
The Acute Abdomen
:
"An acute abdomen" is any sudden, spontaneous, nontraumatic
disorder whose chief manifestation is in the abdominal area and
for which urgent operation may be necessary. Because there is
frequently a progressive underlying intra-abdominal disorder,
undue delay in diagnosis and treatment adversely affects outcome.
The approach to a patient with an acute abdomen must be orderly
and thorough. An acute abdomen must be suspected even if the
patient has only mild or atypical complaints. The history and
physical examination should suggest the probable causes and
guide the choice of initial diagnostic studies..
History Abdominal Pain
History taking by an experienced physician is an active process
whereby a cluster of diagnostic possibilities is considered in order
to systematically eliminate less likely conditions. Pain is the most
common and predominant presenting feature of an acute abdomen.
Careful consideration of the location, the mode of onset and
progression, and the character of the pain will suggest a
preliminary list of differential diagnoses.
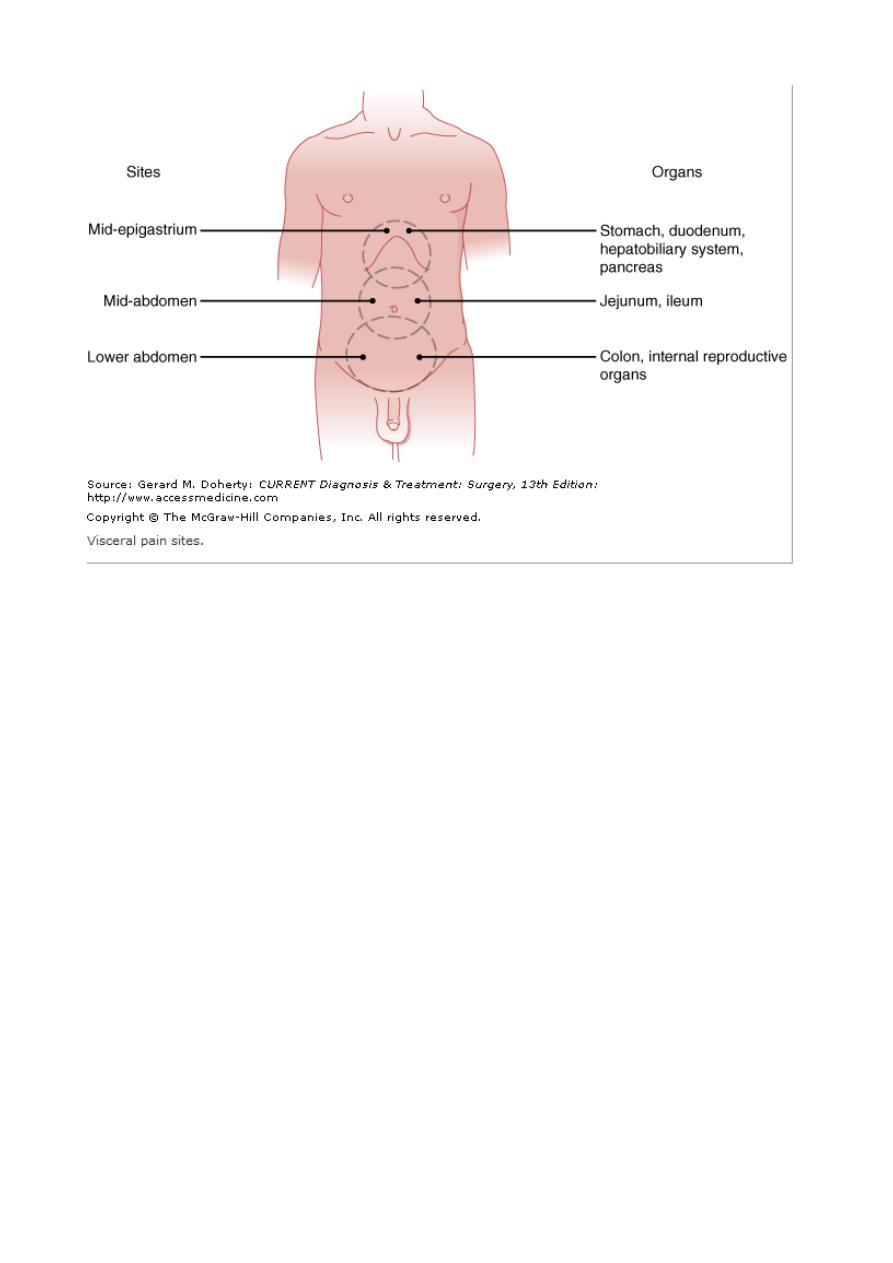
Location
of Pain
Because of the complex dual visceral and parietal sensory network
innervating the abdominal area, pain is not as precisely localized
as in the extremities.. Visceral sensation is mediated primarily by
afferent C fibers located in the walls of hollow viscera and in the
capsules of solid organs. Unlike cutaneous pain, visceral pain is
elicited by distention, by inflammation or ischemia stimulating the
receptor neurons, or by direct involvement (eg, malignant
infiltration) of sensory nerves. The centrally perceived sensation is
generally slow in onset, dull, poorly localized, and protracted.
