Oral cavities &Gastrointestinal tract pathologyLec. 3Dr. Zahraa Marwanlecturer in Mosul medical college
SMALL AND LARGE INTESTINES
.SI is about 6 meters in length, first 25 cm is retro-peritoneal, jejunum marks entry of SI into peritoneal cavity.colon is about 1.5 cm, reflection of peritoneum from rectum over pelvic floor form (pouch of Douglas).blood supply
-celiac
-superior mesenteric
-inferior mesenteric
.small intestinal mucosa consists of
-villi, covered by epithelium, which consists of, (columnar absorptive cells, goblet cells, endocrine cells)-crypts of Lieberkun, containing, (stem cells, goblet cells, endocrine cells, Paneth cells)
.colonic mucosa, regain luminal water and electrolytes, it is flat, consists of
-surface epithelium containing, (goblet cells, columnar absorptive cells)-intervening crypts containing, (goblet cells, endocrine cells, and stem cells, Paneth cells are seen at crypt base of cecum and ascending colon only)
Intestinal Immune System.throughout the intestine are mucosal and submucosal nodules of B cells, in the ileum become macroscopically visible as Peyer patches.throughout the intestine T cells form intraepithelial lymphocytes.both B and T cells are called MALT
Meckel Diverticulum:.results from failure of involution of the vitelline duct, which connects the developing gut to the yolk sac.it is true diverticulum with a rule of 2: -incidence is 2% -measuring 2 inches -presents within 2 feet of ileocecal valve -twice as common in male as in female -often symptomatic at 2 years of age -often contain 2 types of mucosa
Meckel diverticulum
.mucosal lining (small intestine, some- times containing heterotopic rests of gastric mucosa or pancreatic tissue).often asymptomatic, symptoms arise: -peptic ulceration due to heterotopic gastric mucosa -intussusception -incarceration -perforation
Malabsorption Syndromes:
.defective absorption and failure to transport nutrients and water, from small intestinal lumen to circulation.clinically presents as chronic diarrhea
(steatorrhea), due to disturbance of: -intraluminal digestion (mouth, stomach small intestine) -terminal digestion (small intestine) -transepithelial transport (small intestine)
.major syndromes: -defective intraluminal digestion -mucosal cell abnormalities -reduced absorptive surface area -lymphatic obstruction -infection
.clinically the hallmark is the passage of bulky, frothy, greasy, yellow or gray stool (steatorrhea) accompanied by: -weight loss -anorexia -abdominal distention, and muscle wasting
Celiac Disease:.immune-mediated (CD8+, CD4+, B cells) enteropathy triggered by ingestion of gluten-containing cereals (wheat, rye, barley), in genetically predisposed individuals .association with other auto-immune diseases
