
Dr.Nazzal Jabr
Anesthesia
Lec.3
Starting Anesthesia
Every patient undergoing general, regional, or monitored anaesthesia requires the following when
arrive to the operating room:
1. A safe transfer from their bed to the operating room table.
2. An anaesthetic record.
3. Monitors attached including an ECG, blood pressure cuff, and pulse oximeter to start with.
4. Establish an intravenous access.
5.
Record the patients initial vital signs on the anaesthesia record.
Monitoring
Current Canadian guidelines to the Practice of Anaesthesia and patient monitoring are:
1. An anaesthetist present: "The only indispensable monitor is the presence at all times, of an
appropriately trained and experienced physician.
2. A completed preanaesthetic checklist used to ensure that you are ready when the patient
arrives to the operating room. There are many ways anaesthetists ensure that everything is
checked and ready to proceed safely with anaesthesia.
3. An anaesthetic record: Every patient should have their
A. HR and BP measured at least every 5 minutes.
B. The time, dose, and route of all drugs and fluids should be charted.
4- Oxygenation, ventilation, circulation, and temperature are continually evaluated both
clinically and quantitatively.(Continual is defined as 'repeated regularly').
Types of Intraoperative Monitoring
There are two main types of Intraoperative Monitoring:
1- Non-invasive monitores:
A- Pulse Oximetry :
Pulse oximetry allows beat-to-beat analysis of the patient's oxygenation status.
It is also used for pulse rate measurement.
B- End-Tidal CO2 Monltorlng (Capnography) :
Is the continuous monitoring of a patient's capnogram (the CO2 concentration sampled from
the patient's airway during ventilation).
End-tidal CO monitoring is standard for all patients undergoing general anaesthesia with
mechanical ventilation.
Capnography is able to provide the following:
1- Confirmation of tracheal intubation.
2- Recognition of an inadvertent esophageal intubation.
3- Recognition of an inadvertent extubation or disconnection.
4- Assessment of the adequacy of ventilation and an indirect estimate of PaCO2.
5- Aids the diagnosis of a pulmonary embolism (e.g., air or clot).

Dr.Nazzal Jabr
Anesthesia
Lec.3
6- Aids the recognition of a partial airway obstruction (e.g., kinked ETT).
7- Indirect measurement of airway reactivity (eg., bronchospasm).
8- Assessment of the effect of cardiopulmonary resuscitation efforts.
C- ECG:
A three or five lead electrode system used for ECG monitoring in the operating room. Lead II
usually monitored with a three lead system, and it is useful in distinguishing a sinus rhythm
from other rhythms. V5 precordial lead also monitored and useful for ischemic changed
detection.
A five lead electrode system allows monitoring of vectors I, II, III, AVR, AVL, AVF and V5. Over
85% of ischemic events occurring in the left ventricle during surgery can be detected by
monitoring the ST segments of leads II and V5.
D- Automated non-invasive BP measurements:
It is routinely performed intraoperatively. Rapid, accurate (+ 9 mmHg) measurements of SBP,
DBP, and MAP can be obtained several times a minute. Blood pressure determinations during
anesthesia aid drug titration and fluid management and provide warning of conditions that
could affect patient safety.
E- Temperature:
A temperature monitor must be readily available to continuously measure temperature.
Temperature monitoring is mandatory if changes in temperature are anticipated or
suspected.
2- Invasive monitoring of the circulation :
A-
Arterial catheter:
Used for beat-to-beat measurement of BP and for arterial blood gas sampling (ABG)
Indications include:
1-
Major cardiac, thoracic, vascular and neurosurgical procedures.
2-
Procedures requiring induced hypotension or induced hypothermia.
3-
Patients with co-existing diseases, including significant cardiopulmonary disease, severe
metabolic abnormalities.
4-
Morbid obesity
5-
Major trauma.
B-
Central venous catheter:
A central venous pressure (CVP) catheter provides an estimate of the right atrial and
right ventricular pressures.