Because of this, increased wall tension due to luminal distention
or forceful smooth muscle contraction (colic) produces diffuse,
deep-seated pain felt in the midepigastrium, periumbilical area,
lower abdomen, or flank areas .. Visceral pain is most often felt in
the midline because of the bilateral sensory supply to the spinal
cord
By contrast, parietal pain is mediated by both C and A delta
nerve fibers, the latter being responsible for the transmission of
more acute, sharper, better-localized pain sensation. Direct
irritation of the somatically innervated parietal peritoneum
(especially the anterior and upper parts) by pus, bile, urine, or
gastrointestinal secretions leads to more precisely localized pain.
The cutaneous distribution of parietal pain corresponds to the T6–
L1 areas. Parietal pain is more easily localized than visceral pain
because the somatic afferent fibers are directed to only one side of
the nervous system.
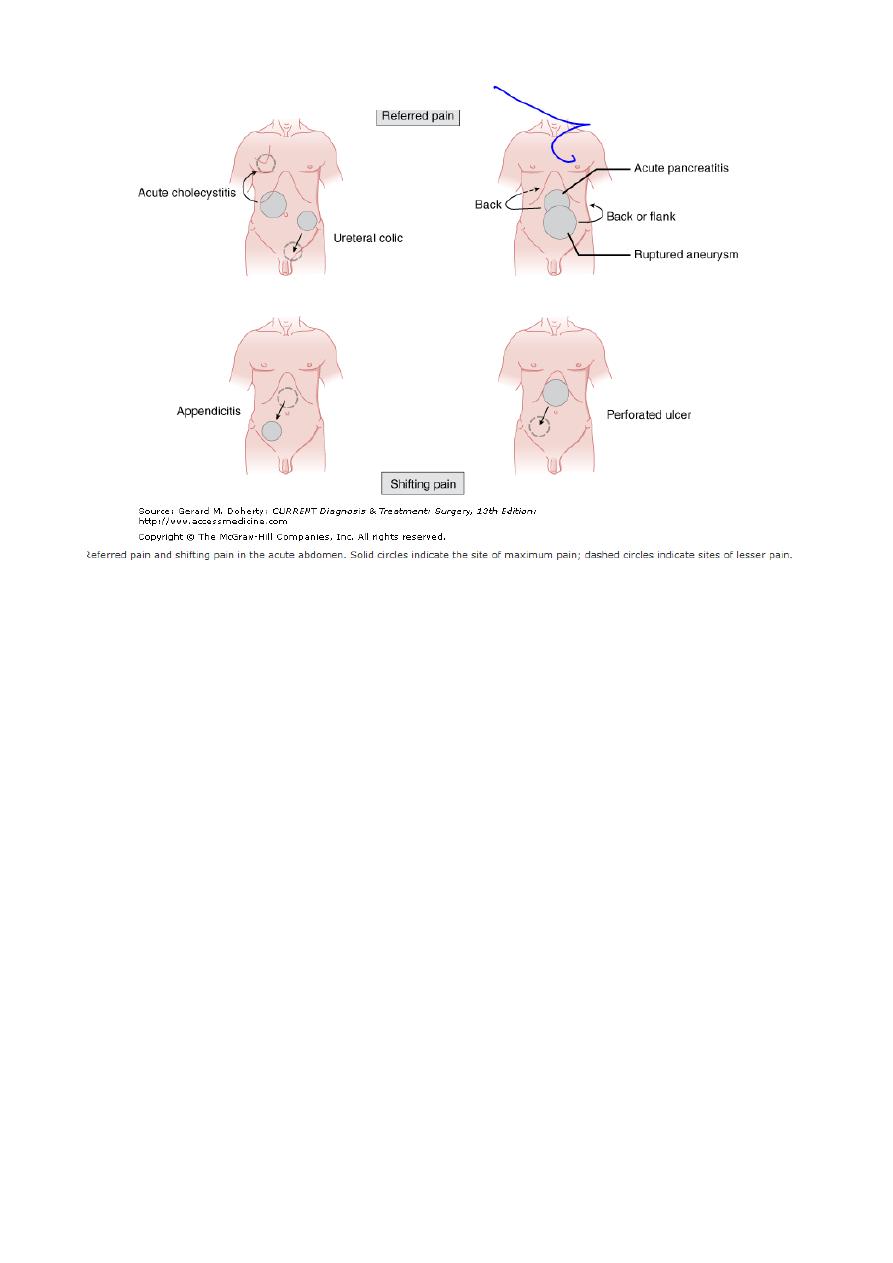
Abdominal pain may be referred or may shift to sites far removed
from the primarily affected organs .Referred pain denotes
noxious (usually cutaneous) sensations perceived at a site distant
from that of a strong primary stimulus. Distorted central
perception of the site of pain is due to the confluence of afferent
nerve fibers from widely disparate areas within the posterior horn
of the spinal cord. For example, pain due to subdiaphragmatic
irritation by air, peritoneal fluid, blood, or a mass lesion is referred
to the shoulder via the C4-mediated (phrenic) nerve. Pain may
also be referred to the shoulder from supradiaphragmatic lesions
such as pleurisy or lower lobe pneumonia, especially in young
patients. Although more often perceived in the right scapular
region, referred biliary pain may mimic angina pectoris if it is
perceived in the anterior chest or left shoulder areas. Posterolateral
right flank pain may be seen in retrocecal appendicitis.
