Endodontic-Periodontic Lesions
Dr. Handren Hunar1
بريو نظري / خامس اسنان كركوك
د.هندرين22/4/2019
470
Endodontic-Periodontic Lesions
Periodontium and pulpal spaces represent the two primary sites of dental infection from oral bacteria.Persistent infection in the pulp tissue leads to secondary infection and breakdown of tissues in the periodontium. Conversely, severe periodontal disease may initiate or exacerbate inflammatory changes in the pulp tissue.
These two spaces are separated by hard shell of dentin, but they may communicate through various portals.
2
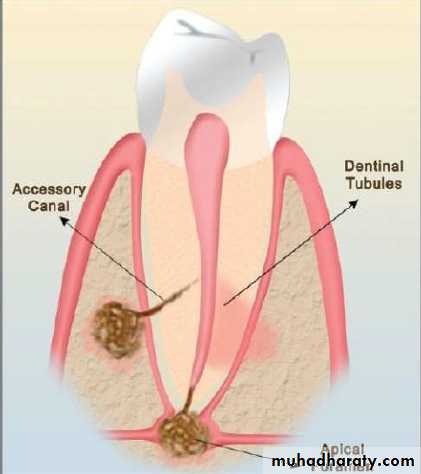
Pathways of communication
Anatomical pathwaysIatrogenic & Pathological pathways
3
Anatomical pathways
Apical foramen:
The apical foramen is the principal and most direct route of communication between the periodontium and the pulp.
accessory canals
multitude of branches connecting the main root canal system with the periodontal ligament.
The frequency of these canals on the root surface are as follows: apical third 17%, coronal third 1.6% and body of the root 8.8%.
Dentine tubules
maintain a tapered structure along the length from the pulpodentinal complex to the dentinoenamel junction with a diameter of 2.5 μm at the pulpodentinal complex and 0.9 μm at the dentinoenamel junction.
4
Iatrogenic & Pathological pathways
Idiopathic resorption- (internal and external).Exposure of dentinal tubules following root planing.
Accidental lateral perforation during endodontic procedure.
Root fractures caused by endodontic procedures
Agents, such as 30–35% hydrogen peroxide used in intracoronal bleaching can diffuse through dentine tubules.
5
WHAT IS ENDODONTIC LESION?
It is used to denote an inflammatory process in the perio dontal tissues resulting from noxious agents presents in the root canal system of the tooth, usually a root canal infection . Also called:Retrograde periodontitis
It represents periodontal tissue breakdown from an apical to a cervical direction.
6
WHAT IS PERIODONTAL LESION?
It is used to denote an inflammatory process in the periodontal tissue resulting from accumulation of dental plaque on the external tooth surface . Also called:
