1
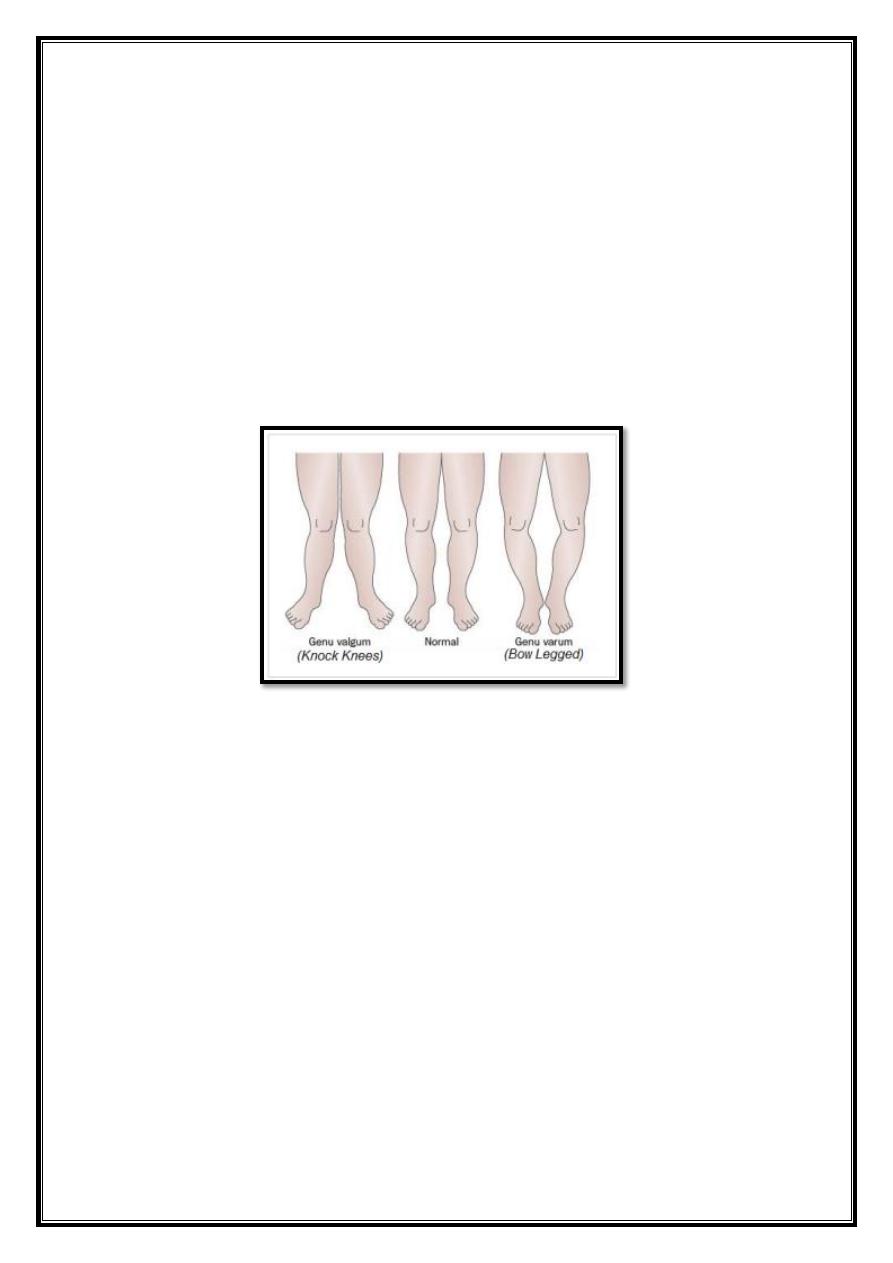
Deformities of the knee
In normal adult the knees are in 5 ̊ – 7
̊ valgus, any deviation from this
may be regarded as deformity.
Types
1. Genu – Varum (Bowleg)
2. Genu – Valgum (knock knee)
3. Hyperextention (genu – recurvatum)
Developmental Bowleg & knock knee
Bilateral bowleg can be recorded by measuring the distance
between the knees with leg held in full extension & heels touching.
It should be less than 6cm.
Knocked knee can be estimated measuring the distance between
the medial malleolus when the knee is held touching with patella
facing forward. It is usually less than 8cm.
Bow leg in babies and knocked knee in 4 years old are so common
that they are considered be normal stages of development.
Other postural abnormalities such any pigeon toes and flat feet
may coexist but these children are normal in all other respect.
The deformity almost in variably correct spontaneously by the age
of 10-12.
Treatment is unnecessary but parents should be reassured and child
should be seen at intervals of 6 months to record progress.
2
In occasional case where by the age 10 years the deformity is still
marked (i.e. the intercondylar distance is more than 10 an operative
R, should be advised.
Types of operative treatment:
1. Stapling of medial or lateral side of knee physis to produce
asymmetrical growth. The staples are removed once the knee has
over corrected slightly.
2. Osteotomy after growth is completed
a. Supra condyler osteostomy for G. valgum.
b. High tibial osteotomy for a varus.
Secondary bow leg & knock knee in children
1. Disorder that distort physical growth
e.g. dysplasia, Ricket, unilateral injuries of growth plate.
Treatment in severe cases operative correction.
2. Apparent bow leg:
e.g. Excessive Anteversion of femoral neck, with patella facing
forward the varus deformity disappear.
Treatment if needed a derotation osteotomy of the femur.
3. Complex deformities:
e.g. varus femur + valgus tibia as in Ricket, polyosteotic lesion such
multiple exostosis.
Treatment corrective osteotomings
Genu Varum & Valgum in adults
1. Sequally to childhood deformity.
If the deformity associated with lig. instability this can lead to O.A.
of medial compartment in varus & lateral compartment in valgus.
It may predispose to patellar dislocation & O.A in valgus knee.
Treatment osteotomy.
Above knee in valgus.
Below knee → in varus.
3
7
2.
Deformities secondary to arthritis
e.g. varus in O.A.
Valgus in Rh. Arthritis.
In these joint is often unstable and corrective osteotomy less
predictable in its effect.
Stress x-ray are essential in the assessment of these cases.
3. Ligamentous injuries, Malunited fracture, pagets disease.
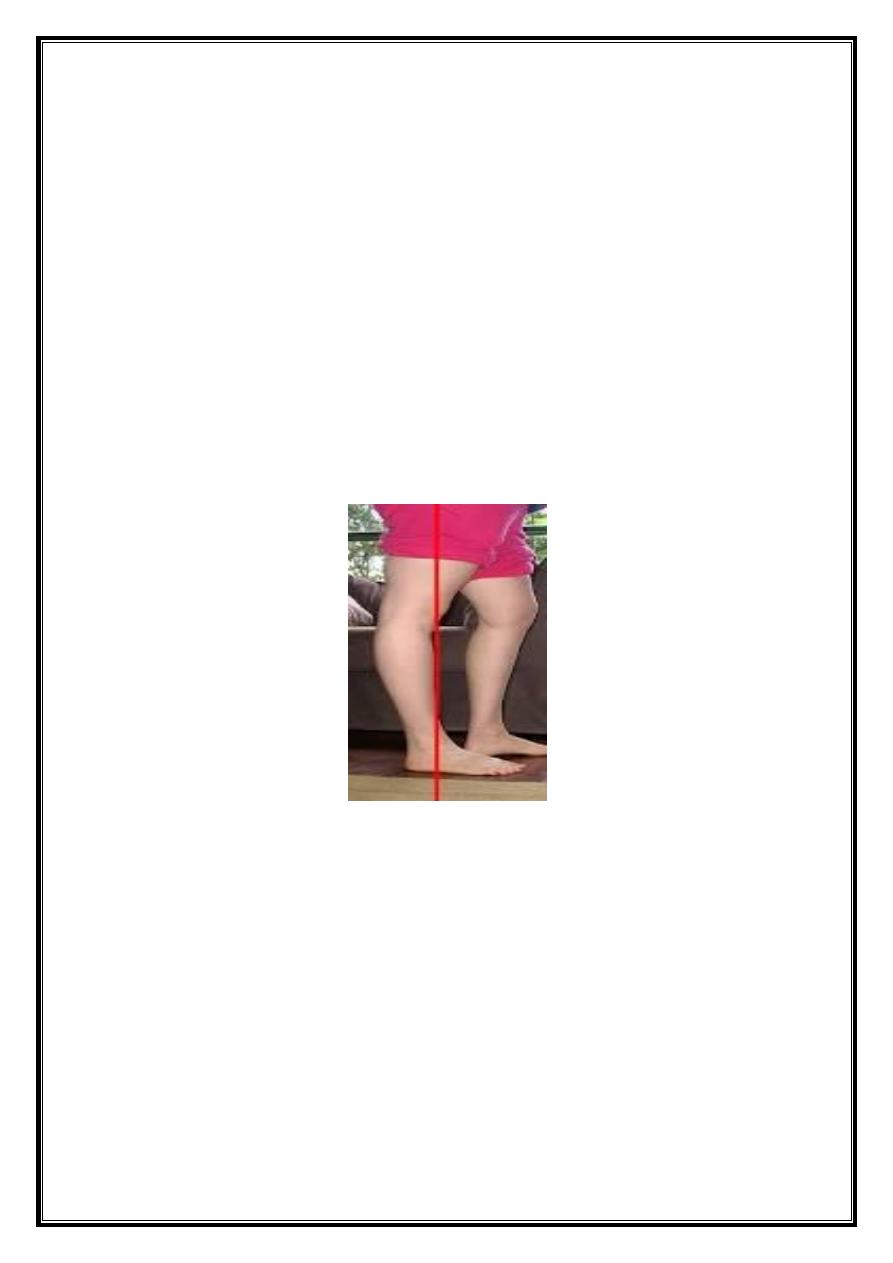
Hyperextension of knee (Genu recurvatum)
1. Congenital recurvatum: may be due to
a. Intarutaine postion (spontaneous) recovery.
b. True congenital dislocation of knee → rare.
2. Lax ligament:
e.g.
Prolonged tration on frame.
Holding knee hyperextended in plaster.
Lig. overstretching following chronic or reccurent synovitis as in
Rh.Arthirtis.
Hypotonia of rickets, poliomyelites, charcot diseas.
4
3. Recurvatum may be secondary to fixed equinus of the Ankle.
In severe paralytic hyperextension treatment is by fixing patella into tibial
plateau where it acts as a bone block.
4. Other causes:
Growth plate injuries
Malunited #s.
Treatment osteotomy.