Spreading or shifting pain. Beginning classically in the
epigastric or periumbilical region, the incipient visceral pain of
acute appendicitis (due to distention of the appendix) later shifts to
become sharper parietal pain localized in the right lower quadrant
when the overlying peritoneum becomes directly inflamed . In
perforated peptic ulcer, pain almost always begins in the
epigastrium, but as the leaked gastric contents track down the right
paracolic gutter, pain may descend to the right lower quadrant
with even diminution of the epigastric pain.
The location of pain serves only as a rough guide to the
diagnosis—"typical" descriptions are reported in only two thirds
of cases. This great variability is due to atypical pain patterns, a
shift of maximum intensity away from the primary site, or
advanced or severe disease. In cases presenting late with diffuse
peritonitis, generalized pain may completely obscure the
precipitating event..
Mode of Onset and Progression of Pain
The mode of onset of pain reflects the nature and severity of the
inciting process. Onset may be explosive (within seconds), rapidly
progressive (within 1–2 hours), or gradual (over several hours).
Unheralded, excruciating generalized pain suggests an intra-
abdominal catastrophe such as a perforated viscus or rupture of an
aneurysm, ectopic pregnancy, or abscess. Accompanying systemic
signs (tachycardia, sweating, tachypnea, shock) soon supersede
the abdominal disturbances and underscore the need for prompt
resuscitation and laparotomy.
A less dramatic clinical picture is steady, mild pain becoming
intensely centered in a well-defined area within 1–2 hours. Any of
the above conditions may present in this manner, but this mode of
onset is more typical of acute cholecystitis, acute pancreatitis,
strangulated bowel, mesenteric infarction, renal or ureteral colic,
and high (proximal) small bowel obstruction.

