Fifth Stage
E.N.T
Dr.Mushtaq – Lecture 16
1
Upper Airways Obstruction
Assess
Look / Listen / Feel
(Anytime)
*Degree of obstruction
*Site of Obstruction
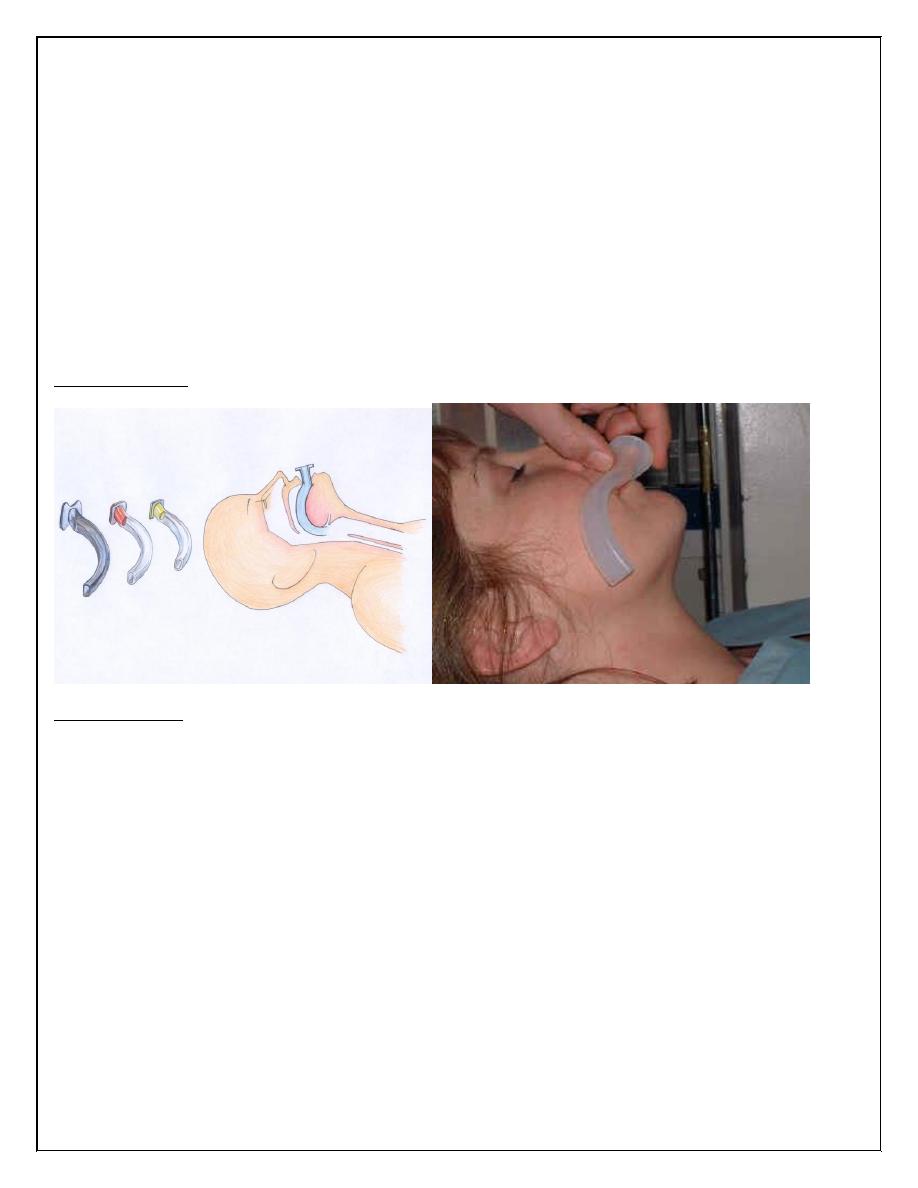
Guedel Airway:
Tracheostomy:
Indications
1. Relief of respiratory obstruction above upper tracheal level. causes:
Congenital
· Bilateral choanal atresia. · Laryngeal web or cyst
· Upper tracheal stenosis. · Tracheo-oesophageal anomalies.
Traumatic
· External /· Internal (1) Inhalation of steam or irritating fumes.
(2) Foreign bodies.
(3) Swallowing of corrosives.
2
Infections
· Acute laryngotracheobronchitis. · Acute epiglottitis.
· Diphtheria. · Ludwig's angina.
Tumors
Tongue, pharynx, larynx, upper trachea and thyroid gland. Miscellaneous : Haemophilia,
Angioneurotic oedema.
