
THE LIVER
Anatomy of the liver its parenchyma is entirely covered by a thin capsule and by
visceral peritoneum on all but the posterior surface of the liver, termed the ‘bare area’
The blood supply to the liver is unique, 80 per cent being derived from the portal vein
and 20 per cent from the hepatic artery. The arterial blood supply in most individuals
is derived from the coeliac trunk of the aorta, where the hepatic artery arises along
with the splenic artery.
Structures in the hilum of the liver;
The porta hepatis, a transverse fissure on the visceral surface of the liver, is the
hilum of the liver .The usual anatomical relationship of the structures is for the bile
duct to be within the free edge of the lesser omentum or the ‘hepatoduodenal
ligament’, the hepatic artery to be above and medial, and the portal vein to lie
posteriorly; and together with nerves and lymphatics enter the liver at the porta
hepatis .
SEGMENTAL ANATOMY OF THE LIVER
Couinaud, a French anatomist, described the liver as being divided into eight
segments . Each of these segments can be considered as a functional unit, with a
branch of the hepatic artery, portal vein and bile duct, and drained by a branch of the
hepatic vein. The overall anatomy of the liver is divided into a functional right and
left ‘unit’ along the line between the gall bladder fossa and the middle hepatic vein
(Cantlie’s line). Liver segments (V–VIII), to the right of this line, To the left of this
line (segments I–IV), functionally is the left liver
.
Liver blood supply
_
There are two anatomical lobes with separate blood supply, bile duct and
venous drainage
_
Dual blood supply (20 per cent hepatic artery and 80 per
cent portal vein)
_
The liver regenerates fully after partial resection
_
Resection is based on anatomical lines to preserve maximal functioning liver.
Liver function :Humans will survive for only 24–48 hours in the anhepatic state
despite full supportive therapy. Bilirubin Increased levels may be associated with

increased haemoglobin breakdown, hepatocellular dysfunction resulting in impaired
bilirubin transport and excretion, or biliary obstruction. In patients with known
parenchymal liver disease, progressive elevation of bilirubin in the absence of a
secondary complication suggests deterioration in liver function. The serum alkaline
phosphatase is particularly elevated with cholestatic liver disease or biliary
obstruction. The transaminase levels (aspartate transaminase(AST) and alanine
transaminase (ALT)) reflect acute hepatocellular damage, as does the gamma-
glutamyl transpeptidase (GGT) level, which may be used to detect the liver injury
associated with acute alcohol ingestion. The synthetic functions of the liver are
reflected in the ability to synthesise proteins (albumin level) and clotting factors
(prothrombin time). The standard method of monitoring liver function in patients
with chronic liver disease is serial measurement of bilirubin, albumin and
prothrombin time.
Clinical signs of impaired liver function
These signs depend on the severity of dysfunction and whether it is acute or chronic.
Features of
chronic
liver disease_
Lethargy
_
Fever
_
Jaundice
_
Protein
catabolism (wasting)
_
Coagulopathy (bruising)
_
Cardiac (hyperdynamic
circulation )
_
Neurological (hepatic encephalopathy)
_
Portal hypertension
Ascites Oesophageal varices Splenomegaly
_
Cutaneous :Spider naevi
Palmar erythema
Laparoscopy
Laparoscopy is useful for the staging of hepatopancreatobiliary cancers particularly
primary liver and biliary tract cancers.Lesions overlooked by conventional imaging
are mainly peritoneal metastases and superficial liver tumours. These lesions can be
detected at laparoscopy, thus avoiding an unnecessary laparotomy. A liver biopsy to
confirm or exclude chronic liver disease can also be performed during laparoscopy
LIVER TRAUMA
General
The liver is the second most common organ injured in abdominal trauma..Blunt
injury produces contusion, laceration and avulsion injuries to the liver, often in
association with splenic, mesenteric or renal injury. Penetrating injuries, such as stab
and gunshot wounds, are often associated with chest or pericardial involvement .
Blunt injuries are more common and have a higher mortality than penetrating
injuries.