6
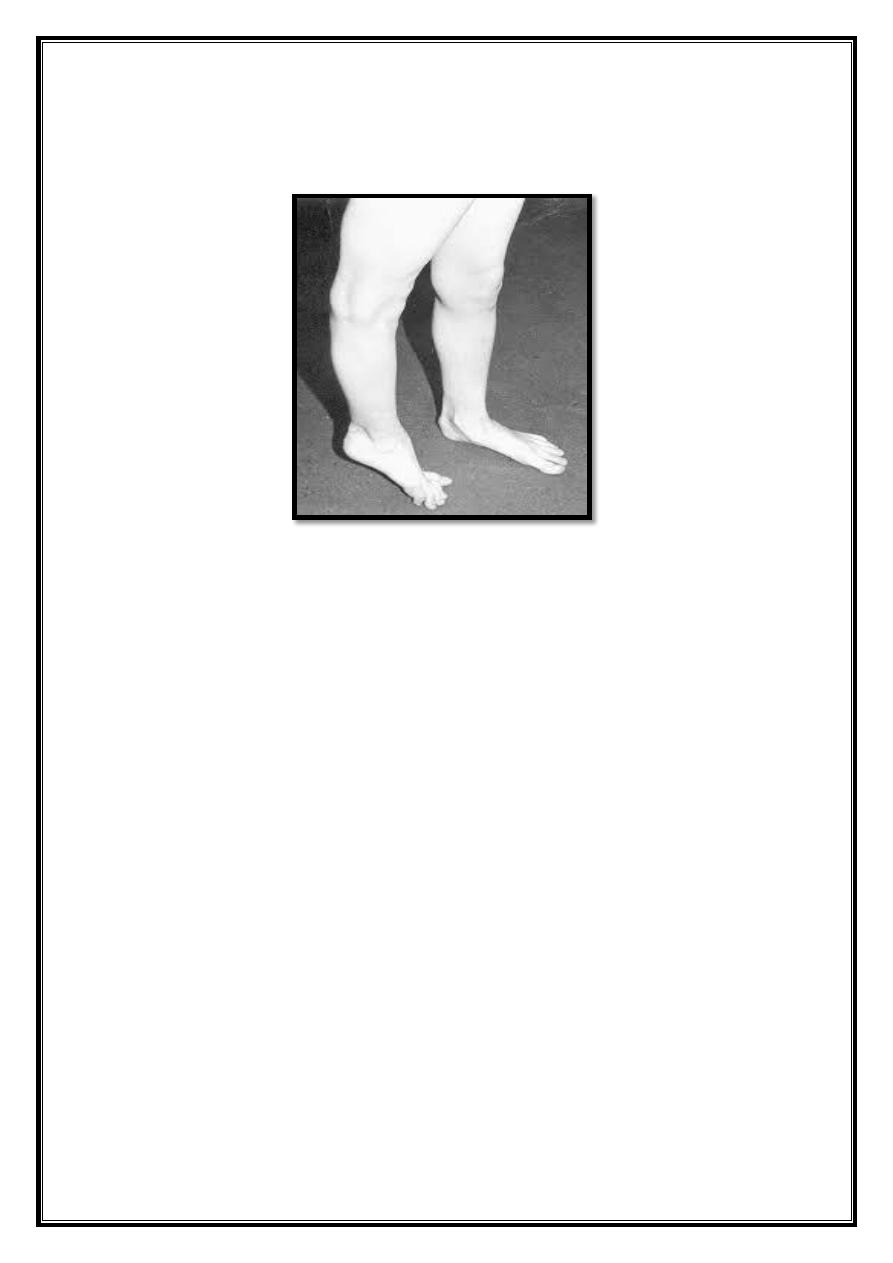
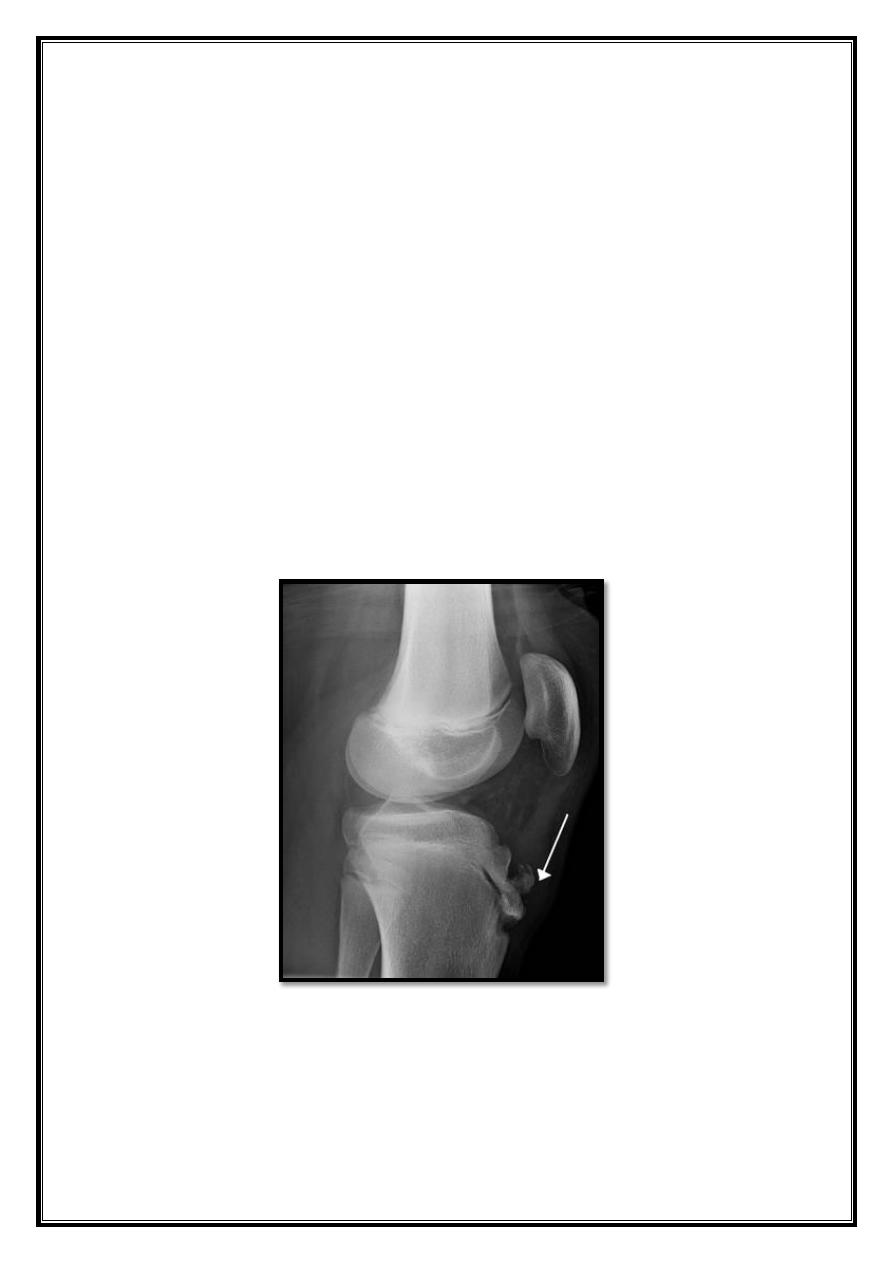
Blount disease
This is a progressive bow leg deformity associated with abnormal
growth of posteromedial part of proximal tibial epiphysis.
Common in the west Indies & parts of Africa.
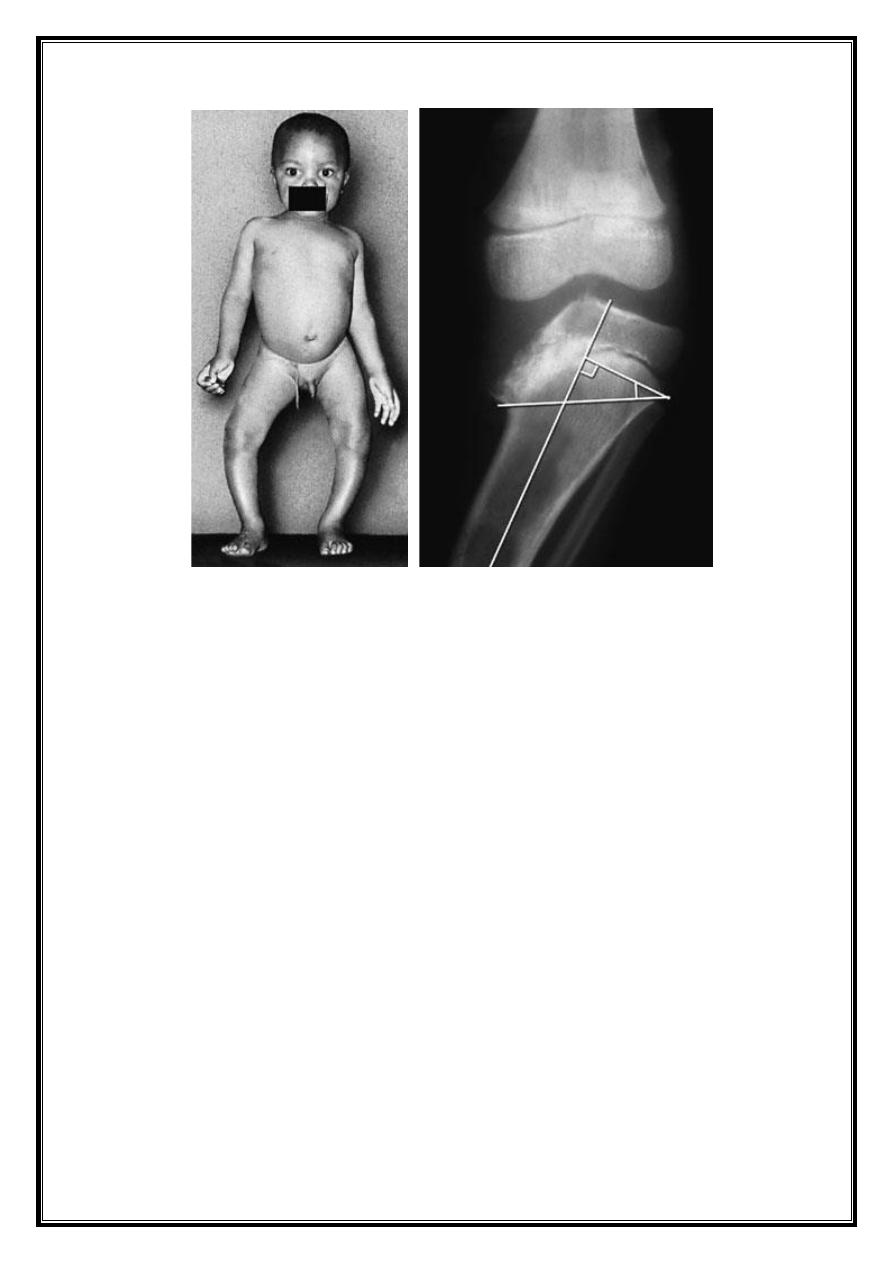
5
On x-ray tibial epiphysis is flat end medially & adjacent
metaphysic is somewhat beak shaped. In the worst cases the
epiphysis looks fragmented. Occasionally the femoral epiphysis
also is affected.
The children are usually over weight and start walking early.
The resulting deformity is nearly always bilateral (80%) and is
usually associated with internal rotation of the tibia.
Spontaneous resolution is rare & once it is clear that the deformity
is progressive treatment by corrective osteotomy aiming at 6 ̊ – 10 ̊
valgus. Both tibia and fibula need to be osteotsomized. This
procedure should accompanied by fasciotomy to reduce the risk of
post operative compartment syndrome.
6
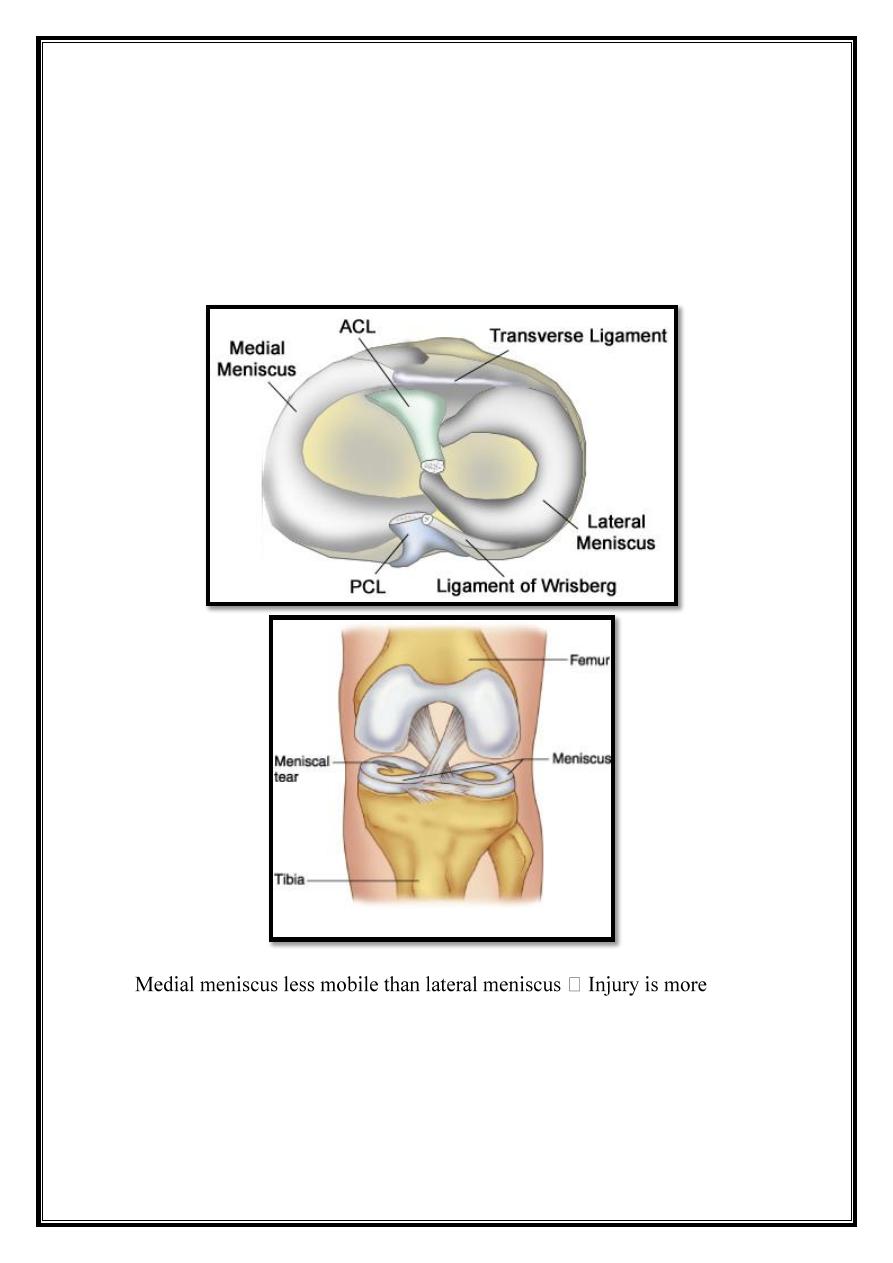
Meniscal Injuries
Meniscal function
1. Stability.
2. Control gliding movement.
3. Distributing load.
common
Anatomy
Circumferential fiber
Few radial fiber
Therefore probability to tear along its length than across its width.