Orthograde periodontitis
Which results from a sulcular infection.
7
Retrograde
periodontitis8
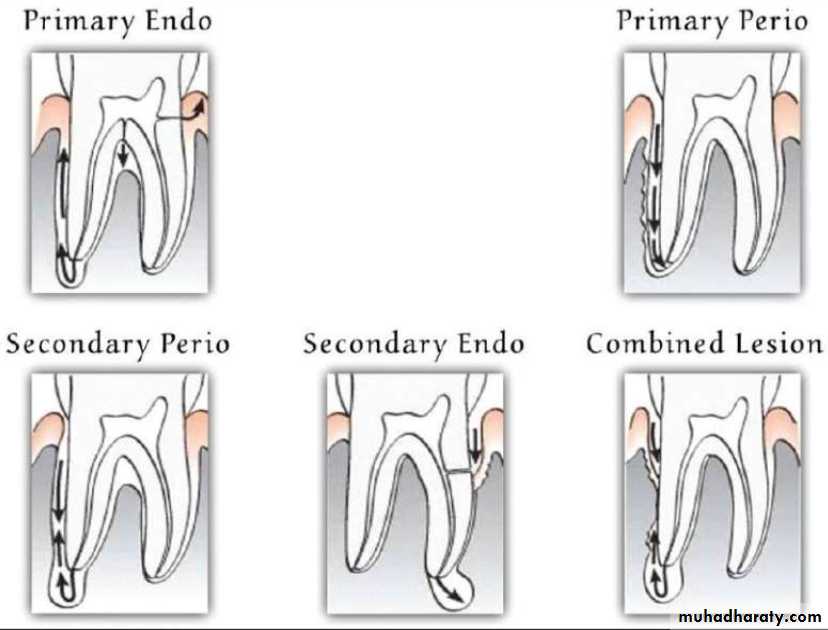
Classification of Pulpal and Apical Diseases
• Primary endodontic lesion• Primary periodontal lesion
• Primary endodontic lesion with secondary periodontal involvement
• Primary periodontal lesion with secondary endodontic involvement
• True combined lesion
9
10
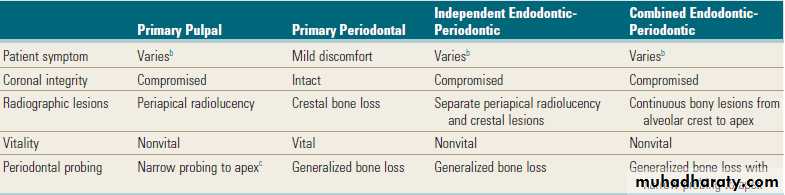
Classification of endodontic-periodontic lesions. (A) Primary pulpal infection can lead to chronic periradicular periodontitis by which a periapical radiolucency can develop and migrate cervically. Mandibular molars can also have accessory canals in lateral orientation or in the furcation area. These accessory canals can allow migration of the primary pulpal infection and cause secondary breakdown of the periodontium at their respective loci. (B) Primary periodontal infection can lead to extensive breakdown of alveolar crest bone that migrates from the cervical area to the apex. In these lesions, one would find generalized bone loss around a single tooth or that often could involve multiple adjacent teeth. Because of the pulpal-periodontal continuum through main root canal foramina or through accessory canals, extensive periodontal infection can cause irritation in the pulp tissues. (C) Both primary pulpal infection and primary periodontal infection can occur simultaneously in an “independent” endo-perio lesion, exhibiting the characteristics of both. (D) Primary pulpal and primary periodontal infections can occur extensively in this “combined” endo-perio lesion.
11
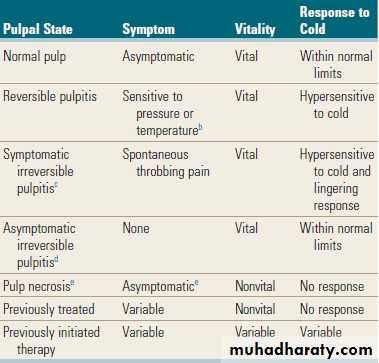
Classification of Pulpal Diseases
12
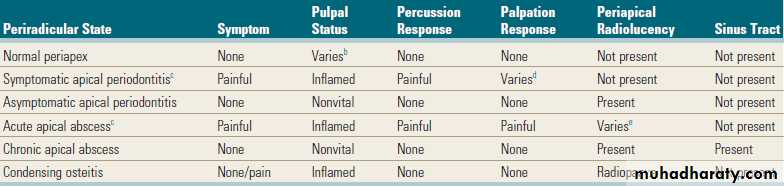
Classification of Periradicular Diseases
13
Different Characteristics of Pulpal and Periodontal Lesions
14
Factors Initiating Pulpal and Apical Diseases
BacterialThermomechnical.
Investigators noted that even a small increase in pulpal temperature (5° to 6° C) is capable of inducing necrotic changes in the pulp.
chemical irritants impose measurable changes in the pulp status ( acid etch, bonding & composit).