Summary box 65.7
Diagnosis of liver injury
The liver is an extremely well-vascularised organ, and blood loss is therefore the
major early complication of liver injuries. Clinical suspicion of a possible liver injury
is essential, as a laparotomy by an inexperienced surgeon with inadequate preparation
preoperatively is doomed to failure. All lower chest and upper abdominal stab
wounds should be suspect, especially if considerable blood volume replacement has
been required. Similarly, severe crushing injuries to the lower chest or upper

abdomen often combine rib fractures, haemothorax and damage to the spleen and/or
liver. Focused assessment sonography in trauma (FAST) performed in the emergency
room by an experienced operator can reliably diagnose free intraperitoneal fluid.
Patients with free intraperitoneal fluid on FAST and haemodynamic instability, and
patients with a penetrating wound will require a laparotomy and/or thoracotomy once
active resuscitation is under way. Owing to the opportunity for massive ongoing
blood loss and the rapid development of a coagulopathy, the patient should be
directly transferred to the operating theatre while blood products are obtained and
volume replacement is taking place. Patients who are haemodynamically stable
should have a contrast-enhanced CT scan of the chest and abdomen as the next step.
This will demonstrate evidence of parenchymal damage to the liver or spleen, as well
as associated traumatic injuries to their feeding vessels. Free fluid can also be clearly
established. The chest scan will help to exclude injuries to the great vessels and
demonstrate damage to the lung parenchyma.
Management of liver trauma
_
Remember associated injuries
_
At-risk groups Stabbing/gunshot in lower chest or upper abdomen
Crush injury with multiple rib fractures
_
Resuscitate
Airway
Breathing
Circulation
_
Assessment of injury : CT chest and abdomen with contrast Laparotomy
if haemodynamically unstable
_
Treatment
Correct coagulopathy
Suture lacerations
Resect if major vascular injury
Packing if diffuse parenchymal injury
Other complications of liver trauma
A subcapsular or intrahepatic haematoma requires no specific intervention and should
be allowed to resolve spontaneously.
Abscesses may form as a result of secondary infection of an area of parenchymal
ischaemia, especially after penetrating trauma. Treatment is with systemic antibiotics
and aspiration under ultrasound guidance once the necrotic tissue has liquefied. Bile
collections require aspiration under ultrasound guidance or percutaneous insertion of
a pigtail drain Late vascular complications include hepatic artery aneurysm and
arteriovenous or arteriobiliary fistulae. These are best treated nonsurgically by a
specialist hepatobiliary interventional radiologist.
CHRONIC LIVER CONDITIONS
There are several chronic liver conditions, which, although rare, are important to
recognise because they require a specific plan for investigation and treatment, and

may present mimickinga more common clinical condition
Important chronic liver conditions.
Condition Common presentations
Budd
–Chiari syndrome Ascites
Primary sclerosing cholangitis(PSC) Abnormal LFTs or
jaundice
Primary biliary cirrhosis (PBC) Malaise, lethargy, itching,
abnormal LFTs
Caroli’s disease Abdominal pain, sepsis
Simple liver cysts Coincidental finding, pain
Polycystic liver disease Hepatomegaly, pain
Budd
–Chiari syndrome
This is a condition principally affecting young females, in which the venous drainage
of the liver is occluded by hepatic venous thrombosis or obstruction from a venous
web. As a result of venous outflow obstruction, the liver becomes acutely congested,
with the development of impaired liver function and, subsequently, portal
hypertension, ascites and oesophageal varices. Treatment of Patients presenting in
fulminant liver failure should be considered for liver transplantation, as should those
with established cirrhosis and the complications of portal hypertension. Those in
whom is not established may be considered for portosystemic shunting by TIPSS,
portocaval shunt or mesoatrial shunting.