Bilateral laryngeal nerve palsies;after thyroidectomy &
with bulbar palsy
Cord fixation due to rheumatoid arthritis.
2. Protection of tracheobronchial tree.
Inhalation & Stagnation
· Bulbar poliomyelitis.
· Polyneuritis.
· Tetanus.
· Myasthenia gravis.
· Coma due to many causes (including head
injuries, drug overdose and cardiac arrest).
· Cervical cord lesions and injuries.
· Burns of face and neck.
· Multiple fractures of mandible.
3. Treatment of conditions leading to respiratory insufficiency.
Any of (1) and (2)
* Pulmonary disease
· Chronic bronchitis and emphysema.
. Postoperative pneumonia.
*Severe chest injuries ('flail chest')
3
*Neuromuscular incoordination,
. Leading to (2) above.
· Needing artificial or intermittent positive-pressure respiration
(IPPR).
Tracheostomy aids respiration by:
1. Reducing the 'dead space' (lips to tracheostome) by about 50%.
2. By-passing resistance to airflow in nose, mouth and glottis.
3. Allowing easy bronchi 'toilet‘.
4. Use of mechanically assisted respiration.
Criteria for intervention
Inspiratory stridor, recession of the suprasternal notch and intercostal spaces, and with
anxious, pale. Sweaty face, operation must not be delayed.
Cyanosis indicates a late and grave stage.
*-With paralyzing disease and normal lungs;
if the vital capacity falls to a quarter of normal or if with deep breath, the patient can count
only to 20 and not to 60.
* With pulmonary disease;
if patient loses consciousness or PCO exceeds 70 mmHg.(35-45mmhg)
* With crushed chest;
clinical judgment is usually sufficient, but PC02 measurement is valuable.
In real urgency
Without proper facilities and training, a laryngotomy must be performed.
With well trained & skilled staff of RCU , endotracheal tube may be a best solution .
4
Emergency tracheostomy
1. Anaesthesia
Best intubation & G.A, but usually infiltration
with lignocaine 0.5 %.
2. Position
Head extended in supine position.
3. Incision
Midline vertical, from lower border of thyroid
cartilage to manubrium of sternum
Cricoid cartilage is the guide and felt with the
left index finger.
4. Midline separation of strap muscles with
scissors.
5. Trachea exposed and opened
Circular cut at level of third ring (2
nd
-4
th
).
The first ring must never be divided.
In children a vertical incision is used .
6. Insertion of tube
A suitable tube is inserted and firmly secured by tapes
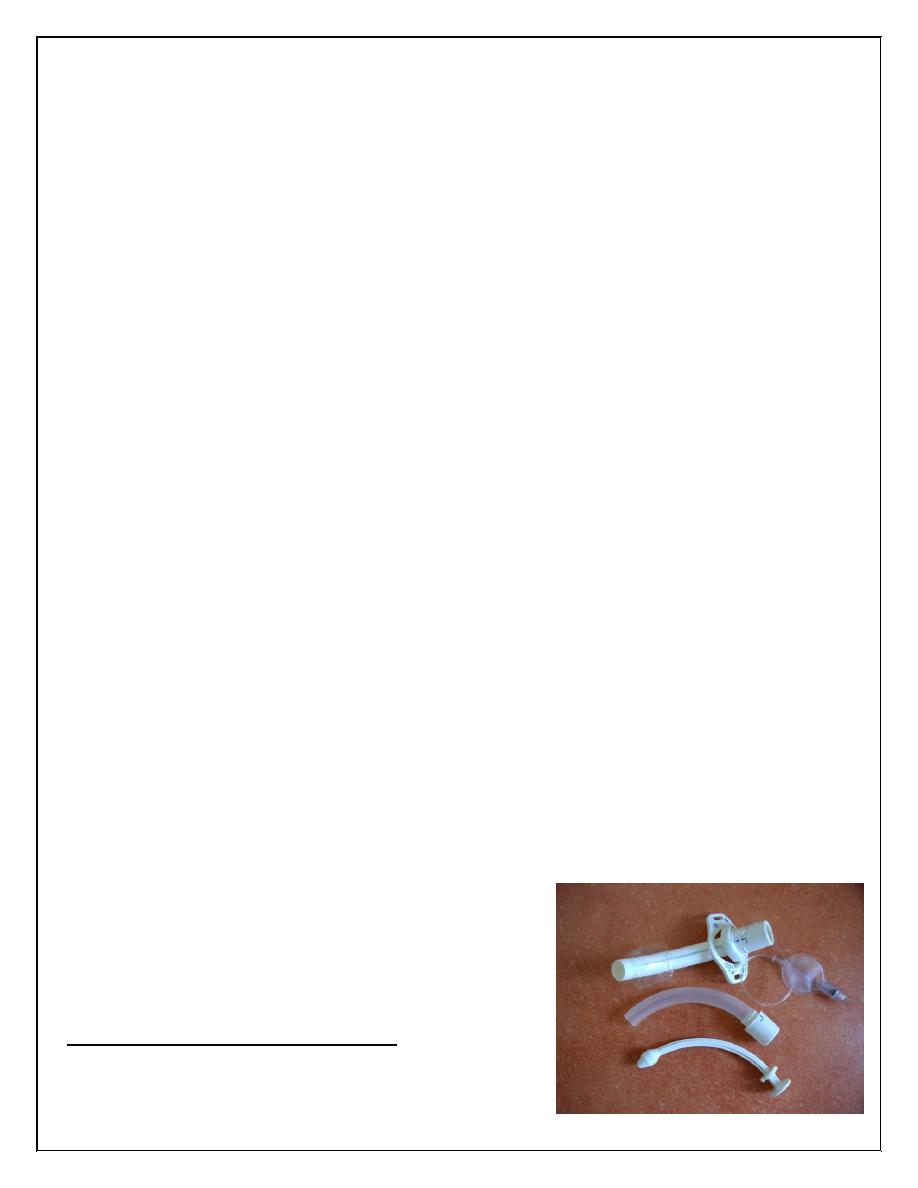
7. Choice of tube
The best type is a cuffed plastic (Portex) tube, but a
silver tube may be preferred in early operation time
because of inner tube .
8. Closure of wound
Ligation of bleeding points is essential. The wound