.morphology: -intraepithelial lymphocytosis -crypt hyperplasia -villous atrophy (biopsy is taken from second part of duodenum or proximal jejunum) .complicated by: -T-cell lymphoma -small cell adenocarcinoma
.clinical features: -infants, 6-24 months: (diarrhea and failure to thrive) -children, non-classic symptoms: (abdominal, nausea, vomiting) -adults, 30-60 years: .silent celiac (asymptomatic, villous atrophy, positive serology) .latent celiac (asymptomatic, no villous atrophy, positive serology) .symptomatic (diarrhea, flatulence, weight loss, fatigue)
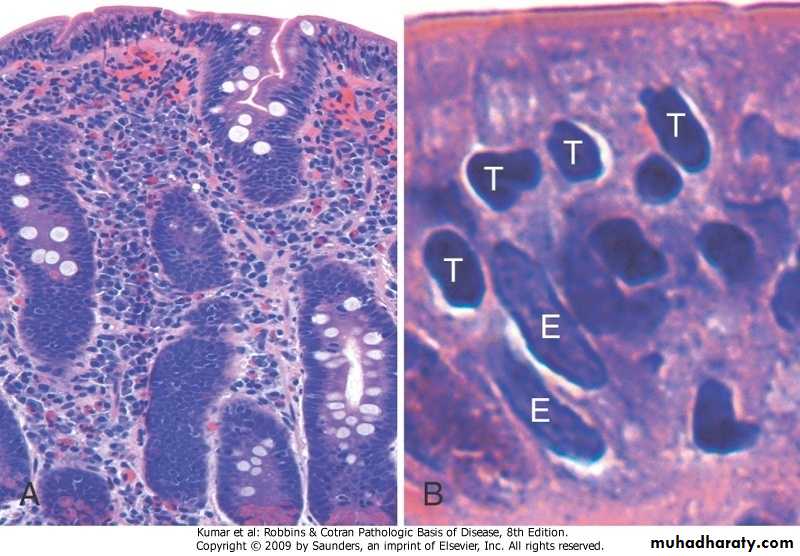
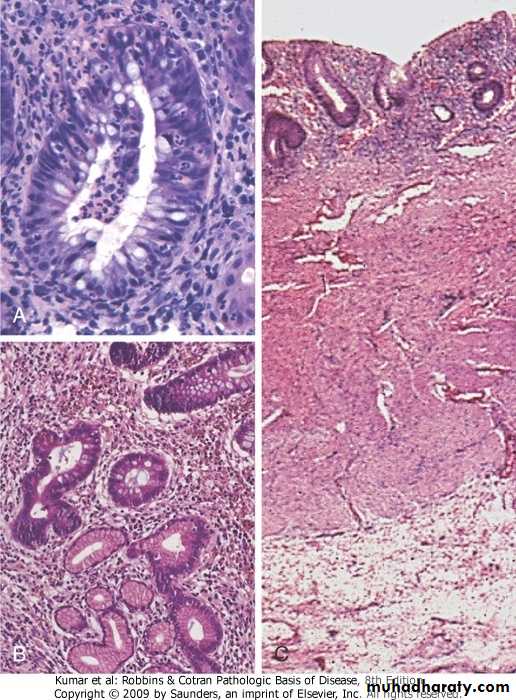
Celiac disease. (A) Advanced cases of celiac disease show complete loss of villi, or total villous atrophy. Note the dense plasma cell infiltrates in the lamina propria. (B) Infiltration of the surface epithelium by T lymphocytes, which can be recognized by their densely stained nuclei (labele T). Compare with elongated, pale-staining epithelial nuclein(labeled E).
.diagnosis depends on: -clinical features -histopathological changes -clinical and histopathological improvement on gluten-free diet -serologic tests: .IgA against transglutaminase .IgA or IgG against gliadin .Antibodies against endomysium is more specific but less sensitive
Enterocolitis:
Diarrhea And Dysentery.diarrhea is an increase in stool mass stool frequency, and/or stool fluidity
greater than 200 g per day,associated with pain, urgency, perianal discomfort, and incontinence
.dysentery is low-volume, painful, bloody diarrhea
Infectious Entero-Colitis:
.Viral gastro-enteritis, mucosa shows lymphocytic infiltration.Bacterial entero-colitis (food poisoning), mechanisms of bacterial:
1-ingestion of preformed toxins, symptoms appear within hours,
(Staphylococcus aureus, Vibrio cholera
Clostridia)
2-infection with toxigenic organisms, which proliferate within gut lumen and elaborate an endotoxin
3-infection with entero-invasive organisms, which proliferate, invade, and destroy epithelium
.Parasitic infection
.Helminthic infestation
Pseudomembranous Colitis:
.acute colitis, usually follows use of broad-spectrum antibiotics, especially elderly and hospitalized patients.etiology
-toxins of C. difficile (most common)
-Salmonella
-C. perfringens
-Staphylococcus aureus
.Pathogenesis: -antiobiotic>disruption of normal colonic flora>overgrowth of C. difficile -immunosuppression>C. difficile colitis.Morphology: -formation of exudate (pseudo- membrane) overlying mucosal injury .Diagnosis: -fecal detection of C. difficile cytotoxin -histopathology support
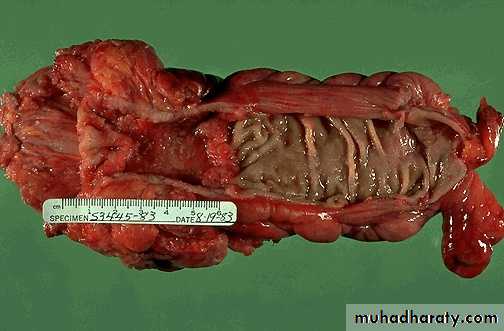
Pseudomembranous enterocolitis.