Primary sclerosing cholangitis
This condition often presents in young adults with mild nonspecific symptoms, and
biliary disease is suggested by the finding of abnormal liver function tests. Rarely, the
first presentation is with jaundice due to biliary obstruction. The disease process
results in progressive fibrous stricturing and obliteration of both the intrahepatic and
the extrahepatic bile ducts
The diagnosis is principally based on the findings at cholangiography,in which
irregular, narrowed bile ducts are demonstrated in both the intrahepatic and the
extrahepatic biliary tree .There is no specific treatment that can reverse the ductal
changes, and the patients usually slowly progress to progressive cholestasis and death
from liver failure. There is a strong predisposition to cholangiocarcinoma (CCA),
Primary biliary cirrhosis
As with PSC, the presentation of patients with primary biliary cirrhosis (PBC) is
often hidden, with general malaise, lethargy and pruritus prior to the development of
clinical jaundice or the finding of abnormal liver function tests. The condition is
largely confined to females. Diagnosis is suggested by the finding of circulating anti-
smooth muscle antibodies and, if necessary, is confirmed by liver biopsy. The
mainstay of treatment is liver transplantation,
Caroli’s disease
This is congenital dilatation of the intrahepatic biliary tree, which is often
complicated by the presence of intrahepatic stone formation. Presentation may be
with abdominal pain or sepsis.Imaging is usually diagnostic, with the finding on

ultrasound or CT of intrahepatic biliary lakes containing stones. Liver transplantation
is a radical but definitive treatment.
Simple cystic disease
Radiological findings to suggest that a cyst is simple are
that it is regular, thin walled and unilocular, with no surrounding tissue response and
no variation in density within the cyst cavity. If these criteria are confirmed and the
cyst is asymptomatic, no further tests or treatment are required. Large cysts may be
associated with symptoms of abdominal discomfort possibly related to stretching of
the overlying liver capsule, acute pain associated with haemorrhage in the cyst, or
may present as right upper quadrant abdominal mass. Aspiration of the cyst contents
under radiological guidance provides a sample for culture, microscopy and cytology,
and allows the symptomatic response to cyst drainage to be assessed.
. Laparoscopic deroofing is the treatment of choice for large symptomatic cysts and is
associated with good long-term symptomatic relief.
Polycystic liver disease
This is a congenital abnormality associated with cyst formation within the liver and
often other abdominal organs, principally the pancreas and kidney. Those associated
with renal cysts may have autosomal dominant inheritance. The cysts are often
asymptomatic and incidental findings on ultrasound. They usually have no effect on
organ function and require no specific treatment .
Ascending cholangitis
Ascending bacterial infection of the biliary tract is usually associated with obstruction
and presents with clinical jaundice, rigors and a tender hepatomegaly. The diagnosis
is confirmed by the finding of dilated bile ducts on ultrasound, an obstructive picture
of liver function tests and the isolation of an organism from the blood on culture. The
condition is a medical emergency, and delay in appropriate treatment results in organ
failure secondary to septicaemia. Once the diagnosis has been confirmed, the patient
should be commenced on a first-line broad-spectrum antibiotic and rehydrated, and
arrangements
should be made for urgent endoscopic or percutaneous transhepatic drainage of the
biliary tree. Biliary stone disease is a common predisposing factor, and the causative
ductal stones may be removed at the time of endoscopic cholangiography by
endoscopic sphincterotomy.
Pyogenic liver abscess
The aetiology of a pyogenic liver abscess is unexplained in themajority of patients. It
has an increased incidence in the elderly, diabetics and the immunosuppressed, who
usually present with anorexia, fevers and malaise, accompanied by right upper
quadrant discomfort. The diagnosis is suggested by the finding of a multiloculated
cystic mass on ultrasound or CT scan and is confirmed by aspiration for culture and
sensitivity. The most common organisms are Streptococcus milleri and Escherichia
coli, but other enteric organisms such as S. faecalis, Klebsiella and Proteus vulgaris
also occur, and mixed growths are common. Opportunistic pathogens include
staphylococci.
Treatment is with antibiotics and ultrasound-guided aspiration. First-line antibiotics
to be used are a penicillin, aminoglycoside and metronidazole or a cephalosporin and
metronidazole. Often, repeated aspirations may be necessary.
Amoebic liver abscess
Entamoeba histolytica exists in vegetative form outside the body . it may also present
with an amoebic abscess, the common
sites being paracaecal and in the liver. The amoebic cyst is ingested and develops into
the trophozoite form in the colon,
and then passes through the bowel wall and to the liver via the portal blood.