Finally, some patients initially have slight—at times only vague—
abdominal discomfort that is fleetingly present diffusely
throughout the abdomen. It may be unclear whether these patients
even have an acute abdomen or whether the illness is likely to be a
matter for medical rather than surgical attention. Associated
gastrointestinal symptoms are infrequent at first, and systemic
symptoms are absent. Eventually, the pain and abdominal findings
become more pronounced and steady and are localized to a
smaller area. This pattern may reflect a slowly developing
condition or the body's defensive efforts to cordon off an acute
process. This broad category includes acute appendicitis
(especially retrocecal or retroileal), incarcerated hernias, low
(distal) small bowel and large bowel obstructions, uncomplicated
peptic ulcer disease, walled-off (often malignant) visceral
perforations, some genitourinary and gynecologic conditions, and
milder forms of the rapid-onset group mentioned in the first
paragraph.
Character of Pain
The nature, severity, and periodicity of pain provide useful clues
to the underlying cause (Figure). Steady pain is most common.
Sharp superficial constant pain due to severe peritoneal irritation
is typical of perforated ulcer or a ruptured appendix, ovarian cyst,
or ectopic pregnancy. The gripping, mounting pain of small bowel
obstruction (and occasionally early pancreatitis) is usually
intermittent, vague, deep-seated, and crescendo at first but soon
becomes sharper, unremitting, and better localized. Unlike the
disquieting but bearable pain associated with bowel obstruction,
pain caused by lesions occluding smaller conduits (bile ducts,
uterine tubes, and ureters) rapidly becomes unbearably intense.
Pain is appropriately referred to as colic if there are pain-free
intervals that reflect intermittent smooth muscle contractions, as in
ureteral colic. .. The "aching discomfort" of ulcer pain, the
"stabbing, breathtaking" pain of acute pancreatitis and mesenteric

infarction, and the "searing" pain of ruptured aortic aneurysm
remain apt descriptions. Despite the use of such descriptive terms,
the quality of visceral pain is not a reliable clue to its cause.
Other Symptoms Associated with Abdominal Pain
Anorexia, nausea and vomiting, constipation, or diarrhea often
accompanies abdominal pain, but since these are nonspecific
symptoms, they do not have much diagnostic value.
Vomiting
When sufficiently stimulated by secondary visceral afferent fibers,
the medullary vomiting centers activate efferent fibers to induce
reflex vomiting. Hence, pain in the acute surgical abdomen
usually precedes vomiting, whereas the reverse holds true in
medical conditions. Vomiting is a prominent symptom in upper
gastrointestinal diseases such as acute gastritis, and acute
pancreatitis. Severe, uncontrollable retching provides temporary
pain relief in moderate attacks of pancreatitis. The absence of bile
in the vomitus is a feature of pyloric stenosis. Where associated
findings suggest bowel obstruction, the onset and character of
vomiting may indicate the level of the lesion. Recurrent vomiting
of bile-stained fluid is a typical early sign of proximal small bowel
obstruction. In distal small or large bowel obstruction, prolonged
nausea precedes vomiting, which may become feculent in late
cases.. Although vomiting may present in either acute appendicitis
or nonspecific abdominal pain, coexisting nausea and anorexia are
more suggestive of the former condition.
Constipation Reflex ileus is often induced by visceral afferent
fibers stimulating efferent fibers of the sympathetic autonomic
nervous system (splanchnic nerves) to reduce intestinal peristalsis.
Hence, paralytic ileus undermines the value of constipation in the
differential diagnosis of an acute abdomen. Constipation itself is
hardly an absolute indicator of intestinal obstruction. However,
obstipation (the absence of passage of both stool and flatus)
strongly suggests mechanical bowel obstruction if there is
progressive painful abdominal distention or repeated vomiting.
Diarrhea Copious watery diarrhea is characteristic of
gastroenteritis and other medical causes of an acute abdomen.
Blood-stained diarrhea suggests ulcerative colitis, Crohn disease,
or bacillary or amebic dysentery. It is also common with ischemic
colitis but often absent in intestinal infarction due to superior
mesenteric artery occlusion.
Other Relevant Aspects of the History
Gynecologic History The menstrual history is crucial to the
diagnosis of ectopic pregnancy, mittelschmerz (due to a ruptured
ovarian follicle), and endometriosis. A history of vaginal
discharge or dysmenorrhea may denote pelvic inflammatory
disease.
Drug History Anticoagulants have been implicated in
retroperitoneal and intramural duodenal and jejunal hematomas;
oral contraceptives have been implicated in the formation of
benign hepatic adenomas and in mesenteric venous infarction.