7
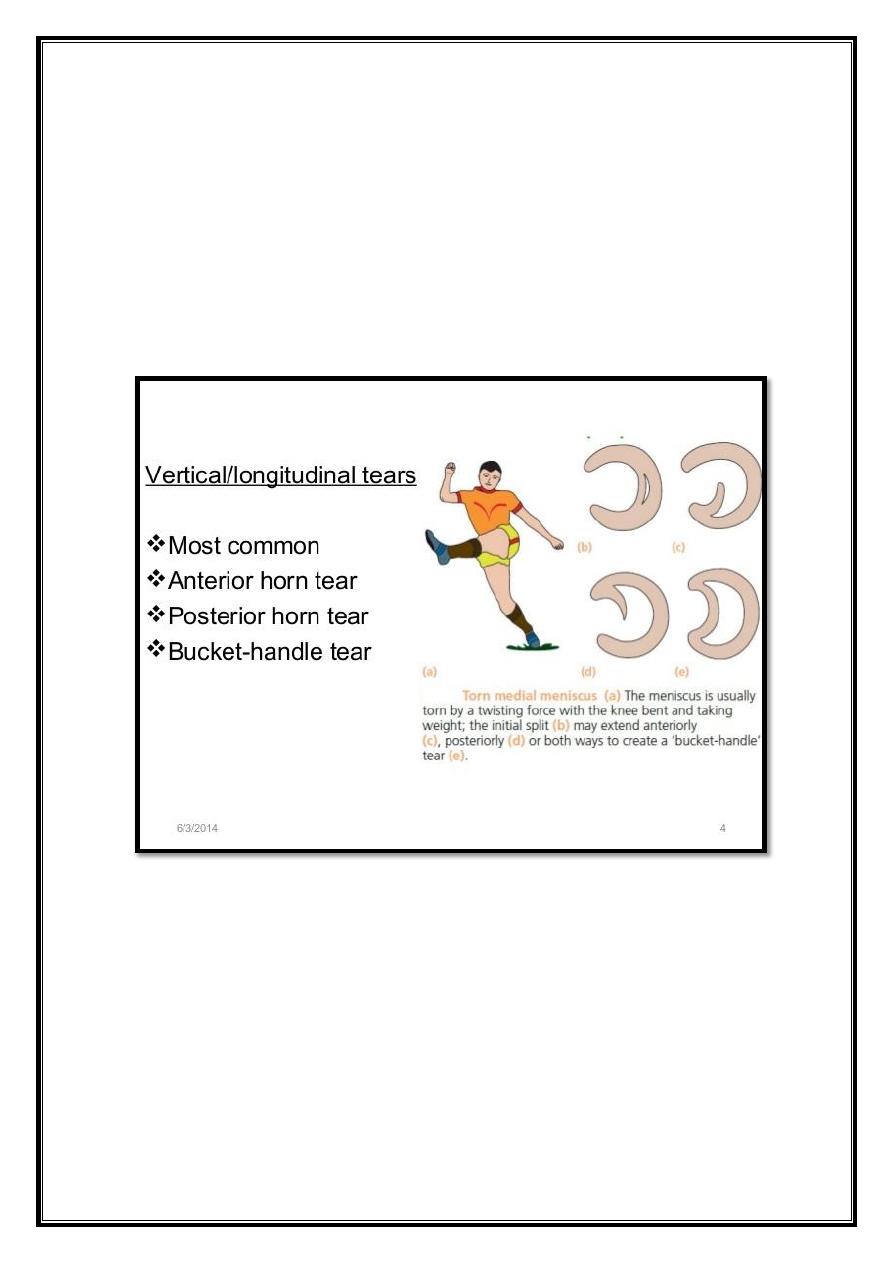
Meniscal tear
Mechanism
Knee flexed
Twisting
Wt bearing
Common
Foot baller
Middle life (fibrosis and restricted mobility need little force).
8
Pathology
Medial > lateral
Both menisci may be torn in sever ligmentous injuries.
75% tear is vertical in length of meniscus i.e. bucket handle.
Flab tear (ant. Or post.)
Horizontal: usually deg.
Repeated trauma
Some associated with meniscal cyst.
Most menisci is avascular and spontaneous repair doesn’t occur
unless the tear is outer third.
Loose tag act as mechanical irritant to synoviam to secrete synovial
fluid (i.e. effusion) and some cases secondary O.A.
Clinical feature
Patient is young having H/O twisting.
Pain → usually on medial side often server so further activity is
avoided.
Occasionally knee is locked in partial flexion.
Swelling appear some hours later or perhaps the following days.
With rest symptoms subside to recover periodically after trivial
twist or strain.
Sometimes giving way followed by pain and swelling.
In patient over 40 yrs: initial injury is unremarkable and main
complaint is giving way or locking.
Examination
Knee joint may slightly flexed.
Effusion
Q.M. wasting in long standing case.
Tenderness at joint line. In vast majority on medial side.
Flexion is usually full but extension is limited.
Between attack of pain and effusion there disconcerting paucity of
sign.
Mc marry & apley’s griding tests may be positive.
9
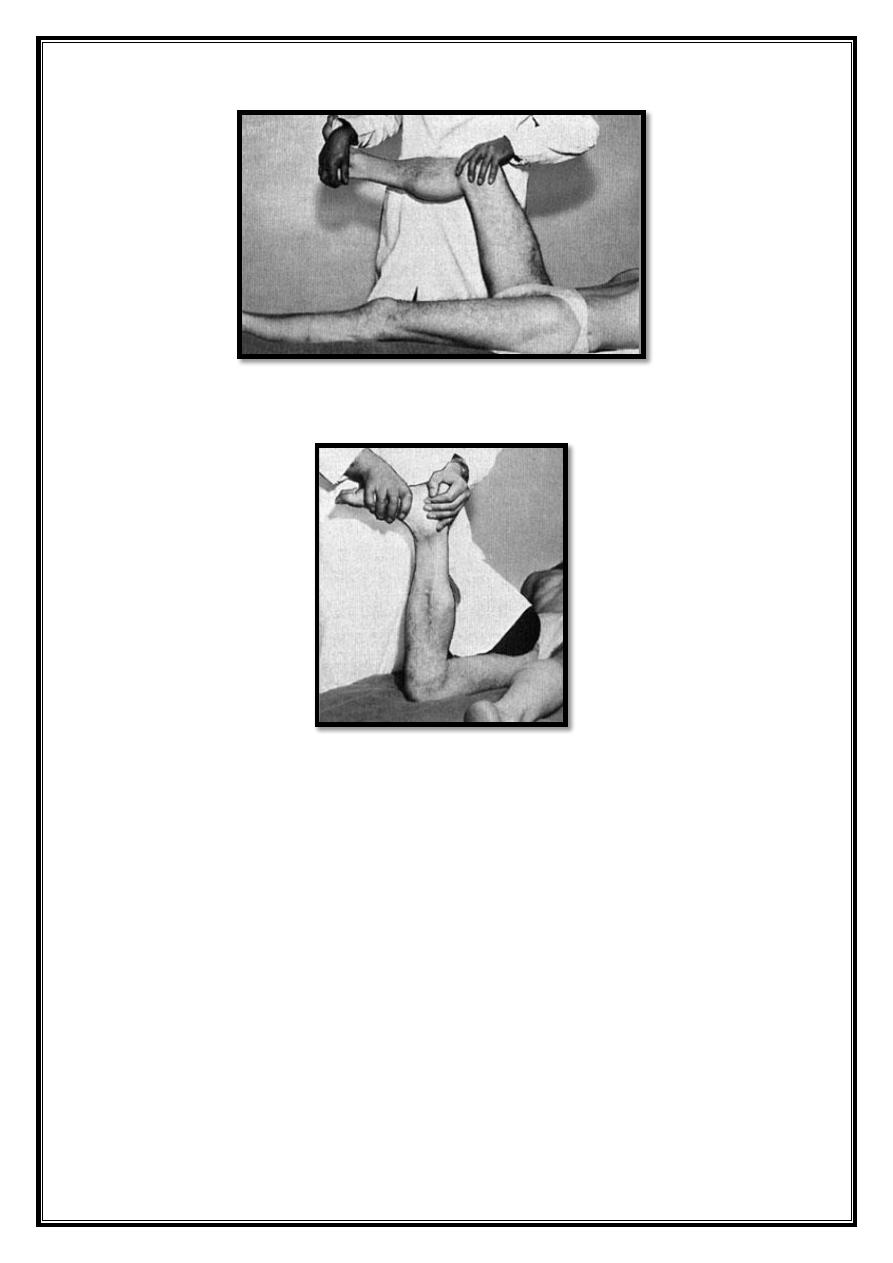
McMurray’s test
The grinding test
10
Investigation
Plain x-ray → may be normal.
MRI → reliable method.
Arthroscopy.
DDX
.
1. Loose body.
2. Recurrent dislocation patella. (i.e. Apprehension test)
3. Fracture tibial spine.
4. Partial tear of MCL.
5. Torn ACL.
Treatment
Locked knee
1.
Unlock spontaneously .
2. Gentle passive flexion and rotation(no forceful manipulation).
3. Arthroscopy.
Conservative treatment
1. If the joint is not locked.
2. If the symptoms that are not disabling.
Watson Jones bandage.
Crutches
Q.M. exercise.
Operative treatment :
A. Surgery: indication:
1. Joint can’t be unlocked.
2. Recurrent mechanical symptom(locking or catching).
3. Failure of conservative treatment.
B.
Arthroscopy :
Repair or partial menisecatomy
11
Meniscal degeneration
Patient > 45 yrs.
Symptoms → same
Arthroscopy: horizontal tear with associated O.A. or chondro
malacia.
Treatment
Repair
Minor menisectomy
Discoid meniscus
The meniscus is disc like shape instead of semilunar shape.
Symptoms :
1. The knee gives way and thuds loudy.
2. Characteristic click may be felt at 110 ̊ as the knee is bent and at 10 ̊ as it
is being straightened .
Diagnosis:
by MRI.
Treatment :
is not essentially unless the pain is intrusive , treatment by
menisecoplasty
Meniscal cyst
Traumatic in origin.
Arising from small horizontal tear.
Synovial cell infiltrate into the vascular area between menisous and
capsule and then multiply.
It contains gelatinous fluid.
Clinical feature
Swelling at the joint line.
Lateral side > medial side.
Patient complain of aches worse.
After activity.
On examination
Lump between joint line.
Usually anterior to collateral lig.
Seen easily with knee flexed.
In some position may disappear altogether.
Lateral cyst solid swelling
Medial cyst soft and large.
12
DDX.
Ganglion
Calcific deposite in collateral lig.