Diagnosis is by isolation of the parasite from the
liver lesion or the stool and confirming its nature by microscopy.
Often patients with clinical signs of an amoebic abscess will be treated empirically
with metronidazole (400–800 mg, three
times a day, for 7–10 days) and investigated further only if they do not respond.
Resolution of the abscess can be monitored
using ultrasound.
Hydatid liver disease
. The causative tapeworm, Echinococcus granulosus, is present in the dog intestine,
and ova are ingested by humans and pass in the portal blood to the liver. Liver cysts
are often large by the time of presentation with upper abdominal
discomfort or may present after minor abdominal trauma as an acute abdomen due to
rupture of the cyst into the peritoneal cavity. Diagnosis is suggested by the finding of
a multiloculated cyst on ultrasound and is further supported by the finding of a
floating membrane within the cysts on CT scan .
Active cysts contain a large number of smaller daughter cysts, and rupture can result
in these implanting and growing within the peritoneal cavity. Liver cysts can also
rupture through the diaphragm producing an empyema, into the biliary tract
producing obstructive jaundice, or into the stomach. Clinical and radiological
diagnosis can be supported by serology for antibodies to hydatid antigen in the form
of an enzyme-linked immunosorbent assay (ELISA).
Treatment
is

indicated to prevent progressive enlargement and rupture of the cysts. In the first
instance, a course of albendazole or mebendazole may be tried. There are many
reports that percutaneous treatment of hydatid cysts is safe and effective.
Percutaneous treatment constitutes an intial course of albendazole followed by
puncture of the cyst under image guidance, aspiration of the cysts contents,
instillation of hypertonic saline in the cyst cavity and reaspiration (PAIR). PAIR
should only be attempted if there is no communication with the biliary tree. Failure to
respond to medical treatment or percutaneous treatment usually requires surgical
intervention. The surgical options range from liver resection or local excision of the
cysts to deroofing with evacuation of the contents. Contamination of the peritoneal
cavity at the time of surgery with active hydatid daughters should be avoided by
continuing drug therapy with albendazole and adding peroperative praziquantel. This
should be combined with packing of the peritoneal cavity with 20 per cent hypertonic
saline-soaked packs and instilling 20 per cent hypertonic saline into the cyst before it
is opened. A biliary communication should be actively sought and sutured. The
residual cavity may become infected, and this may be reduced, as may bile leakage,
by packing the space with pedicled greater omentum (an omentoplasty). Calcified
cysts may well be dead. If doubt exists as to whether a suspected cyst is active, it can
be followed on ultrasound, as active cysts gradually become larger and more
superficial in the liver. Rupture of daughter hydatids into the biliary tract may result
in obstructive jaundice or acute cholangitis. This may be treated by endoscopic
clearance of the daughter cysts prior to cyst removal from the liver.
Portal Hypertension
The portal venous system contributes approximately 75% of the blood and 72% of the oxygen
supplied to the liver. In the average adult 1000 to 1500 mL/min of portal venous blood is supplied
to the liver. However, this amount can be significantly increased in the cirrhotic patient. The portal
venous system is without valves and drains blood from the spleen, pancreas, gallbladder, and
abdominal portion of the alimentary tract into the liver. The normal portal venous pressure is 5 to 10
mmHg, and at this pressure very little blood is shunted from the portal venous system into the
systemic circulation. As portal venous pressure increases, however, the communications with the
systemic circulation dilate, and a large amount of blood may be shunted around the liver and into
the systemic circulation. Portal Hypertension : direct portal venous pressure that is >5 mmHg
greater than the inferior vena cava (IVC) pressure, a splenic pressure of >15 mmHg, or a portal
venous pressure measured at surgery of >20 mmHg is abnormal and indicates portal hypertension.
A portal pressure of >12 mmHg is necessary for varices to form and subsequently bleed. Ascites
occurs when portal hypertension is particularly high and when hepatic dysfunction is present.
Anorectal varices are present in approximately 45% of cirrhotic patients
.