Corticosteroids, in particular, may mask the clinical signs of even
advanced peritonitis.
Family History :Family history often provides the best
information about medical causes of an acute abdomen.
.
Operation History Any history of a previous abdominal, groin,
vascular, or thoracic operation may be relevant to the current
illness. Particular attention to the mode of operation (laparoscopic,
open, endovascular) and any anatomic reconstructions may clarify
aspects of the current complaint
Physical Examination

The tendency to concentrate on the abdomen should be resisted in
favor of a methodical and complete general physical examination.
A systematic approach to the abdominal examination noticing
specific signs that confirm or rule out differential diagnostic
possibilities
General observation: General observation affords a fairly
reliable indication of the severity of the clinical situation. The
writhing of patients with visceral pain (eg, intestinal or ureteral
colic) contrasts with the rigidly motionless bearing of those with
parietal pain (eg, acute appendicitis, generalized peritonitis).
Diminished responsiveness or an altered sensorium often precedes
imminent cardiopulmonary collapse.
Systemic signs: Systemic signs usually accompany rapidly
progressive or advanced disorders associated with an acute
abdomen. Extreme pallor, hypothermia, tachycardia, tachypnea,
and sweating suggest major intra-abdominal hemorrhage (eg,
ruptured aortic aneurysm or tubal pregnancy). Given such
findings, one must proceed rapidly with the subsequent
examination and tests in order to exclude extra-abdominal causes.
Fever: Constant low-grade fever is common in inflammatory
conditions such as diverticulitis, acute cholecystitis, and
appendicitis. High fever with lower abdominal tenderness in a
young woman without signs of systemic illness suggests acute
salpingitis. Disorientation or extreme lethargy combined with a
very high fever (> 39 °C) or swinging fever or with chills and
rigors signifies impending septic shock. This is most often due to
advanced peritonitis, acute cholangitis, or pyelonephritis.
However, fever is often mild or absent in elderly, chronically ill,
