THE THERAPY OF HYPERTENSION
(Anti-hypertensive drugs)Dr. Faehaa
Assistant professor of pharmacology
Hypertension: is a multifactorial disease,
characterized by elevated systolic &/ or diastolic arterial blood pressure above normal on repeated measurements.CLASSIFICATION OF BLOOD PRESSURE IN ADULTS
SBP (mmHg) DBP (mmHg)Normal < 120 < 80
Prehypertension 120-139 80-89
Stage 1 140-159 90-99
Stage 2 ≥ 160 ≥ 100
Classification
• Essential hypertension: sustained, elevated blood pressure for which no cause is apparent.• Secondary hypertension: results from known disorder, such as renal and vascular disease.
THE MANAGEMENT OF Hypertension
There are over 100 drug products that are available for the treatment of hypertension.
In addition to drugs used to lower blood pressure, life-style modifications can also decrease blood pressure.
Angiotensin Converting Enzyme (ACE) Inhibitors and Angiotensin (AT1)-Receptor Antagonists.
ACE inhibitors( Captopril, & Enalapril) and AT1- receptor antagonists (Losartan ) are agents for the treatment of hypertension.
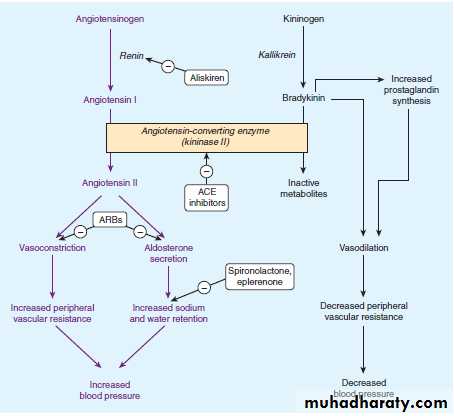
Mechanism of action
The ACE inhibitors lower blood pressure by reducing peripheral vascular resistance without increasing cardiac output, rate, or contractility.These drugs block the ACE that cleaves angiotensin I to form the potent vasoconstrictor, angiotensin II .
These inhibitors also diminish the rate of bradykinin inactivation.
Vasodilation occurs as a result of the combined effects of lower vasoconstriction caused by diminished levels of angiotensin II and the potent vasodilating effect of increased bradykinin.Side Effects
dry cough.Rashes.
Fever.
Altered taste or loss of taste.
Hypotension (in hypovolemic states) .
Hyperkalemia.
Calcium Channel Blockers
Calcium channel blockers are recommended when other agents are contraindicated or ineffective.
Mechanism of Action
Calcium channel antagonists block the inward movement of calcium by binding to L-type calcium channels in the heart and in smooth muscle of the coronary and peripheral vasculature.This causes vascular smooth muscle to relax, dilating mainly arterioles.
Classes of calcium channel blockers
The calcium channel blockers are divided into :three chemical classes, each with different pharmacokinetic properties and clinical indications.Benzothiazepines: Diltiazem
Diphenylalkylamines: Verapamil
Dihydropyridines: nifedipine , amlodipine, isradipine, nicardipine.
Side Effects
• Headache.• Flushing.
• Dizziness.
• Palpitations.
• Hypotension may occur during the first few hours after dosing.
• Ankle edema also develop. This is due to a rise in intracapillary pressure as a result of the selective vasodilatation by calcium blockers.
• The edema is not a sign of Na+ retention. It is not therefore relieved by diuretics but disappears after lying flat (e.g. overnight).
• Bradycardia and dysrhythmia may occur.
• Gastrointestinal effects include constipation, nausea and vomiting; palpitation and lethargy may be felt.
Beta Blockers
These drugs have diverse effects on cardiovascular function and have a variety of cardiovascular and non cardiovascular uses.Mechanism of Action
The β-blockers reduce blood pressure primarily by decreasing cardiac outputClasses of Beta Blockers
There are selective and nonselective beta blockersThe prototype β-blocker is propranolol, which acts at both β1- and β2 receptors.
Newer agents, such as atenolol and metoprolol, are selective for β1 receptors.
Therapeutic uses
• Subsets of the hypertensive population: The β-blockers are more effective for treating hypertension in white than in black patients, and in young patients compared to the elderly.Therapeutic uses
• Hypertensive patients with concomitant diseases: The β-blockers are useful in treating conditions that may coexist with hypertension, such as supraventricular tachyarrhythmia, previous myocardial infarction, angina pectoris, glaucoma (applied topically), and migraine headache.Side Effects
Common effects: The β -blockers may cause CNS side effects such as fatigue, lethargy, insomnia, and hallucinations; these drugs can also cause hypotension.
Alterations in serum lipid patterns: The β-blockers may disturb lipid metabolism, decreasing high-density lipoproteins (HDL) and increasing plasma triacylglycerol.
Side Effects
Drug withdrawal: Abrupt withdrawal may cause rebound hypertension, probably as a result of up-regulation of β-receptors.Patients should be tapered off of β1-blocker therapy in order to avoid precipitation of arrhythmias.