LIVER TUMOURS
Surgical approaches to resection of liver tumours

Adequate exposure of the liver is an absolute prerequisite to safe liver surgery. A
transverse abdominal incision in the right upper quadrant with a vertical midline
extension to the xiphoid provides excellent access to the liver if adequate retraction of
the costal margin is employed using a costal margin retractor. If necessary,
the incision can be extended across the midline transversely in the left upper
quadrant.
Benign liver tumours
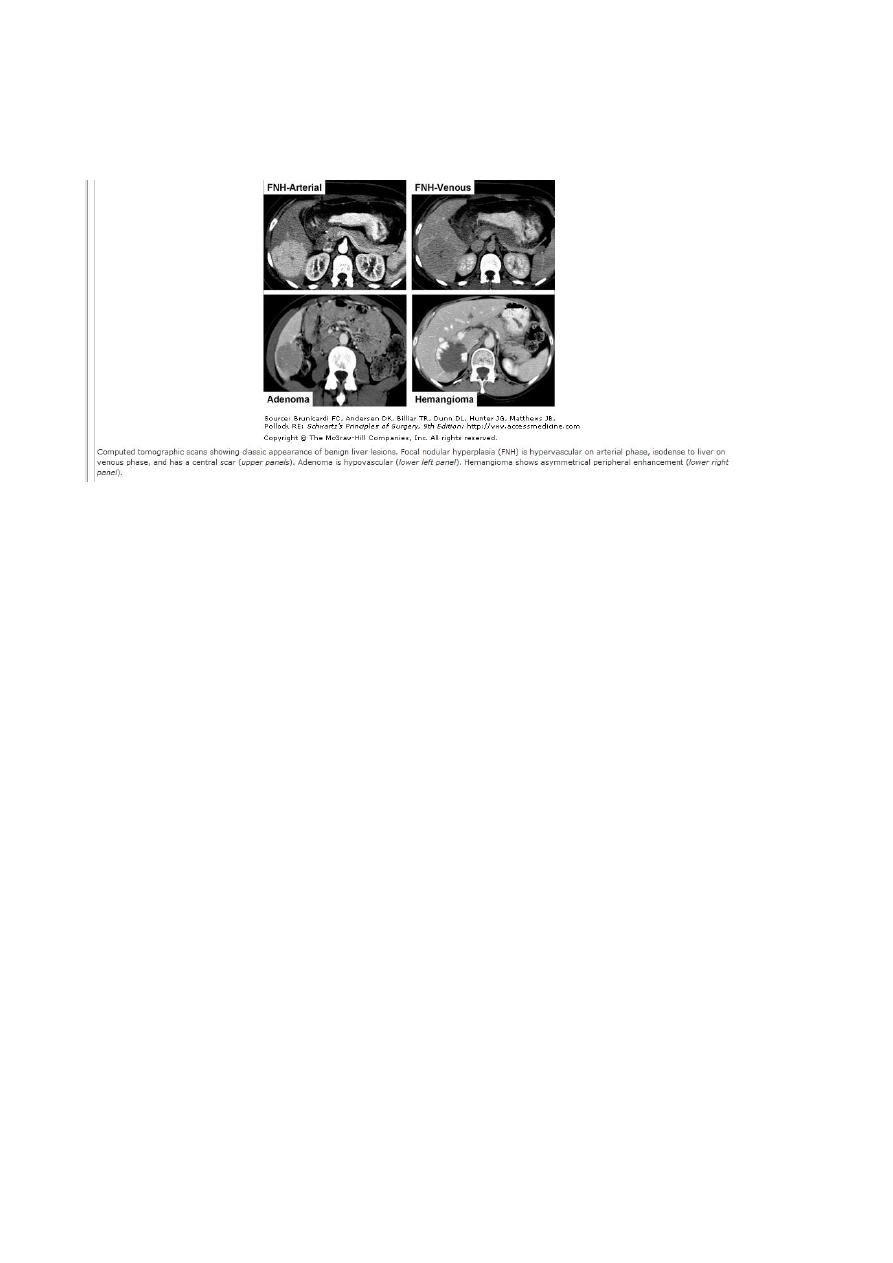
Haemangiomas
These are the most common liver lesions.. They consist of an abnormal plexus of
vessels, and their nature is usually apparent on ultrasound. If diagnostic uncertainty
exists, CT scanning with delayed contrast enhancement shows the characteristic
appearance of slow contrast enhancement due to small vessel uptake in the
haemangioma.Often, haemangiomas are multiple. Lesions found incidentally require
confirmation of their nature and no further treatment.