The CVP reflects the patients' blood volume, venous tone, and right ventricular
performance.
Indications:
1- Patients undergoing procedures associated with large fluid volume shifts
2- Shock states
3- Massive trauma
4- Significant cardiopulmonary disease
5- The need for vasoactive medications

Dr.Nazzal Jabr
Anesthesia
Lec.3
C-
Pulmonary artery catheter:
It passes through the right atrium and right ventricle and rests in a branch of one of the
pulmonary arteries for measurement of the pulmonary artery wedge pressure (PCWP)
which reflects the left atrial filling pressure.
Detailed analysis of the patient's blood and fluid requirements, as well as the adequacy
of oxygen transport can be made with the measurements obtained from a PA catheter.
The results of manipulating the patient's hemodynamic parameters with ionotropic
agents, vasopressors, vasodilators, diuretics, fluids or blood products, can then be
followed.
General Anesthesia
It is a reversible loss of conscious with whole body (general) analgesia, element of amnesia with or
without muscle relaxation.
Components of general anesthesia
• Unconsciousness (Hypnosis)
• Analgesia (Areflexia)
• Muscle relaxation
Stages of general anesthesia
Stage I : Analgesia
From induction of anesthesia to loss of consciousness (loss of eyelid reflex).
Stage II : Excitement
Excitation, Pupils dilated and eyes divergent, Agitation, delirium, irregular respiration, and
breatholding. Potentially dangerous responses can occur during this stage including vomiting,
laryngospasm, HTN, tachycardia, and uncontrolled movement.
Stage III : Surgical anesthesia
Central gaze,constricted pupils, and regular respirations, and combined of 4 planes.
Stage IV : Impending Death/Overdose
Onset of apnea, dilated and nonreactive pupils, and hypotension to complete circulatory failure.
Dr.Nazzal Jabr
Anesthesia
Lec.3
Anaesthetic Strategies
Induction of anaesthesia
Maintenance of anesthesia
Recovery from anesthesia
Induction of anaesthesia:
Induction is the process that produces a state of surgical anaesthesia in a patient. This term is used