or immunosuppressed patients with a serious acute abdomen.
Inguinal and femoral rings; male genitalia: The inguinal and
femoral rings in both sexes and the genitalia in male patients
should be examined next.
Rectal examination: A rectal examination should be performed in
most patients with an acute abdomen. Diffuse tenderness is
nonspecific, but right-sided rectal tenderness accompanied by
lower abdominal rebound tenderness is indicative of peritoneal
irritation due to pelvic appendicitis or abscess. Other useful
findings include a rectal tumor, blood-stained stool, or occult
blood (detected by guaiac testing
Pelvic examination: An acute abdomen is incorrectly diagnosed
more often in women than in men, particularly in younger age
groups. A pelvic examination is vital in women with a vaginal
discharge, dysmenorrhea, menorrhagia, or left lower quadrant
pain..
Investigative Studies
The history and physical examination by themselves provide the
diagnosis in two thirds of cases of an acute abdomen.
Supplementary laboratory and radiologic examinations are
indispensable for diagnosis of many surgical conditions, for
exclusion of medical causes ordinarily not treated by operation,
and for assistance
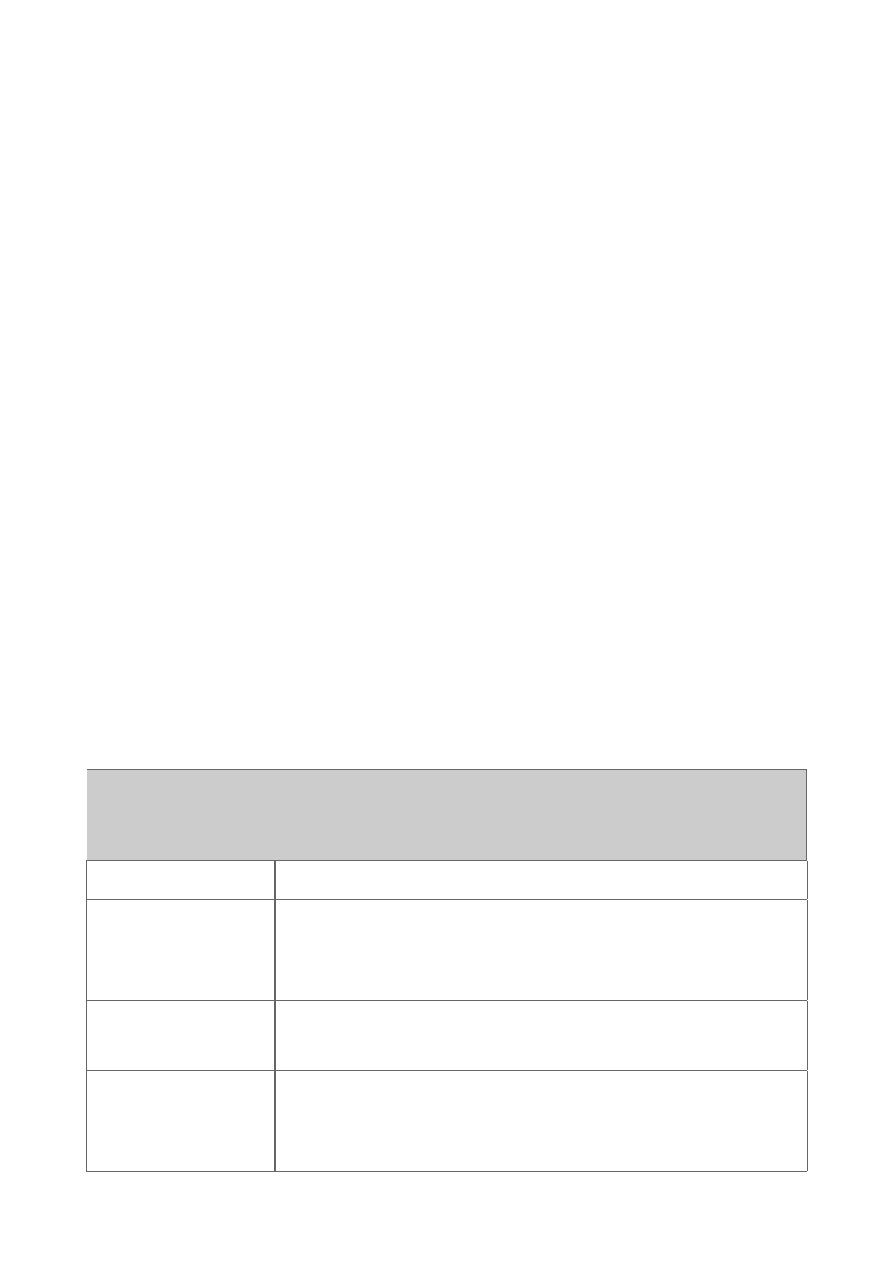
Physical Findings in Various Causes of Acute Abdomen.
Condition
Helpful Signs
Perforated
viscus
Scaphoid, tense abdomen; diminished bowel
sounds (late); loss of liver dullness; guarding or
rigidity.
Peritonitis
Motionless; absent bowel sounds (late); cough
and rebound tenderness; guarding or rigidity.
Inflamed mass
or abscess
Tender mass (abdominal, rectal, or pelvic);
bump tenderness; special signs (Murphy, psoas,
or obturator).
Intestinal
obstruction
Distention; visible peristalsis (late);
hyperperistalsis (early) or quiet abdomen (late);
diffuse pain without rebound tenderness; hernia
or rectal mass (some).
Paralytic ileus
Distention; minimal bowel sounds; no localized
tenderness.
Ischemic or
strangulated
bowel
Not distended (until late); bowel sounds
variable; severe pain but little tenderness; rectal
bleeding (some).
Bleeding
Pallor, shock; distention; pulsatile (aneurysm)
or tender (eg, ectopic pregnancy) mass; rectal
bleeding (some).