. Percutaneous biopsy of these lesions should be avoided as they are vascular lesions
and may bleed profusely into the peritoneal cavity.
Hepatic adenoma
. They occur mostly in women of child-bearing age. Imaging byCT or MRI
demonstrates a well-circumscribed and vascular solid tumour. They usually develop
in an otherwise normal liver. Unfortunately, there are no characteristic radiological
features to differentiate these lesions from HCC. An association with sex hormones
(including the oral contraceptive pill) is well recognised, and regression of
symptomatic adenomas on withdrawal of hormone stimulation is well documented.
Focal nodular hyperplasia
This is a focal overgrowth of functioning liver tissue supported by fibrous stroma.
Patients are usually middle-aged
. females, and there is no association with underlying liver disease. Ultrasound shows
a solid tumour mass but does not
help in discrimination. Contrast CT or/and MRI may show central scarring and
evidence of a well-vascularised lesion.
Again, these appearances are not specific for focal nodular hyperplasia (FNH). FNH
contain both hepatocytes and Kupffer
cells. MRI using liver-specific contrast agents, such as gadoxetic acid may be useful
in determining the hepatocellular origin of FNH and allowing differentiation of FNH
from metastatic cancer. FNH do not have any malignant potential and, once the
diagnosis is confirmed, they do not require any treatment
Surgery for liver metastases
.
(b
The resectability rate for liver metastases from colorectal cancer is 20–30 per
cent.The expected patient survival rate for resection of colorectal metastases is
approximately 35 per cent at five years, with few cancer-related deaths beyond this
period. Solitary, multiple unilobar and multiple bilobar liver metastases are all
considered

for resection, although cure rates will vary significantly
)
Staging
This involves defining the extent of the liver involvement with metastases and
excluding extrahepatic disease. A standard work up would involve oral and
intravenous contrast CT scans of the liver and abdomen, chest CT scan and
colonoscopy to look for locally recurrent or synchronous colonic cancers. MRI and
PET scanning are useful in the clarification of equivocal lesions. This information
should be taken in parallel with a general medical evaluation before deciding on the
suitability for surgery of an individual patient.. These patients usually have normal
liver parenchyma and therefore tolerate a 60–70 per cent resection of liver
parenchyma without risk of postoperative liver failure (Summary box 65.13).
Tumour markers are useful but have low specificity. Histological confirmation prior
to undertaking surgery is not necessary and percutaneous biopsy of resectable lesions
should be avoided as there is good evidence that malignant cells can seed along the
biopsy track.
Surgical approach
A search for local recurrent disease, peritoneal deposits and regional lymph node
involvement should be made at the start of the laparotomy. Planar imaging often
overlooks peritoneal or superficial liver metastatic deposits. Coeliac node
involvement in patients with liver metastases considerably reduces the overall
survival whether or not the liver and nodal disease is resected. Intraoperative
ultrasound with bimanual palpation of the liver is valuable in assessing the number
of lesions and resectability.
In patients who cannot be rendered resectable, systemic chemotherapy has been
shown to produce survival and quality of life benefit
Hepatocellular carcinoma
Primary liver cancer (HCC) is one of the world’s most commoncancers, and its
incidence is expected to rise rapidly over the next decade due to the association with
chronic liver disease, particularly HBV and HCV. Many patients known to have
chronic liver disease are now being screened for the development of HCC by serial
ultrasound scans of the liver or serum measurements of alpha-fetoprotein (AFP).
Patients often present in middle age, either because of the symptoms of chronic liver
disease (malaise, weakness, jaundice, ascites, variceal bleed, encephalopathy) or with
the anorexia and weight loss of an advanced cancer. The surgical treatment options
include resection of the tumour and liver transplantation. Which option is most
appropriate for an individual patient depends on the stage of the underlying liver
disease, the size and site of the tumour, the availability of organ transplantation and
the management of the immunosuppressed patient.
(a)