isloosely closed, for fear of emphysema.
5
Postoperative management
1. Nursing is essential for the first 24 h at least including chart of follow up.
2. Position sitting upright in bed.
3. Suction regularly, with aseptic technique, passing a sterile catheter into trachea and main
bronchi.
4. Humidification is essential, using humidifier or moistened gauze over the tracheostomy
tube.
5. Prevention of crusting by irrigation with N/S & suction
6. Prevention of apnea
In cases of long-standing obstruction, apnea may occur immediately after opening of trachea,
caused by sudden cleaning of the C02.
Carbon dioxide (5-7% in oxygen) is given via flow-meter through the tracheostome if this
occurs.
7. Care of tube
Metal type . The inner tube is taken out and cleaned hourly at first day . the outer tube must
be held firmly while withdrawing the inner one.
Cuffed plastic tubes ;
The cuff should be of adequate length and not inflated too much, to avoid pressure necrosis
of tracheal mucosa, necessity of periodic deflation of cuff : 5/60 minutes
Low-pressure high volume cuffed tubes or double-cuffed type must always be employed, to
minimize the risk of tracheal stenosis.
8. Decannulation
The tube is removed when the patient is comfortable with its corked off.
Difficulty occurs. especially with children. if the tracheostomy has been present for a long
time. Gradual reduction in the size of tube, then sealing off
Complications
A.Early
1.Apnoea
2. Haemorrhage
6
May occur if haemostasis is not secured at operation or ulceration by the tip of the tube if of
the wrong shape.
3. Displacement of tube
If complete it must be reinserted at once after the wound and tracheal opening are adequately
dilated.
Partial dislodgement may pass unobserved for a time, with the tube lying just in front of the
tracheal opening.
4. Surgical emphysema and pneumothorax
A- More common in children.
B- If tracheostomy is too low.
C- If wound closed tightly.
D- If tissue planes are dissected too much.
E- Under L.A more than G.A .
F- Adminstration of high pressure O2
5. Syncope &Cardiac arrest
Manipulation of sucker catheter
B. Late
1. Local sepsis; septicemia.
2. Perichondritis and stenosis
a. May develop in the subglottic region if the
tracheostome is too high
a smaller tube, of non-irritating Portex, may help .
b. A stricture above a well-placed trache-ostome may result from trauma by an ill-fitting
tube or a small opening .
c. A low tracheal stricture may be a late sequel of prolonged over-inflation of a cuffed tube.
3.Tracheo-oesphageal fistula
Due to pressure of an ill-fitting tube against the posterior wall.
Thank you,,,