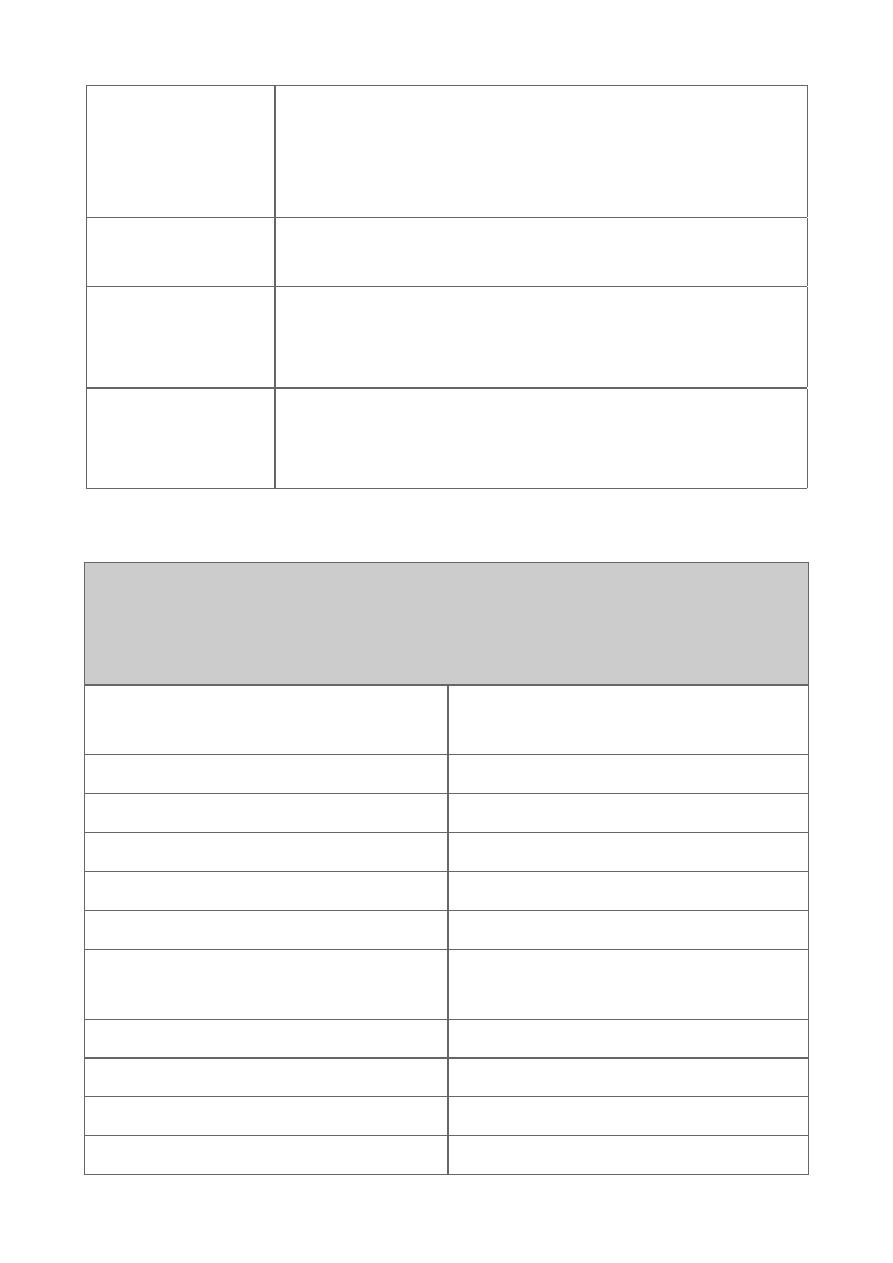
Medical Causes of an Acute Abdomen for which Surgery Is Not
Indicated.