Root canal overfills with gutta-percha and sealers invariably cause severe inflammatory reactions in the apical tissues, even though patients may be completely asymptomatic
15
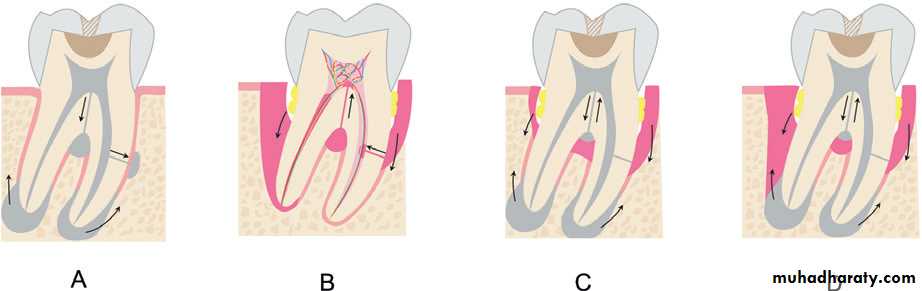
Factors Initiating Pulpal and Apical Diseases
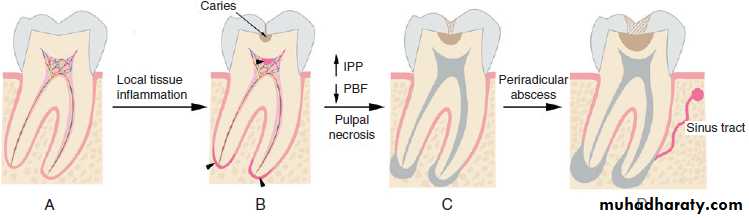
Progression of the pulpal and periradicular pathosis. (A) Normal tooth without any pulpal pathosis is richly vascularized and innervated. (B) With microbial challenges such as caries, local tissue inflammation can occur in the pulp adjacent to the site of carious lesions, as well as in the apical regions (arrowheads). (C) Pulpal inflammation can lead to reduction in pulpal blood flow (PBF) caused by an increase in intrapulpal pressure (IPP), causing pulpal necrosis (shown in gray). (D) Pulpal necrosis, if left untreated, can cause chronic inflammation of periradicular tissues and abscess formation, leading to a draining sinus tract.
16
EFFECTS OF PULPAL DISEASE ON PERIODONTIUM
Bone resorptionRadiolucency at the apex of the root
Highly vascularized granulation tissue infiltrate to varrying degrees by inflammatory cells
Nutrophils are present near the apical foramen
Plasma cells , macrophages, lymphocytes in fibroblast are increased in the periphery of the lesion
17
VARIOUS DIAGNOSTIC PROCEDURES THAT CAN BE USED TO IDENTIFY PERIO ENDO LESIONS
• Visual examination• Palpation
• Percussion
• Mobility
• Radiographs
• Pulp vitality testing
• Pocket probing
• Fistula tracking
• Cracked tooth testing
18
Visual examination
Soft tissues:
• Inflmmation
• Ulcerations
• Sinus tracts
Teeth:
• Caries
• Deffective restorations
• Abrasions
• Crack
• Fractures
• Discolorations
19
Palpation
Periradicular abnormalitiesCannot differentiate between endodontic and periodontic lesion
Compare with control teeth
Percussion
Compare with control teeth
Periraducular inflammation
20
Mobility
Loss of periodontal supportFractured roots
Recent traumas
Periradicular abscess
Radiographs
Periradicular resorption of endodontic origin- not effective
Bone loss due to periodontal disease- effective
21
Pulp vitality testing
Abnormal response- degenerative changesNo response- pulp necrosis
Modern transient response- normal vital pulp
Quick painful response- reversible pulpitis
Lingering painful response- irreversible pulpitis
22
Pocket probing
Probing depthClinical attachment level
Sinus tracking
Fistula tracking
Semi-rigid radiopaque material (gutta percha) then take X Ray.
23
Cracked tooth testing
Transillumination
Wedging
staining
24
Treatement
Primary endodontic lesionconventional endodontic therapy
Primary endodontic lesion with secondory periodontal involvement
endo-perio therapy
Primary periodontal lesion
Periodontal therapy
Guided tissue regeneration
Root amputation and hemisection
Pulp space therapy
25
Treatement
Primary periodontal lesion with secondary endo lesionSpace therapy
Periodontal therapy
Root amputation
GTR
True combined lesion
Endo therapy
Perio therapy
hemisection
bicuspidization
Root amputation
26
Conclusion
Periodontitis Associated with Endodontic Disease may be difficult to diagnose, but an understanding of the lesions help in diagnosis, proper treatment and better prognosis.
27