The mucosal surface of the colon seen here is hyperemic and is partially covered by a yellow-green exudate. The mucosa itself is not eroded. It is due to overgrowth of bacteria such as Clostridium dificile or S. aureusMicroscopically, the pseudomembrane is seen to be composed of inflammatory cells, necrotic epithelium, and mucus in which the overgrowth of microorganisms takes place. The underlying mucosa shows congested vessels, but is still intact
Inflammatory Bowel Disease:
.Remitting relapsing inflammation resulting from inappropriate mucosal immune activation..Includes: -Crohn’s disease -ulcerative colitis
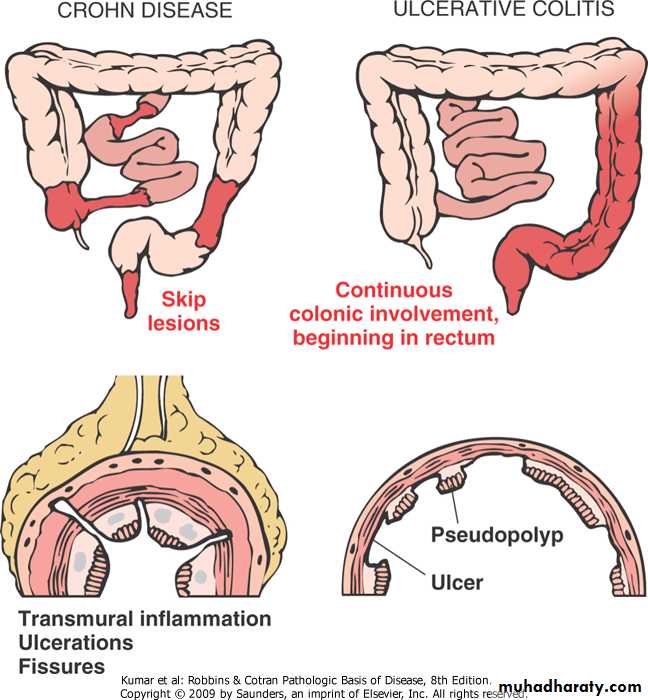
Inflammatory bowel disease
.Epidemiolgy: -more common in females -affects teens and early twenties .Pathogenesis: -results from a combination of 1.defects in host interactions with intestinal microbiota 2.intestinal epithelial dysfunction 3.aberrant mucosal immune response
4.transepithelial influx of luminal bacterial components activates innate and adaptive immune responses5.in genetically susceptible host, the subsequent release of TNF and other immune-mediated signals direct epithelia to increase tight junction permeability, which causes further increases in the influx of luminal material
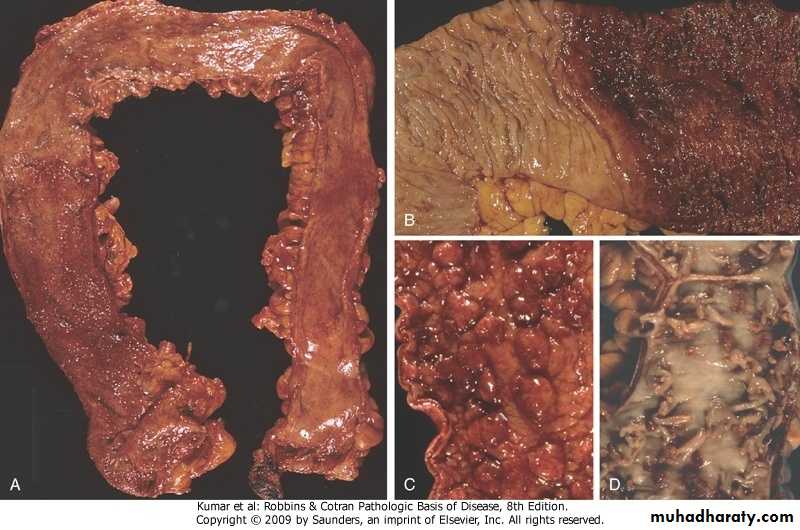
Crohn’s Disease: .involvement of -terminal ileum, ileocecal valve, cecum -delimited (skip lesions) and trans- mural involvement of the bowel wall.gross, ulcer, cobblestone, fissuring, fistulae, creeping fat.microscopy, crypt abscess, distortion of mucosal architecture, paneth cell metaplasia, noncaseating granulomas, metastatic Crohn disease
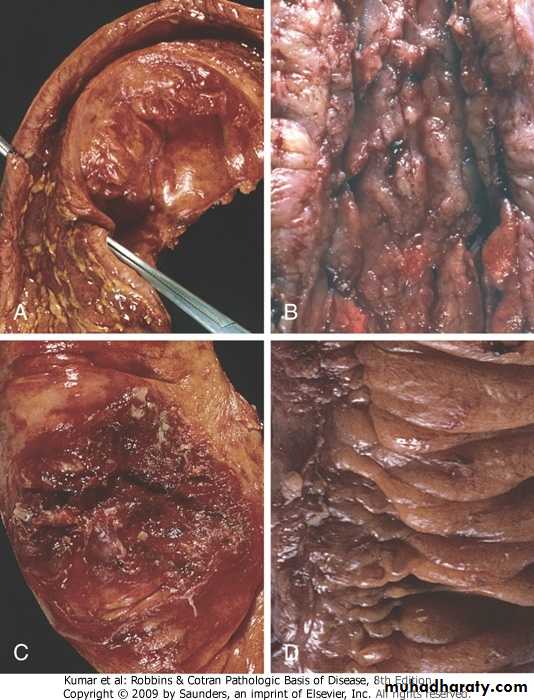
Crohn’s disease, S-I stricture, linear mucosal ulcers, perforation with serositis, creeping fat