Endocrine and metabolic
disorders
Infections and inflammatory
disorders
Uremia
Tabes dorsalis
Diabetic crisis
Herpes zoster
Addisonian crisis
Acute rheumatic fever
Acute intermittent porphyria
Henoch-Schönlein purpura
Acute hyperlipoproteinemia
Systemic lupus erythematosus
Hereditary Mediterranean
fever
Polyarteritis nodosa
Hematologic disorders
Referred pain
Sickle cell crisis
Thoracic region
Acute leukemia
Myocardial infarction
Other dyscrasias
Acute pericarditis
Toxins and drugs
Pneumonia
Lead and other heavy metal
poisoning
Pleurisy
Narcotic withdrawal
Pulmonary embolus
Black widow spider poisoning Pneumothorax
Empyema
Hip and back
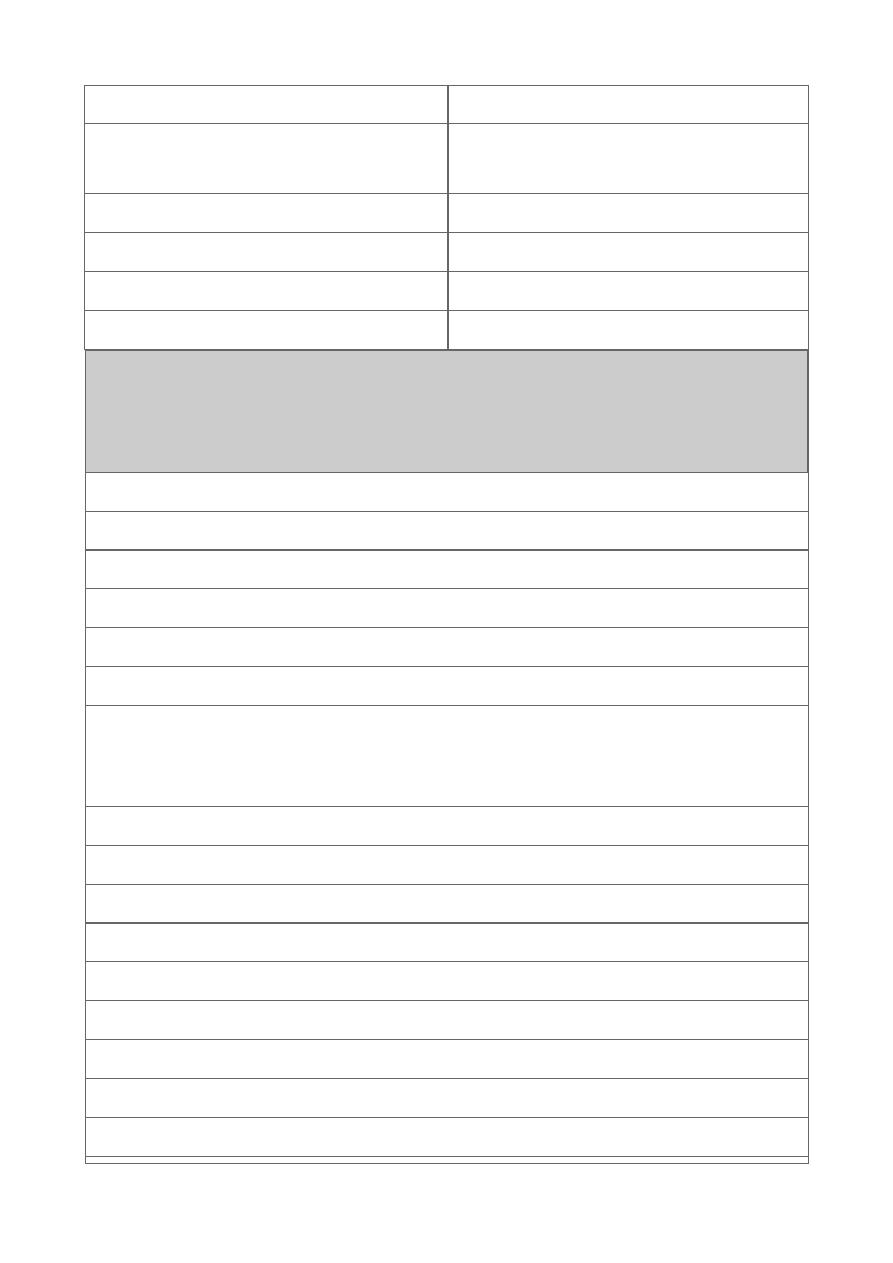
Indications for Urgent Operation in Patients with an Acute
Abdomen.
Physical findings
Involuntary guarding or rigidity, especially if spreading
Increasing or severe localized tenderness
Tense or progressive distention
Tender abdominal or rectal mass with high fever or hypotension
Rectal bleeding with shock or acidosis
Equivocal abdominal findings along with septicemia (high
fever, marked or rising leukocytosis, mental changes, or
increasing glucose intolerance in a diabetic patient)
Bleeding (unexplained shock or acidosis, falling hematocrit)
Suspected ischemia (acidosis, fever, tachycardia)
Deterioration on conservative treatment
Radiologic findings
Pneumoperitoneum
Gross or progressive bowel distention
Free extravasation of contrast material
Space-occupying lesion on scan, with fever
Mesenteric occlusion on angiography

.