Prolapsed torn meniscus.
Various tumors (lipoma, fibroma)
Treatment
Arthroscopy
Remove torn or damaged meniscus.
Decompress cyst from the joint
Patella femoral over load syndrome
Synonym:
(
chondromalacia patellae), (Patellar pain syndrome)
Def:
syndrome of anterior knee pain & Patello. Femoral. tenderness.
Pathology:
Mechanical overload of P.F. joint.
Rarely single inj., most common repetitive over load due to either:
1. Malcongruence P.F. surfaces.
2. Malalignment of extensor mechanism.
a. Tilt.
b. Subluxation.
Changes
P.F articular cartilage softening and fibrillation.
Subchondral bone vascular congestion (intra osseous hypertension)
→ resultant anterior knee pain.
A.C. fibrillation.
1. Usually occur on medial articular facet.
2. Rarely on lateral facet (ficat hypertension zone syndrome).
CL/F
1. Patient teenage girls or young adult athletic.
2. Pain over front of the knee or underneath knee cup.
Symp.
Occasionally H/O recurrent subluxation.
Symptoms are aggravated by activity or climbing stairs, when
standing up after prolonged sitting.
The knee may give way.
13
There may be swelling.
Sometime knee catch (Not true locking).
Often both knees affected.
Sign
First knee looks normal.
Careful examination reveals malalignment or tilting of the
patellae.
Quadriceps m. wasting.
Fluid in the knee.
Tender under the edge of patella.
Crepitus on moving the knee.
Pressing the patellae against femoral condyles creating pain.
Apprehension test is positive (suggests previous subluxation
or dislocation).
Patellar tracking can be observed while patient sitting on the
edge of couch flexing & extending the knee.
Q angle in supine position. (normally: 0-7).
Lastly examine the structure around the knee for other sources
of pain.
Examine the hip to exclude referred pain.
Image:
X-ray:
- Skyline view → patellar tilt.
- Lateral view → high or small patellae.
CT & MRI
- Most accurate way for measuring patella- Femoral malposition in
full extension & varying degree of flexion.
Arthroscopy
- A.C softening (in asymptomatic knee).
- It can serve to gauge patellofemoral congruence, alignment, and
tracking.
- It excludes other causes of ant. Knee pain.
DDX.:
1. Referred from hip
2. Patellofemoral disorders:
-
Patellar instability
-
Osteochondral injury
-
Patello-femoral osteoarthritis.
14
3. Knee joint disorders
-
Osteochondritis dissecans.
-
Loose body in the joint.
-
Synovial chondromatosis.
4. Peri-articular disorders.
-
Patellar tendinitis.
-
Patellar ligament strain.
-
Bursitis.
-
Osgood–Schlatter disease
Treatment:
Conservation treatment:
1. Adjustment of stressful activities.
2. Physiotherapy.
3. Reassurance that most patient recovered. Exercise the medial
quadriceps so as to counter balance the tendency to tilt or
subluxation of the patella.
4. NSAIDs.
5. Avoid. corticosteroidal injection.
Operative treatment:
Indications
1. There is demonstrable abnormality that is correctable by
operation.
2. Conservative treatment has been tried for at least 6 months.
3. Patient genuinely incapacitated.
Principle of operation:
1. Improve patellar alignment & patellafemoral congruence.
2. Reduce patellofemoral pressure.
3. Lateral release of the capsule (tilt) + medial reefing.
4. If there is instability (maquet patellar lig. elevation procedure.
5. Chondroplasty (open, arthroscopy) .
6. Last resort patellectomy (in
severe discomfort).
15
Osgood–Schlatter disease(apophysitis of the tibial tubercle)
Common disorder of adolescent in which the tibial tubercle become
painful and swelling.
Pathology:
Traction injury of apophysis in which part of the patellar tendon is
inserted.
Symptoms:
1. No history of injury.
2. Sometime bilateral.
3. Young adolescent complain of pain after activity.
4. The lump is tender and its situation over the tibial tuberosity is
diagnostic.
5. Active extension of the knee against resistance is painful.
X-ray:
reveal fragmentation of the apophysis
MRI:
confirm the diagnosis and exclude other causes of the pain.
Treatment:
1. Spontaneous recovery is usual but take time.
2. Restricted activity such as cycling jumping, and soccer.
3. If symptoms persist and separated ossicle in the tendon can be
identified surgical removal can be considered.
16
Swelling of the knee
It is either soft tissue or bone swelling
I.
Entire knee joint swelling:
a. Acute swelling of the joint:
1. Posttraumatic heamarthrosis.
2. Bleeding disorder.
3. Acute septic arthritis.
4. Traumatic synovitis.
5. Aseptic nontraumatic synovitis(gout, pseudogout,
inflammatory monopathy).
b. Chronic swelling of the joint:
1. Arthritis( OA, inflammatory arthritis).
2. Synovial disorder (synovial chondromatosis, pigmented
villonodular synovitis).
II.
Swelling in front of the joint:
1. Prepatellar bursitis (HOUSE MAIDE 'S KNEE).
2. Infrapatellar bursitis ( CLERGYMN 'S KNEE).
3. Other bursae (Bursae deep to patellar tendon may become
inflamed and painful).
III.
Swelling at the back of the knee joint:
1. Semimembranosus bursae.
2. Popleteal cyst.
3. Popleteal aneurysm.
Bone swelling around the knee joint:
1.
Benign bone swelling ( osteochondromata , Osgood–Schlatter
disease
).
2. Malignant bone swelling.
17
Ankle & Foot diseases
Congenital Clubfoot
Talipes Equino Varus
.
The term talipes is derived from talus (latin=ankle) and pes
(latin=foot).
May be bilateral in one-third of cases.
More common in males thanfemales(Twice)
Occurs in about 1-2 out of 1000 birth.
Clubfoot is the most common congenital
disorder of the legs.
It can range from mild and flexible to severe and rigid.
Causes
The exact cause is unknown, possible mechanisms:
1. Germ defect or arrested development.
2. There is in utero malalignment of the talocalcaneal, talonavicular
and
calcaneocuboid joint.
3. Neurological disorder and neural tube defect ( myelomeningocele,
spinal dysraphism).
4. Severe clubfoot deformity are seen in association with :
a. Arthrogryposis.
b. Dysraphic dysplasia.
c. Amniotic constriction ring.
d.
Poliomyelitis .
e.
Cerebral palsy.
f. Peroneal type of progressive muscle atrophy
.
18
Pathological anatomy:
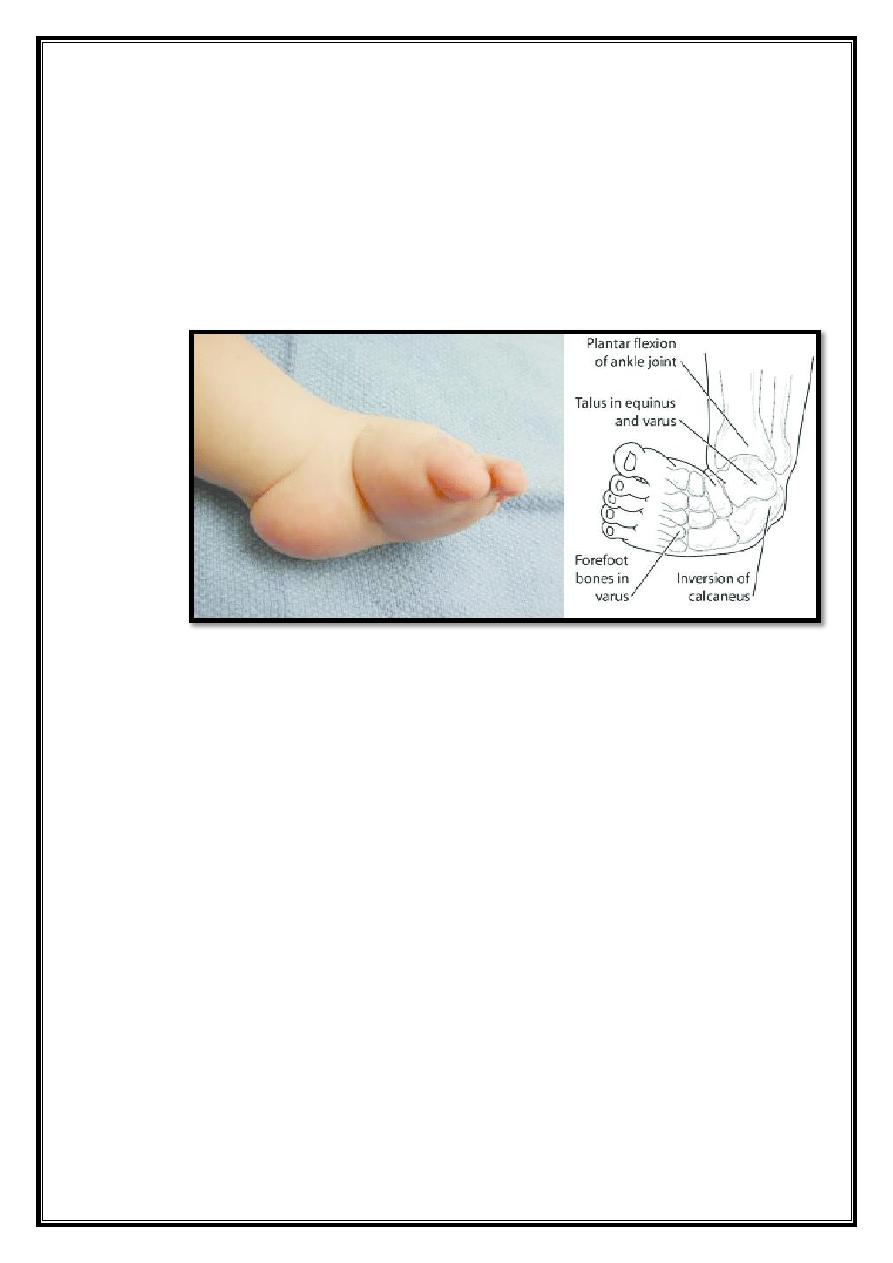
1. The ankle is in equinus. The heel is inverted, the forefoot is
adducted and supinated.
2. Sometimes the foot also has a high medial arch(cavus), deep
creases appear posteriorly and medially.
Clinical Anatomy
affected limb:
may be shortened.
calf muscle is atrophic.
and foot is short. compared to opposite side.
medial rotation of tibia
.
N.B : Always examine the hips for D.D.H. and the back for spina
bifida.
