presents, the more
likely it is to represent either preexisting liver disease or non-pregnancy-related
acute liver disease.
Intercurrent and pre-existing
liver disease
1-Acute hepatitis A→ no effect on the fetus.
2-Chronic hepatitis B → effectiveness of perinatal
vaccination (with or without pre-delivery maternal
antiviral therapy) in reducing neonatal acquisition of
chronic hepatitis B.
3- Maternal transmission of hepatitis C occurs in 1% of cases.
4-Hepatitis E→ progress to acute liver failure much more
commonly in pregnancy, with a 20-25% maternal mortality.
5- worsening or improvement of autoimmune hepatitis, although improvement
during pregnancy and rebound postpartum is the most common pattern seen.
6-Complications of portal hypertension may be a particular issue in the second
and third trimesters.
Gallstones are more common during pregnancy
-
7
and may present with cholecystitis or biliary
obstruction. The diagnosis can usually be made with
. In biliary obstruction due to gallstones,
ultrasound
lead protection for the fetus is
can be safely performed, but
ERCP
therapeutic
essential and X-ray screening must be kept to a minimum
Pregnancy-associated liver disease
Acute cholestasis of pregnancy
-
20% of cases of jaundice in pregnancy
-
-third trimester of pregnancy but can arise earlier.
associated with intrauterine fetal death if the pregnancy goes beyond 36 weeks
C.F: itching and cholestatic LFTs. A normal bilirubin and hepatitic LFT do not
preclude the diagnosis.
Mx:
1-Delivery leads to resolution and should be considered from 36 weeks onwards.
2-UDCA (15 mg/kg daily) effectively controls itching and probably prevents
premature birth. long time required to achieve effective levels
which renders it of little use in patients presenting in the very end stages of
Cholestasis recurs in 60% of future pregnancies and the
pregnancy.
7
أ.د حسن سالم الجميلي باطن
يه الكورس الثاني
lec3
opportunities available for screening based on previous risk make UDCA a much
iable Rx
more v
Acute fatty liver of pregnancy
-more common in twin and first pregnancies, fetus male.
-between 31 and 38 weeks of pregnancy
C.F: vomiting and abdominal pain followed by jaundice. In severe cases, this may
be lactic acidosis, coagulopathy, encephalopathy and renal failure.
Hypoglycaemia can also occur.
Mechanism:
1-defect in beta-oxidation of fatty acids in the mitochondria that leads to the
formation of small fat droplets in liver cells (known as microvesicular fatty liver).
2-Some women are heterozygous for loss-of-function mutations in the long-
chain 3- hydroxyacyl-CoA dehydrogenase (LCHAD) gene.
high serum uric acid levels and
emia of pregnancy by
from toxa
Differentiation
the absence of haemolysis.
Early diagnosis, specialist care and delivery of the fetus have led to a fall in
maternal and perinatal mortality to 1% and 7% respectively
Toxaemia of pregnancy and HELLP
The HELLP syndrome (haemolysis, elevated liver enzymes and low platelets) is a
variant of pre-eclampsia that tends to affect multiparous women.
CF: usually presents at 27–36 weeks of pregnancy with hypertension proteinuria and
fluid retention. Jaundice only occurs in 5% ocases.
Invex→lowHb, fragmented red cells, ↑ serum transaminase and↑ D-dimers.
Cx: hepatic infarction and rupture, DIC and placental abruption. Maternal mortality
is 1% and perinatal mortality can be up to 30%.
Mx: Delivery usually leads to prompt resolution, and disease recur in fewer than 5%
of subsequent pregnancies