only in the context of general anaesthesia and not with local anaesthesia.
It is the first step in the process of anaesthesia whereby the patient is rendered unconscious,
preventing both awareness of, and response to, surgical stimuli.
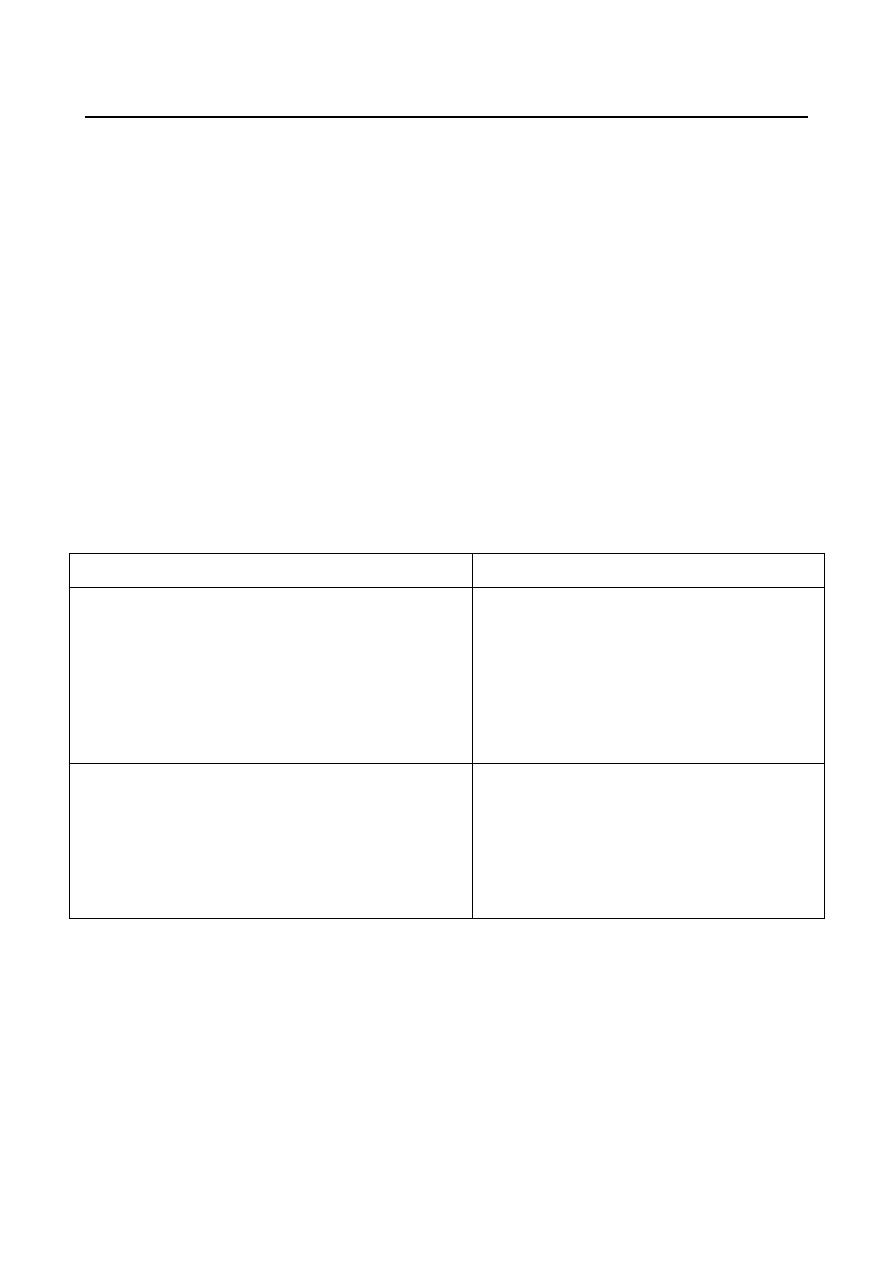
Induction methods
Most anaesthetic inductions are performed using intravenous or inhalational (‘gas’) induction; each
has advantages and disadvantages as below:
Intravenous
inhalational
Advantage
1- Rapid onset
2- Patient comfort
3- Depression of pharyngeal reflexes allows
early insertion of LMA
4- Airway protection in rapid-sequence
induction
Advantages
1- Does not require IV access (Useful
for patient with needle-phobia)
2- useful in pediatrics
3- Respiration is maintained
4- Upper oesophageal sphincter tone
maintained
Disadvantage
1- Venous access required
2- Risk of hypotension
3- Apnea common
4-Loss of airway control
5- Anaphylaxis
Disadvantage
1- Slow process
2- Potential excitement phase
3- Irritant and unpleasant, may induce
coughing
4- Pollution
5- May cause a rise in ICP/IOP
Intravenous induction
Steps of Intravenous induction
Pulse oximetry and ECG monitoring should be established before intravenous access because
occasionally a cardiovascular event (e.g. vasovagal syncope) occurs during cannulation.
Intravascular access commonly consists of a simple venous cannula; however, complex cases
may require an arterial line, a central venous line and/or a pulmonary artery catheter.
Pre-oxygenation: some anaesthetists routinely pre-oxygenate their patients before induction.
The correct technique is for the patient to breathe 100% oxygen via an anaesthetic circuit
and close-fitting mask for about 3 minutes of tidal volume breathing, or by three vital
capacity breaths has been demonstrated to be effective.
Dr.Nazzal Jabr
Anesthesia
Lec.3
Intravenous drugs: slow, smooth injection of an intravenous anaesthetic agent usually results
in loss of consciousness in less than 1 minute.
muscle relaxant : the induction agent may be followed by a muscle relaxant, particularly if
tracheal intubation is planned.