19
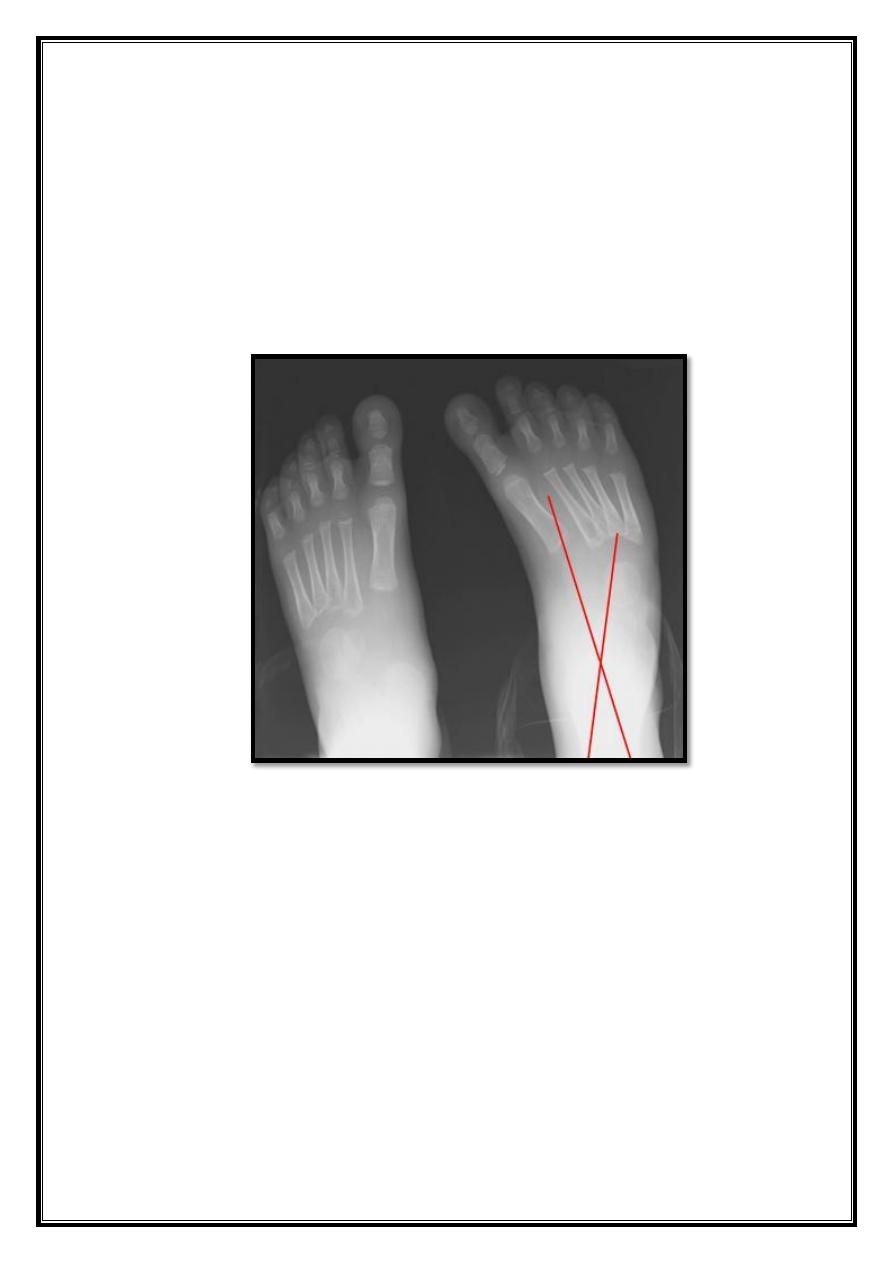
X- ray:
To assess progress after treatment
AP of Foot:
Taken in 30 deg plantar flexion, with the x-ray tube directed 30 deg
from the perpendicular:
Lines are drawn longitudinally thru the talus parallel to its medial
border and thru the calcaneus parallel to its lateral border.
On ap view, talocalcaneal angle should be between 25- 40 deg;
In club foot the two lines may be almost parallel.
20
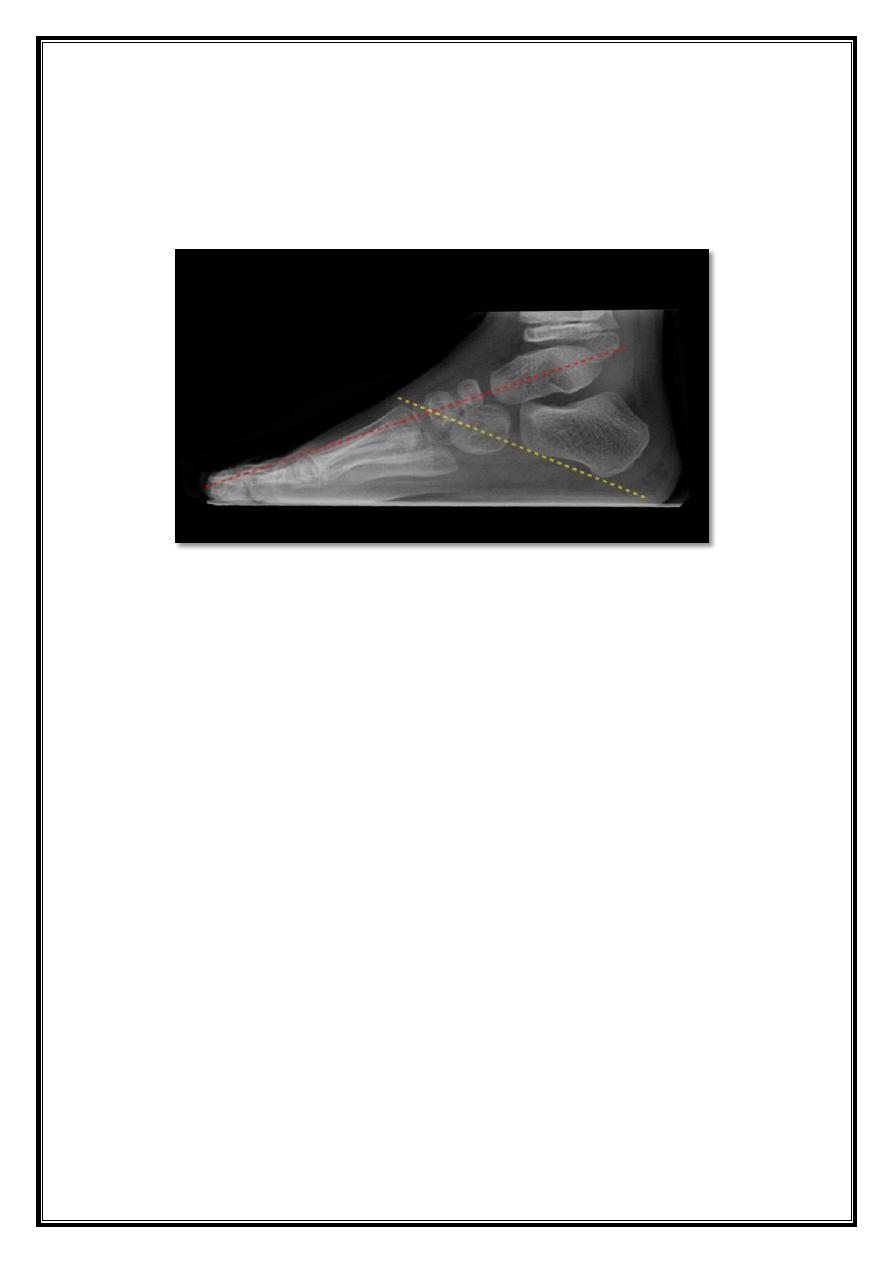
Forced dorsiflexion lateral view:
Lines are drawn longitudinally thru the central axis of talus and parallel
to the lower border of the body of the calcaneus this angle should be
between 35 - 40 deg.
Treatment
Aim:
To correct the deformity
.
Full correction
.
Maintain correction until foot stop growth
Two types of club foot are recognized:
a. Easy cases: responds to splintage.
b. Resistant cases: no response to splintage
21
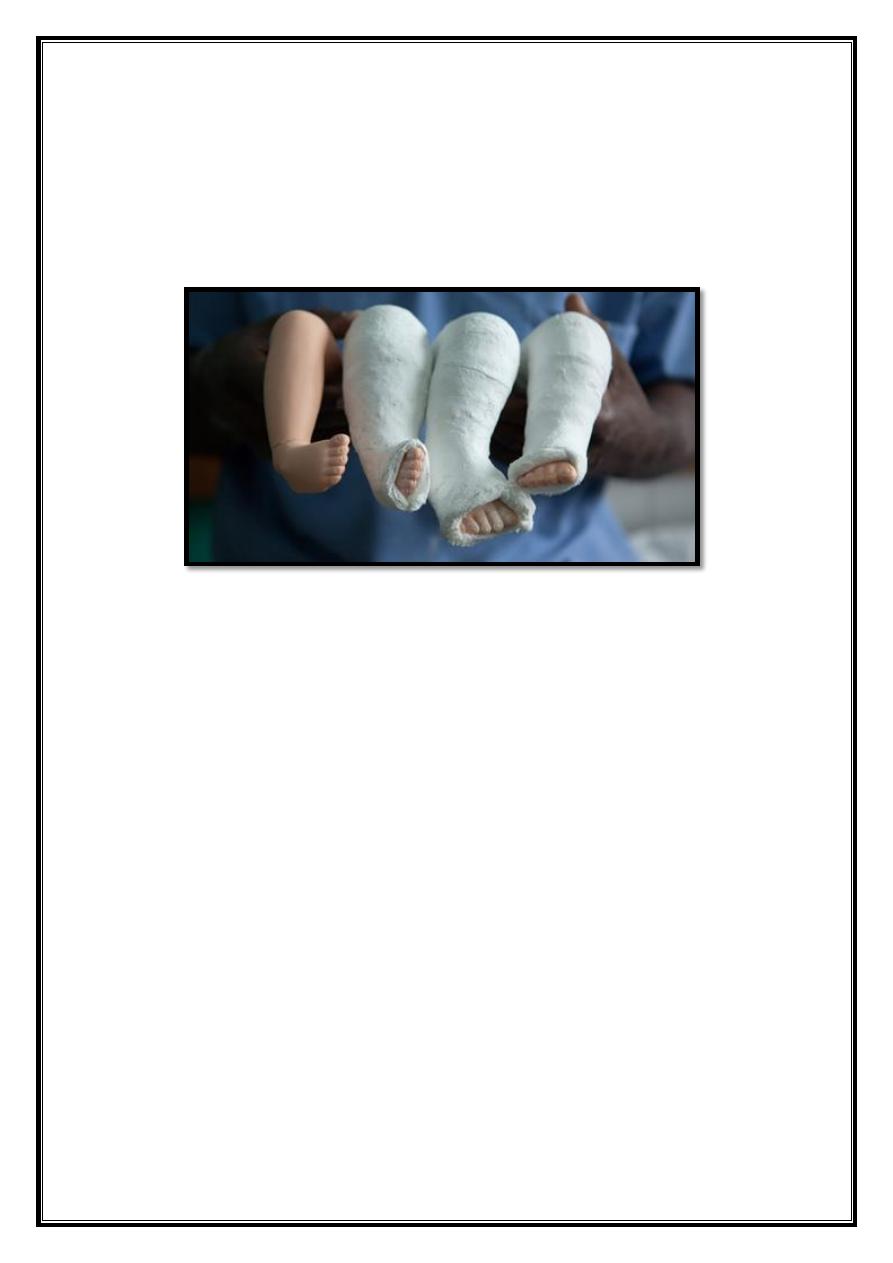
Splintage: (Ponsetti)
Gentle stretching and recasting occurs every week to improve the
position
of the foot.
Generally, five to 10 casts are needed.
The final cast remains in place for 3 weeks.
Operation
Circumferential release: "cincinati incision"
Approach:
Medial release
.
Posterior release
.
posteromedial release.
1. Complete release of joint tethers (capsular ligamentous
contractures and fibrotic bands) .
2. Lengthening of tendons so that the foot can be positioned normally
without tension.
Salvage procedures:
Combined soft-tissue and bone procedures.
Arthrodesis / osteotomy: (triple arthrodesis).