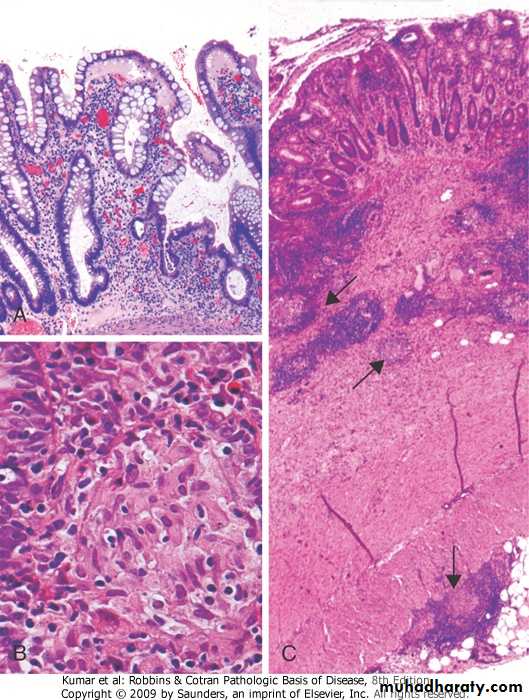
Crohn’s disease, disorganized crypts,noncaseating granuloma, transmural involvement
.Clinical features: -intermittent attacks, of mild diarrhea, fever, and abdominal pain -chronic occult or overt fecal blood loss leads to anemia -in 1/5 of patients onset is abrupt (acute abdominal pain, fever, and diarrhea)
.Complications -fibrosing strictures -fistulas to loops of bowel, urinary bladder, vagina, or perianal skin -perforation to peritoneum -malabsorption syndrome -increased incidence of cancer of the gastrointestinal tract
Ulcerative Colitis: .left-sided colitis, proctitis, procto- sigmoiditis, backwash ileitis .toxic megacolon (damage to muscularis propria and neural plexus) .gross, broad-based ulcers, pseudo- polyps, mucosal bridges .microscopy, mucosal atrophy, diffuse inflammation limited to mucosa and submucosa
Ulcerative colitis, pancolitis, inflammatory polyps, mucosal bridges
Ulcerative colitis, crypt abscess, pseudopyloric metaplasia, mucosal involvement only
.clinical features:
-chronic remitting relapsing condition marked by attacks, of bloody mucoid diarrhea that may persist for days, weeks, or months-may have an explosive onset as a medical emergency -long-term complication is cancer of colon
Polyps:.most common in the colon, grossly -sessile -pedunculated.types -inflammatory -hamartomatous -hyperplastic -neoplastic
Neoplastic Polyps (Adenomas): .small pedunculated to large sessile .based on epithelial architecture, 3 subtypes are recognized; -tubular adenomas, (most common) -villous adenomas, (least common) -tubulovillous adenomas.all adenomas have dysplasia (low- grade, high-grade, carcinoma in situ) .malignant risk is correlated with; -type, size, site and number of polyp(s) -severity of dysplasia -duration (10 years)