Intubation: the trachea is intubated with a cuffed tube following unconsciousness and muscle
relaxation. Uncuffed tubes are used in children to avoid local pressure on the tracheal wall
and to maximize the internal diameter of tube available.
Inhalational induction
It is often used as a means of inducing anaesthesia (particularly in a child) without having to site an
intravenous cannula first.
Indications:
1- Needle phobia or No venous access.
2- Inhalational induction (with intravenous access) is indicated for patients in whom airway
difficulties are expected. In these cases, the patient continues to breathe spontaneously
throughout and apnoea is avoided, since it may then be impossible to manually ventilate the
lungs with bag and mask.
3- Upper airway obstruction is an important indication for inhalation induction.
Maintenance of anaesthesia
It should provide:
1-
Maintenance of unconsciousness:
is usually achieved by anaesthetic drug delivery via
the inhalational or intravenous route, or both.
A- Inhalational route – this is the most widely used technique, using a volatile anaesthetic agent
with or without nitrous oxide.
B- Intravenous route – a popular alternative to inhalational anaesthesia is total intravenous
anaesthesia (TIVA).
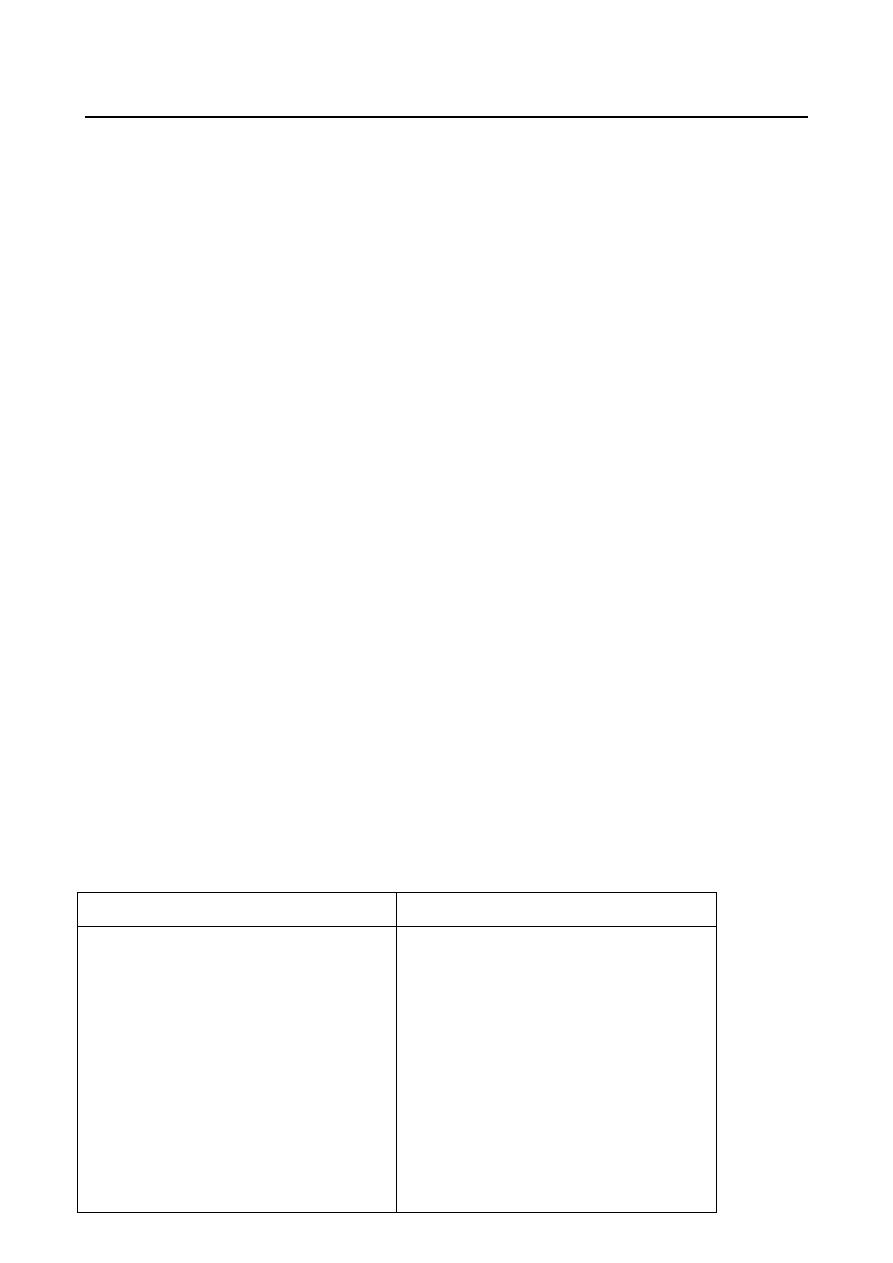
Inhalational
TIVA
Advantages
1- Cost-effective (when used with
low-flow circle systems)
2- Minimal metabolism of modern
agents
3- no accumulation
4- clearance independent of
patient hepatic and renal function
Advantages
1- No specialized equipment is
essential.