22
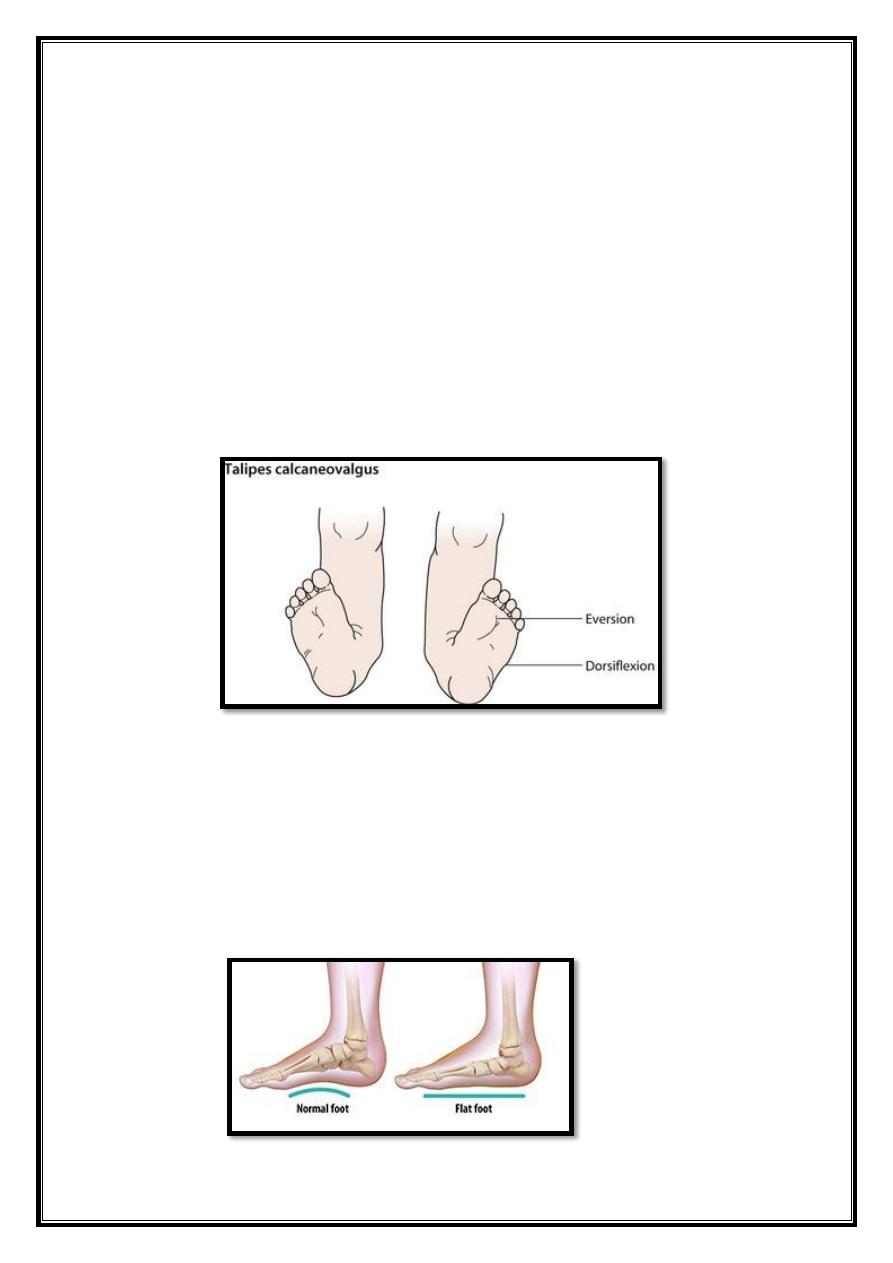
Talipes calcaneovalgus
It is a common deformity that presents in newborn as an
acutely dorsiflexed
foot.
This is postural deformity probably due to abnormal
intrauterine position and it is usually bilateral.
There is deep crease on the front of the ankle.
Unlike congenital vertical talus (which also presented as
acutely dorsiflexed foot), talipes calcaneovalgus is flexible, the
creases in congenital vertical talus located over the midfoot.
It is often corrected spontaneously in the neonatal period. In
resistant cases may require serial cast for correction.
Flat foot (pes planus)
The apex of the medial arch is collapsed.
Medial border of the foot is in contact with the ground.
Heel is in valgus.
Foot pronates at subtalar, midtarsal joints
.
23
Aetiology
1. Developemental disorder.
2. Ligamentous laxity.
3. Muscle weakness e.g. paralytic disorder.
4. Abnormal load distribution e.g. knock knees
.
A.
Flat foot in children & adolescents
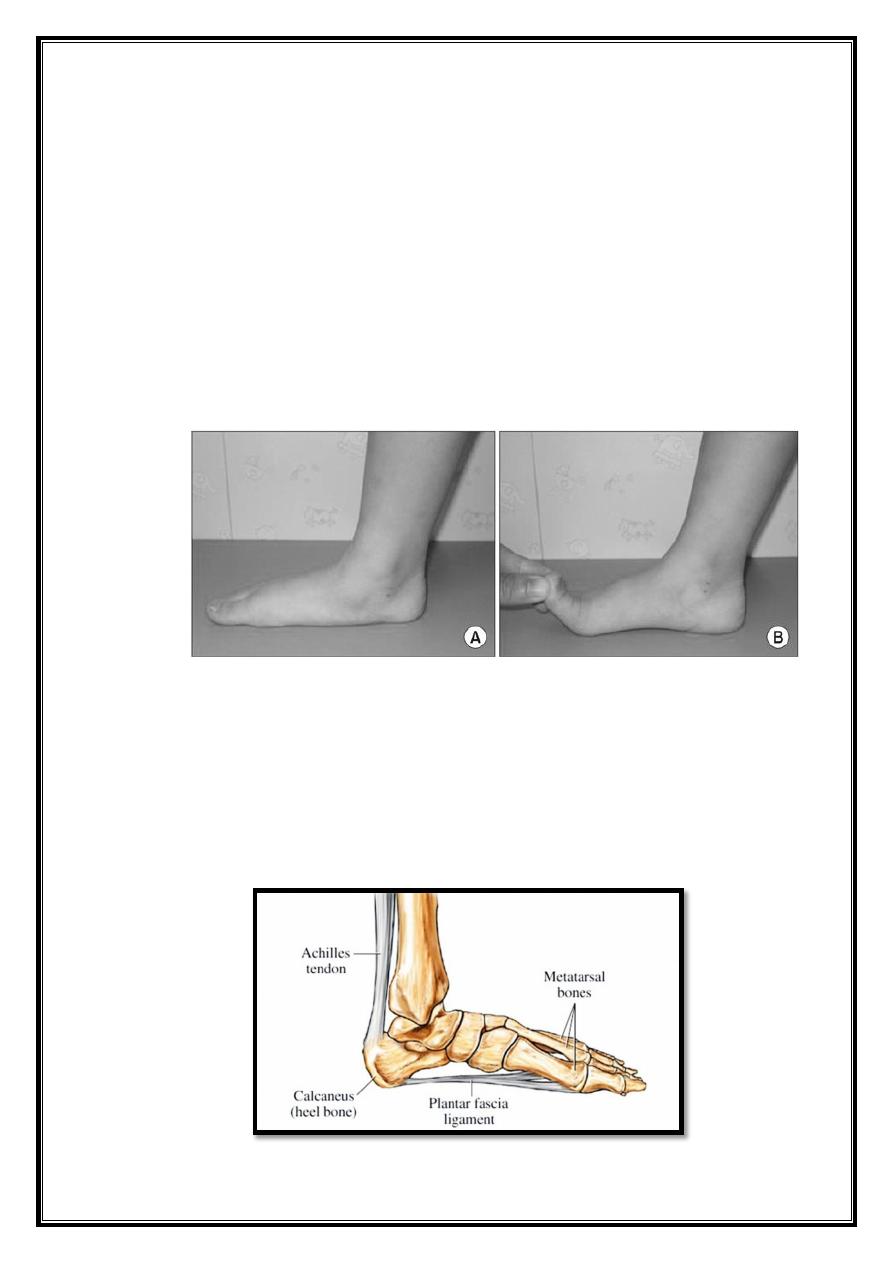
1. Flexible flat-foot. Appears in toddlers as a normal stage in
development and it usually disappear between 4- 10 years of age,
the arch can often be restored by simply dorsi flexing the great toe
(Jack`s test).
2. Stiff flat-foot .
-
Congenital vertical talus.
-
Tarsal coalition.
-
Inflammatory joint disorder
.
-
Neurological disorder
.
3. Compensatory flat-foot, Tight tendo Achillis.
24
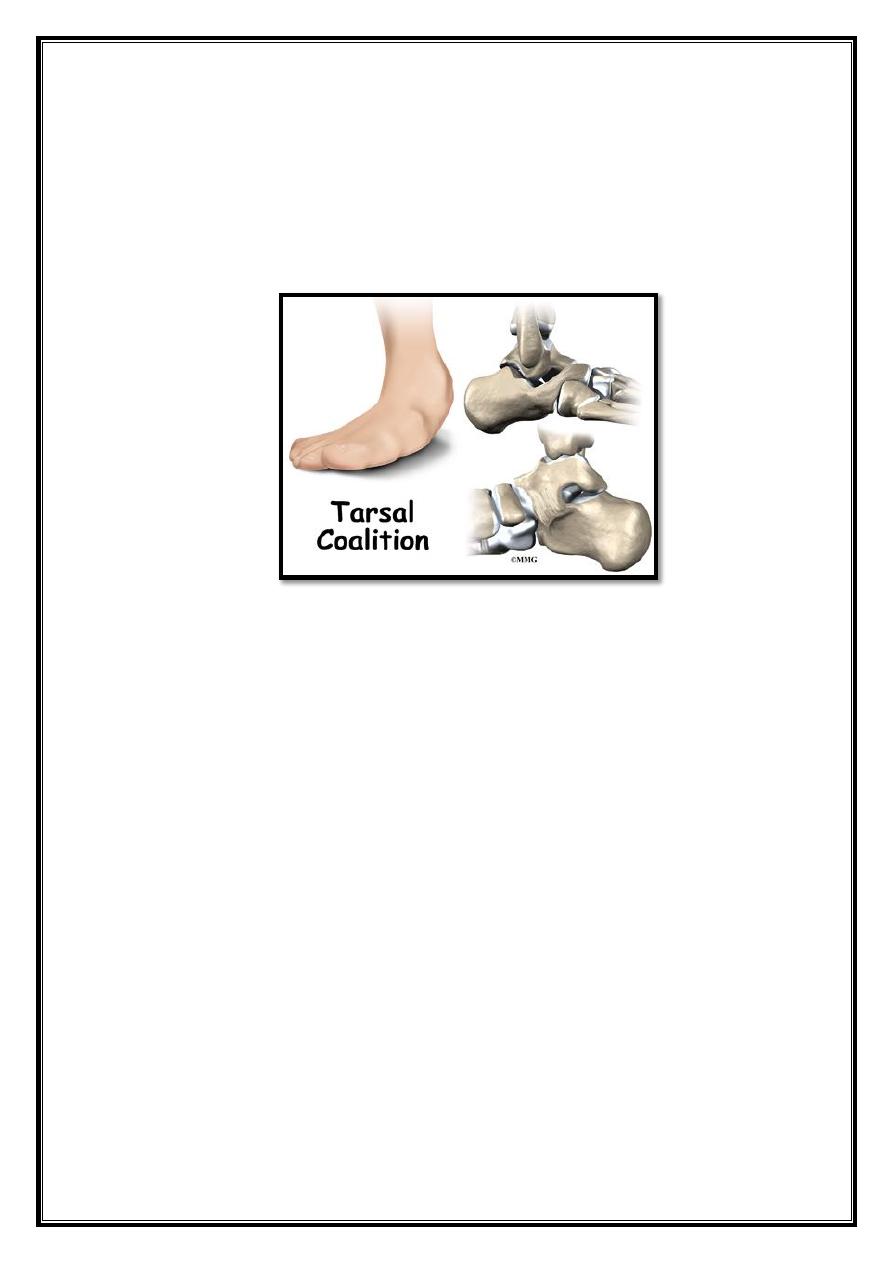
4. Peroneal spastic flat-foot (Tarsal coalition) Autosomal dominant
condition, is present at birth but it becomes symptomatic only
when the abnormal fibrous syndesmosis matures into a stiffer,
cartilaginous syndesmosis that later ossifies to become a rigid bar.
Talocalcaneal, calcaneonavicular and talonavicular.
B.
("Adul t acquired flatfoot")
Flat feet can also develop as an adult ("adult acquired flatfoot") due
to
injury, illness, unusual or prolonged stress to the foot, faulty
biomechanics, or as part of the normal aging process.
This is most common in woman over 40 years of age. Known risk
factors include obesity, hypertension and diabetes.
Flat feet can also occur in pregnant women as a result of temporary
changes, due to increased elastin (elasticity) during pregnancy.
Disorders of tibialis posterior tendon
.
Treatment
In children & adolescents
Flexible: no need for special treatment.
Tight tendo Achillis: tendon-stretching exercises.
Accessory navicular: the accessory bone can be shelled out from
within the tibialis posterior tendon.
Tarsal coalition: resection of the bar and the gap filled with fat or a
piece of muscle. or triple arthrodesis.
Relative rest
.
25
Support with a temporary insole
.
Elasticated foot/ankle support
.
NSAIDs.
Functional foot orthotics(FFOs)
.
Surgery:
surgical decompression
.
Tenosynovestomy
.
reconstruction of tibialis posterior tendon+calcaneal osteotomy
or triple
arthrodesis.