.clinical features -asymptomatic (most of them) -occult rectal bleeding>anemia -villous adenomas may cause hypo- proteinemic hypokalemia
Multiple nodules of different sizes attached to colonic mucosa by a stalkDiagnosis: adenomatous polyp
Colorectal Carcinomas:.most common malignancy of GI tract .epidemiology and etiology; -peak incidence is 7th-8th decade, slightly more in males -predisposing factors include, .genetic factors .environmental factors, (diet with high fat, high refined carbohydrate, low fiber content and deficient in vitamins A, C, and D)
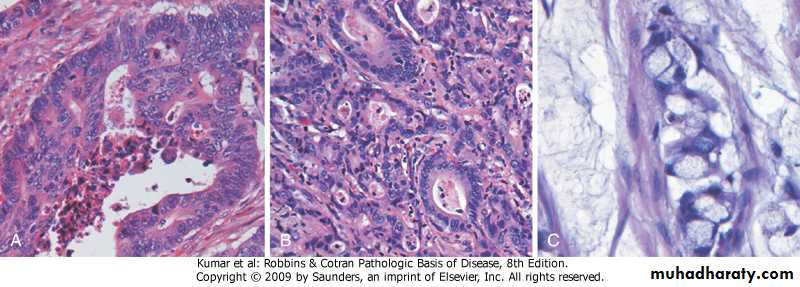
.morphology:
-distributed equally over the entire length of the colon-tumors at proximal colon are polypoid, (rarely obstructive), and those of distal colon are annular (obstructive) -differentiation varies -some tumor cells produce abundant extracellular mucin, others have signet-ring appearance, or neuro- endocrine differentiation
Carcinoma –colon, there is a heaped up margin of tumor at each side with a central area of ulceration.
Colorectal carcinoma, well differentiated, poorly differentiated, mucinous (signet ring)
.clinical course: -right colonic cancers (weakness and fatigue, due to iron-deficiency anemia) -left-sided carcinomas (occult bleeding, change in bowel habit, left-sided abdominal pain) -most important prognostic indicator is stage of tumor at time of diagnosis
.TNM staging system
-Tis (confined to mucosa)-T1 (involving mucosa and submucosa)
-T2 (involving full-wall thickness)
-T3 (invading extracolonic tissue)
-No (no regional LNs metastasis) -N1 (metastasis in up to 3 LNs) -N2 (metastasis in more than 3 LNs) -Mo (no distant metastasis) -M1 (distant metastasis)