2- Rapid increase in anaesthetic
depth possible by administration
of intravenous bolus
3- Low incidence of postoperative
nausea and vomiting and
4- better quality of early recovery
(especially for propofol)
5- No contraindication in
malignant hyperpyrexia
Dr.Nazzal Jabr
Anesthesia
Lec.3
Disadvantage
1- Requires specialized equipment
(e.g. vaporizer)
2- Concern regarding tissue and
organ toxicity
3- All volatile anaesthetics are
known triggers for malignant
hyperpyrexia
4- Environmental pollution
Disadvantage
1- Requires patent and
dependable intravenous access.
2- Drug accumulation with
prolonged infusion
2-
Analgesia:
modern inhalational or intravenous anaesthetic drugs possess little analgesic
activity, with the exception of ketamine.
Analgesia has several effects.
1. It reduces the required of co-administered anaesthetic drugs. Analgesia is an important
component of the balanced anaesthetic technique.
2. It reduces the immediate autonomic activity in response to pain.
3. It reduces the neuroendocrine ‘stress response’ caused by surgery.
3-
Providing the best possible operating conditions
The surgeon hopes for two things from his patient during the operation: not to move, and
not to bleed. If the anaesthetist has succeeded in keeping the patient relaxed (using
appropriate muscle relaxant drugs) then the patient is unlikely to move.
The anesthetist can also help to minimize bleeding by:
Tourniquets