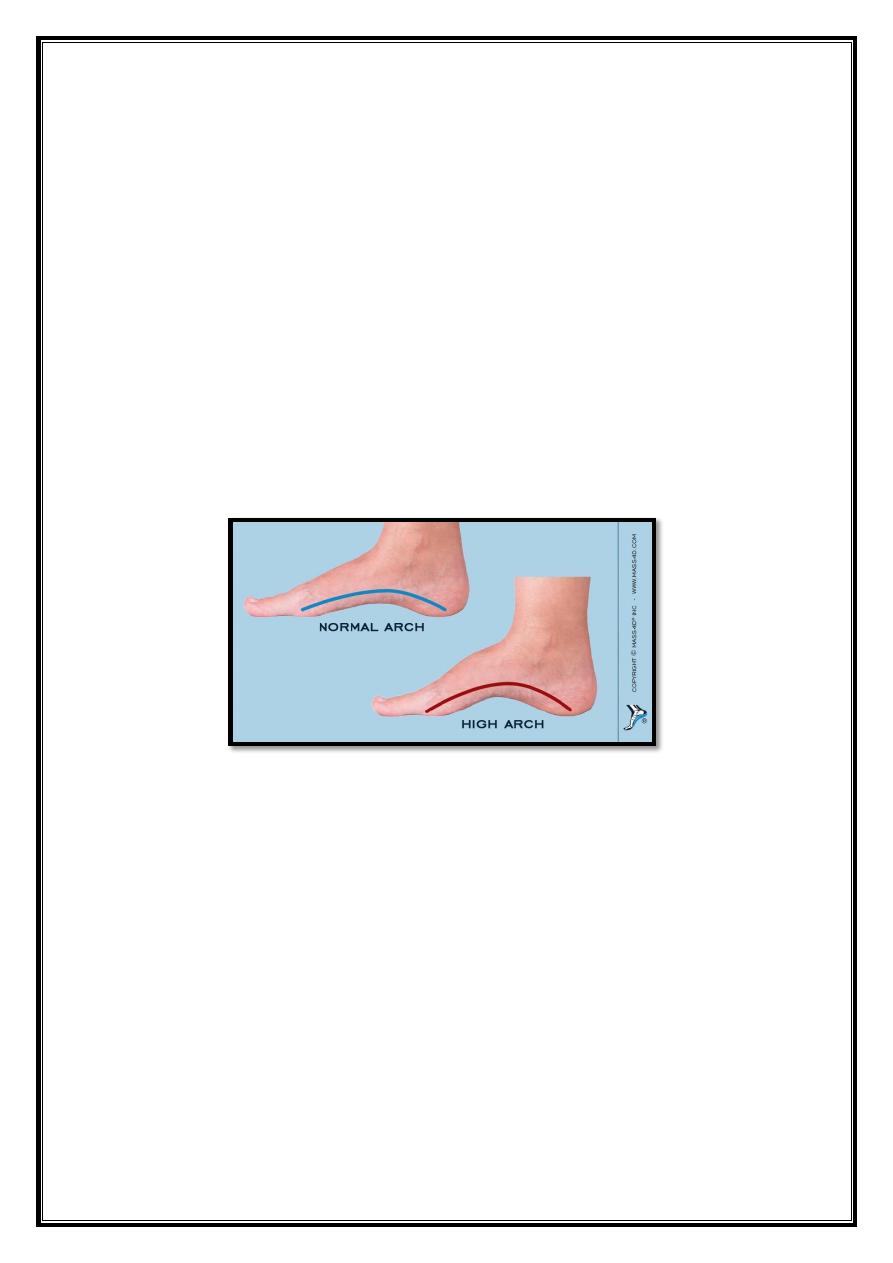
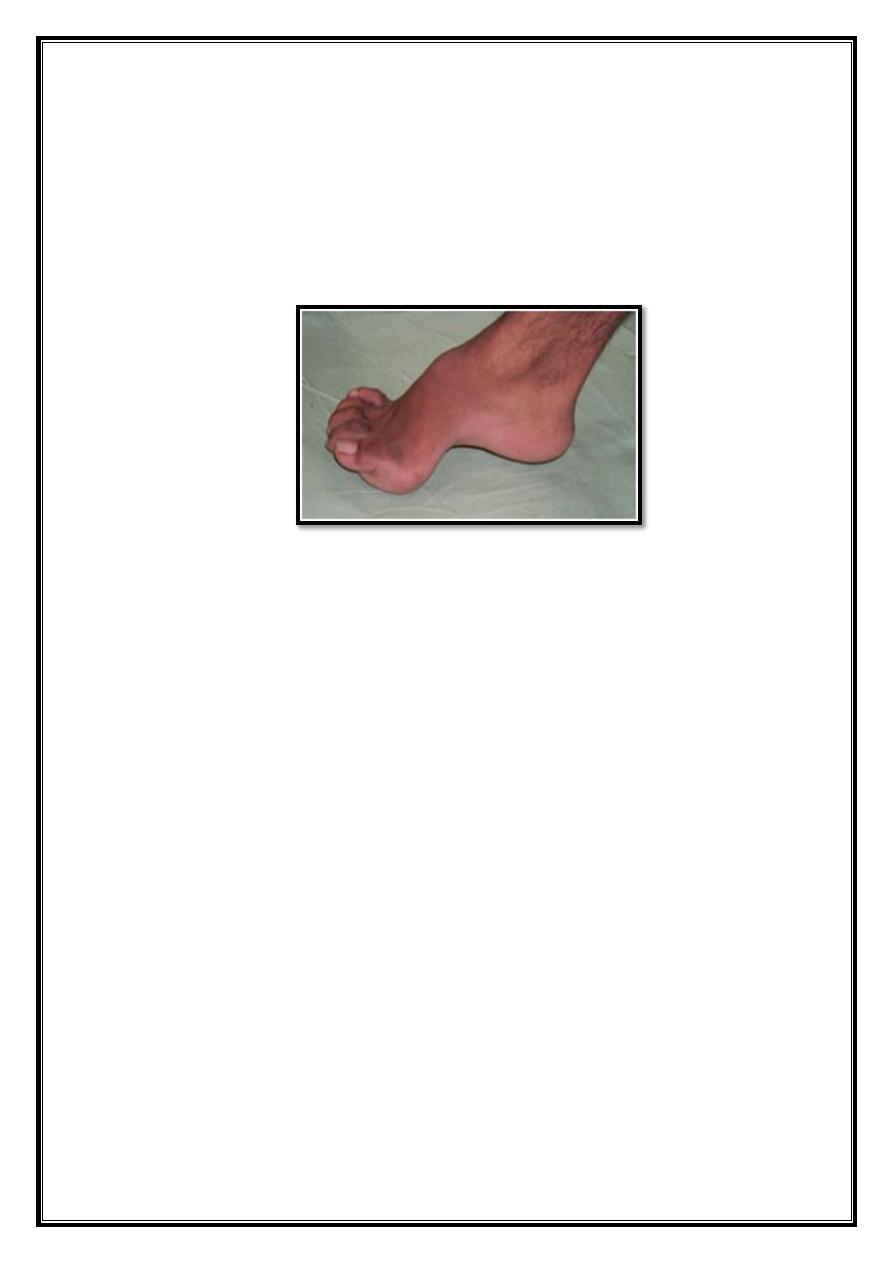
Pes cavus
The medial arch is higher than normal &often there is also clawing of the
toes.
Aetiology
Weakness or paralysis of intrinsicmuscles of the foot e.g. peroneal
atrophy.
Myelomeningocele.
Poliomyelitis.
Cerebralpalsy.
26
Pathology
Arch of the mid foot is accentuated
.
Metatarsal heads: forced into the sole
.
Toes: clawed
.
Heel: inverted.
soft tissue at the sole are tight
.
Treatment
Arch support, use of especially custom- made shoes
Operation: if conservative treatment fails
1. soft tissue release (steindler) .
2. Bony surgery (wedge tarsectomy)
.
27
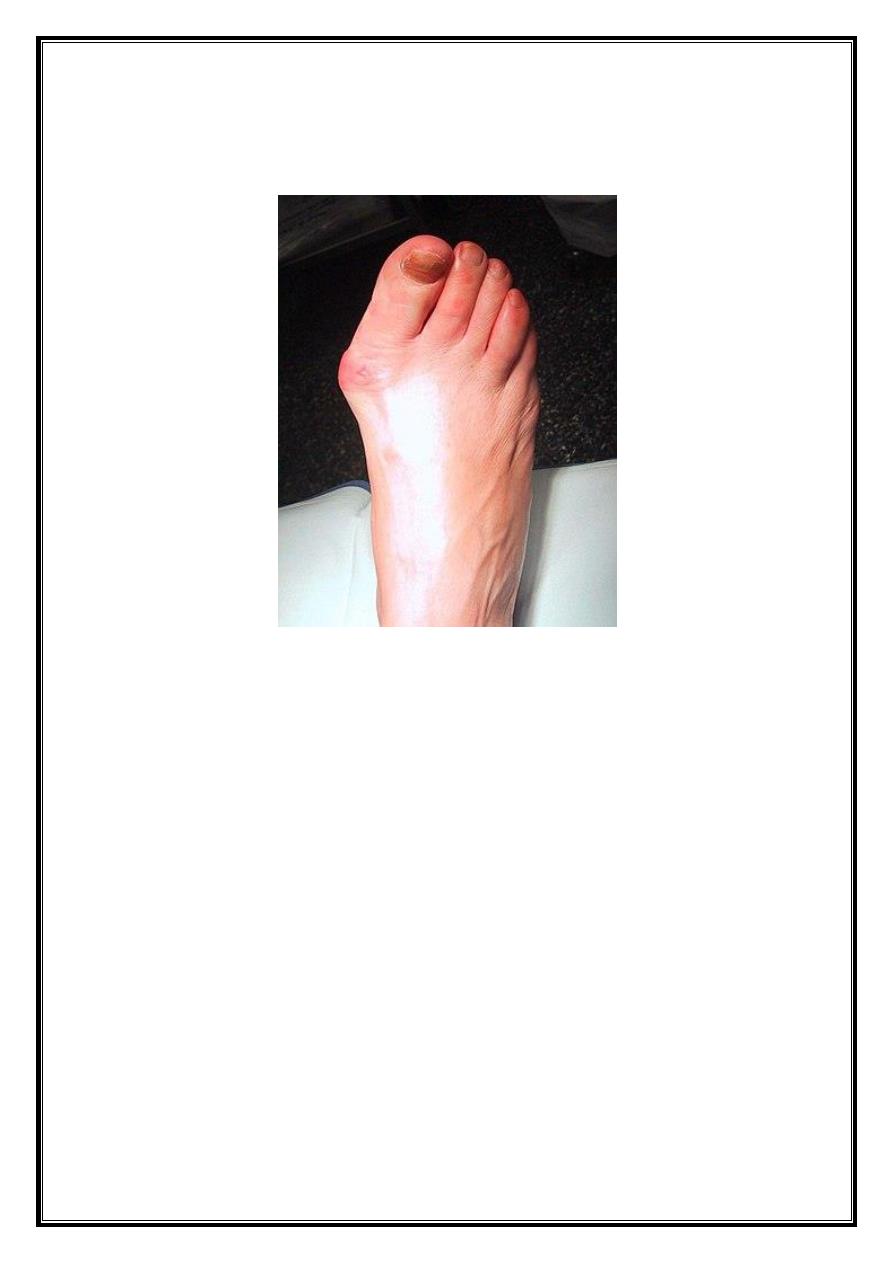
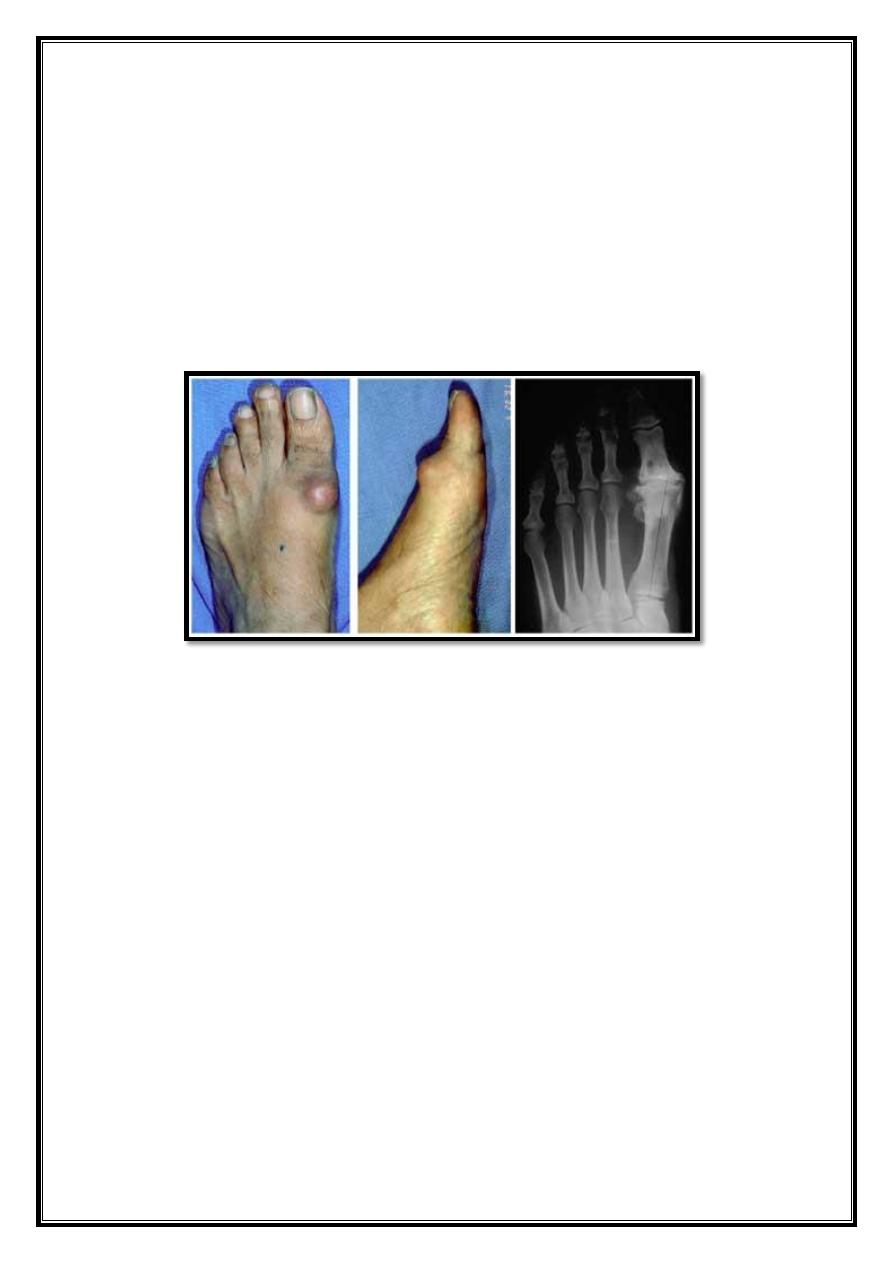
Hallux valgus
Excessive lateral deviation of the big toe away from the midline.