Side Effects
The β-blockers should be avoided in treating patients with asthma, congestive heart failure, and peripheral vascular disease.α -ADRENERGIC BLOCKING AGENTS
Prazosin, oxazosin and terazosin produce a competitive block of α1 adrenoceptors.They decrease peripheral vascular resistance and lower arterial blood pressure by causing the relaxation of both arterial and venous smooth muscle.
α -ADRENERGIC BLOCKING AGENTS
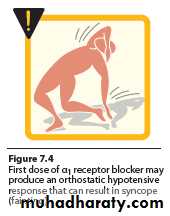
These drugs cause only minimal change in cardiac output, renal blood flow, and glomerular filtration rate.Postural hypotension is the most common side effect.
Prazosin
Prazosin is used to treat mild to moderate hypertension and is prescribed in combination with propranolol or a diuretic for additive effects.
Reflex tachycardia and first dose syncope are almost universal adverse effects.
VASODILATORS
. VASODILATORSThe direct-acting smooth muscle relaxants, such as hydralazine and minoxidil, have traditionally not been used as primary drugs to treat hypertension.
. VASODILATORS
Vasodilators act by producing relaxation of vascular smooth muscle, which decreases resistance and therefore decreases blood pressure.These agents produce reflex stimulation of the heart, resulting in the competing symptoms of increased myocardial contractility, heart rate, and oxygen consumption.
A. Hydralazine
This drug causes direct vasodilatation, acting primarily on arteries and arterioles.This results in a decreased peripheral resistance, which in turn prompts a reflex elevation in heart rate and cardiac output.
B. Minoxidil
This drug causes dilation of resistance vessels (arterioles) but not of capacitance vessels (venules).
Implications for Dentistry
Because there are several categories of antihypertensive drugs (each class having a different mechanism of action), there are numerous possibilities for drug interactions. Aspirin and other nonsteroidal antiinflammatory drugs (NSAIDs) antagonize many antihypertensive drugs. The antihypertensive effects are reduced by aspirin. In addition, the effect of diuretics is inhibited by NSAIDs. This interaction apparently results from the inhibitory effect of chronic (>5 days) NSAID therapy on prostaglandin synthesis. Prostaglandins are important in maintaining renal blood flow and urine output. NSAIDs also reduce the antihypertensive effect of β blockers. Patients should be advised of this drug interaction; in the event that blood pressure control is lost, substitution with acetaminophen with or without opioid supplementation is advised for pain.
In general, the use of vasoconstrictors in local anesthesia is not contraindicated in hypertensive patients, especially in patients whoseblood pressure is well controlled. A possible exception to this statementis a patient receiving an adrenergic neuron–blocking or adrenergic neuron–depleting drug, such as guanethidine, or a nonselective β-adrenergic receptor–blocking drug such as propranolol.
Long term use of guanethidine-related drugs produces supersensitivity tothe actions of exogenously administered catecholamines. Use of vasoconstrictors in local anesthetic solutions could possibly lead to serious disturbances of blood pressure and cardiac rhythm. Nonselective β-adrenergic receptor blockers preventthe decrease in peripheral vascular resistance normally caused bydoses of epinephrine used in local anesthesia. Unopposed α-agonisticaction may lead to an acute hypertensive episode. To avoid potentialcomplications, the blood pressure of a patient on any of these medicationsshould be taken before and 5 minutes after the injection of a smallamount of local anesthetic (e.g., 1 mL of 2% lidocaine with 1:100,000epinephrine). If no significant reaction is observed, dangerous hypertensiveresponses to additional local anesthetic are unlikely.
The use of epinephrine-impregnated retraction cord is contraindicated in patients with compromised cardiovascular function, including hypertensive patients. Significant amounts of epinephrine can be absorbed, especially if the gingiva is abraded or multiple teeth are involved.
Although not widely used, centrally acting sympatholytics,which have a sedative side effect, are important to the dentist.In dealing with patients taking these drugs, the dentist must proceed cautiously when using antianxiety agents or other drugs that depress the CNS. In combination with antihypertensives with sedative side effects, these agents may lead to excessive CNS depression. Use of a smaller dose is advised in the premedication of a patient taking methyldopa, clonidine, guanabenz, or guanfacine for hypertension.
One adverse effect of significance to the dentist that is associated with antihypertensive medication is orthostatic, or postural, hypotension.After being in a supine position, many patients receiving antihypertensivetherapy may be unable to compensate adequately for a suddenchange in position. Such patients should be observed carefullyat the end of dental appointments. Drugs affecting peripheral adrenergic transmission are most likely to cause orthostatic hypotension, although other drugs may also have this action.
Another adverse effect that has implications in dentistry is inhibition of salivary secretion leading to dry mouth. Xerostomia is especially common in patients medicated with centrally acting antihypertensive agents (methyldopa, clonidine, guanabenz, and guanfacine).