Positioning:
Hypotensive anaesthesia
Blood gases
Recovery from anaesthesia:
It is the process of retaining the patient to consciousness, orientation and resuming the
preoperative
vital state.
The recovery involve 5 points:
Emergence from General Anesthesia
Transport from the Operating Room
Arrival into recovery room
Management of postanesthetic problems
Discharge
postanesthetic problems include:
Airway Obstruction
Hypotension
Hypertension
Agitation & Delirium
Dr.Nazzal Jabr
Anesthesia
Lec.3
Shivering & Hypothermia
Nausea and Vomiting
Pain control
Discharge
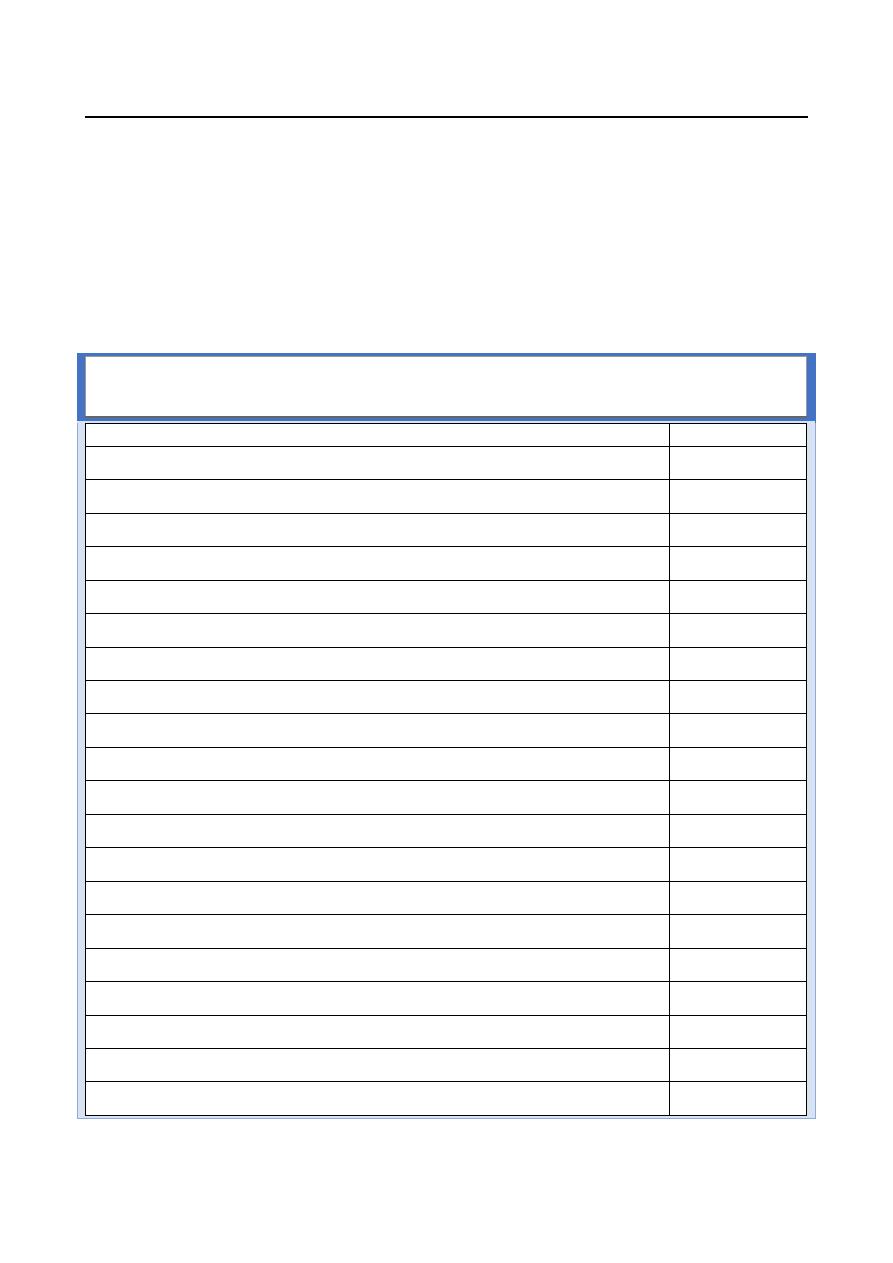
All patients must be evaluated by an anesthesiologist prior to discharge from the PACU unless strict
discharge criteria are adopted. Discharge criteria are based on Aldrete postanesthetic recovery
score. Ideally, the patient should be discharged when the total score is 10 but a minimum of 9 is
required.
Postanesthetic Aldrete Recovery Score.
Criteria
Point Value
Oxygenation
Sp
O
2
> 92% on room air
2
Sp
O
2
> 90% on oxygen
1
Sp
O
2
< 90% on oxygen
0
Respiration
Breathes deeply and coughs freely
2
Dyspneic, shallow or limited breathing
1
Apnea
0
Circulation
Blood pressure ± 20 mm Hg of normal
2
Blood pressure ± 20–50 mm Hg of normal
1
Blood pressure more than ± 50 mm Hg of normal
0
Consciousness
Fully awake
2
Arousable on calling
1
Not responsive
0
Activity
Moves all extremities
2
Moves two extremities
1
No movement
0