Aetiology
Hereditary factors (positive family history).
Metatarsal primus varus. (congenital or may result from loss of
muscle tone in forefoot in elderly).
Use of shoes, high heels.
R. arthritis.
Clinical Features
Women more men
.
Pain over bunion (prominence of 1st metatarsal head is due to
subluxation of MTP joint, increasing shoe pressure on medial side
leads overlying bursa &thickened soft tissue).
Worries about cosmoses
.
difficulty fitting shoes.
Circulation
.
Sensation
.
28
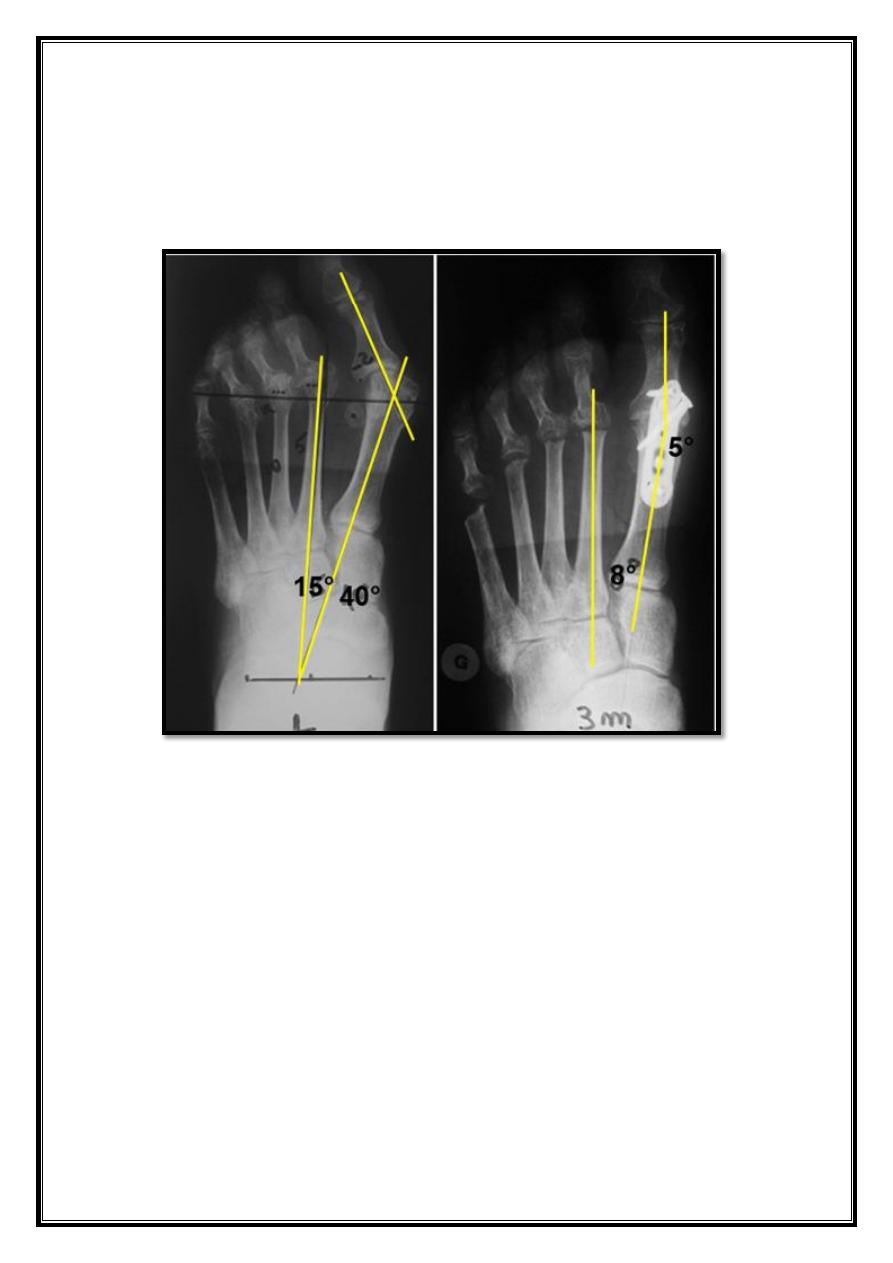
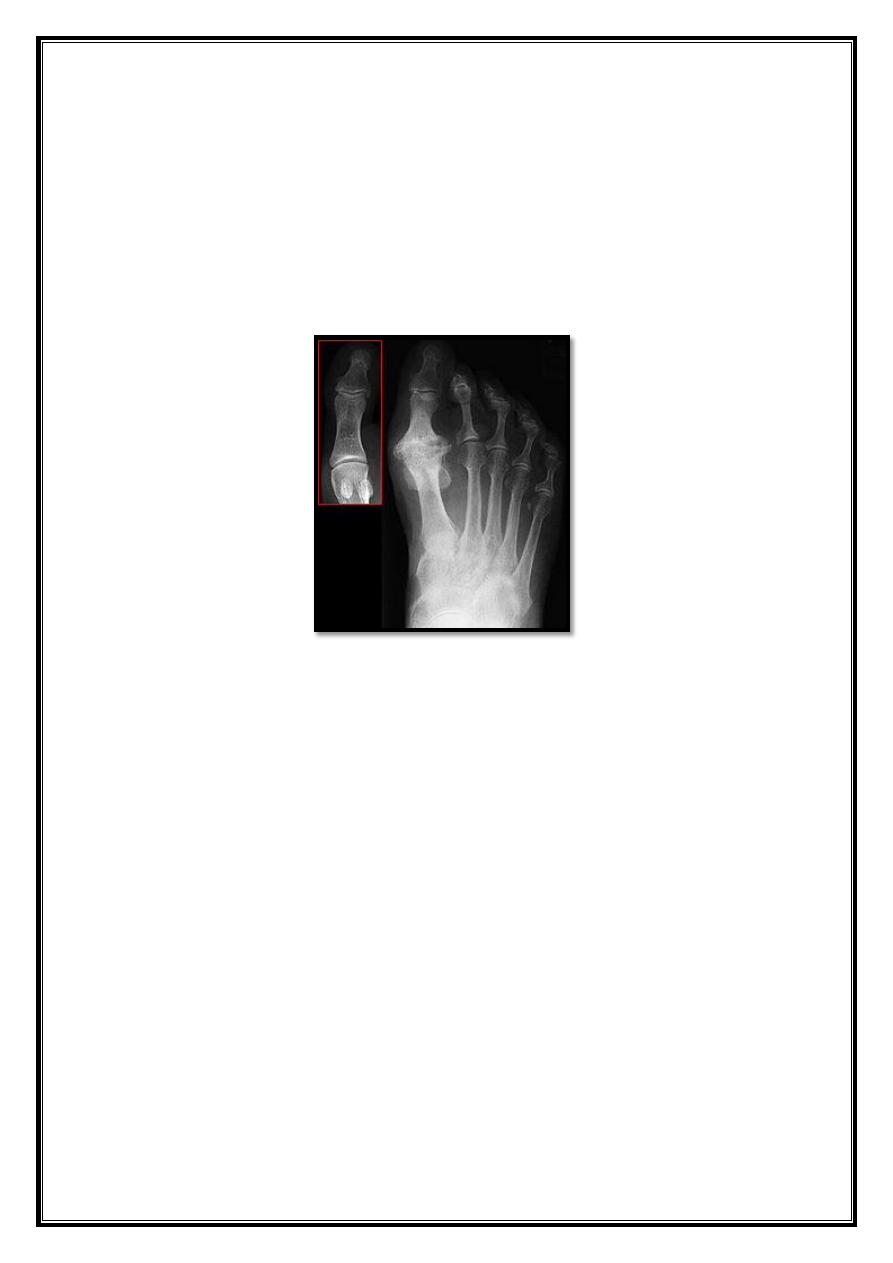
X-ray
Standing view:
- MPA (Metatarsal phalangeal angle) less 15D.
- IMA (Inter metatarsal angle) less 9D.
Treatment
- Conservative treatment: use wide shoes, protect bunion with felt.
- Operative correction:
For severe pain & disability There are
different soft tissue & bony procedures.
29
Hallux Rigidus
Rigidity & Stiffness of the first MTP joint of the foot .
Occurs at almost any age from adolescence onwards.
Men=women.
+ve family history
.
Is very often bilateral
.
Causes:
1. Repeated trauma.
2. Osteochondritis dissecans of the 1st metatarsal head.
3. Gouty arthritis &Pseudo gout of the 1st MTP joint.
4. O.A.
30
Clinical features
Pain on walking, especially on slops or rough ground.
On examination
MTP joint swollen, tender,
-
Dorsiflextion of the big toe is painful & limited.
-
Planterflextion also limited.
X-Ray
OA changes of the 1st MP joint of the foot.
Treatment
Conservative:
If the condition is not interfering with the activity it can be treated by
reassuring the patient and NSAID & local injection of corticosteroid.
Operative Treatment:
- Young patient: Extension osteotomy of the proximal phalanx
.
- Older patient: Excision of dorsal osteophyte.
- Joint replacement; using silastic prosthesis
.
- Arthrodesis: for patient engaged in heavy work
.
31
POSTERIOR HEEL PAIN
1. Traction apophysitis (Sever’s disease)
.
boys ,10 years, pain tenderness localized to tendoAchillis insertion.
2.
Calcaneal bursitis.
posterolateral portion of the calcaneum is prominent and shoe friction
causes reterocalcaneal bursitis .
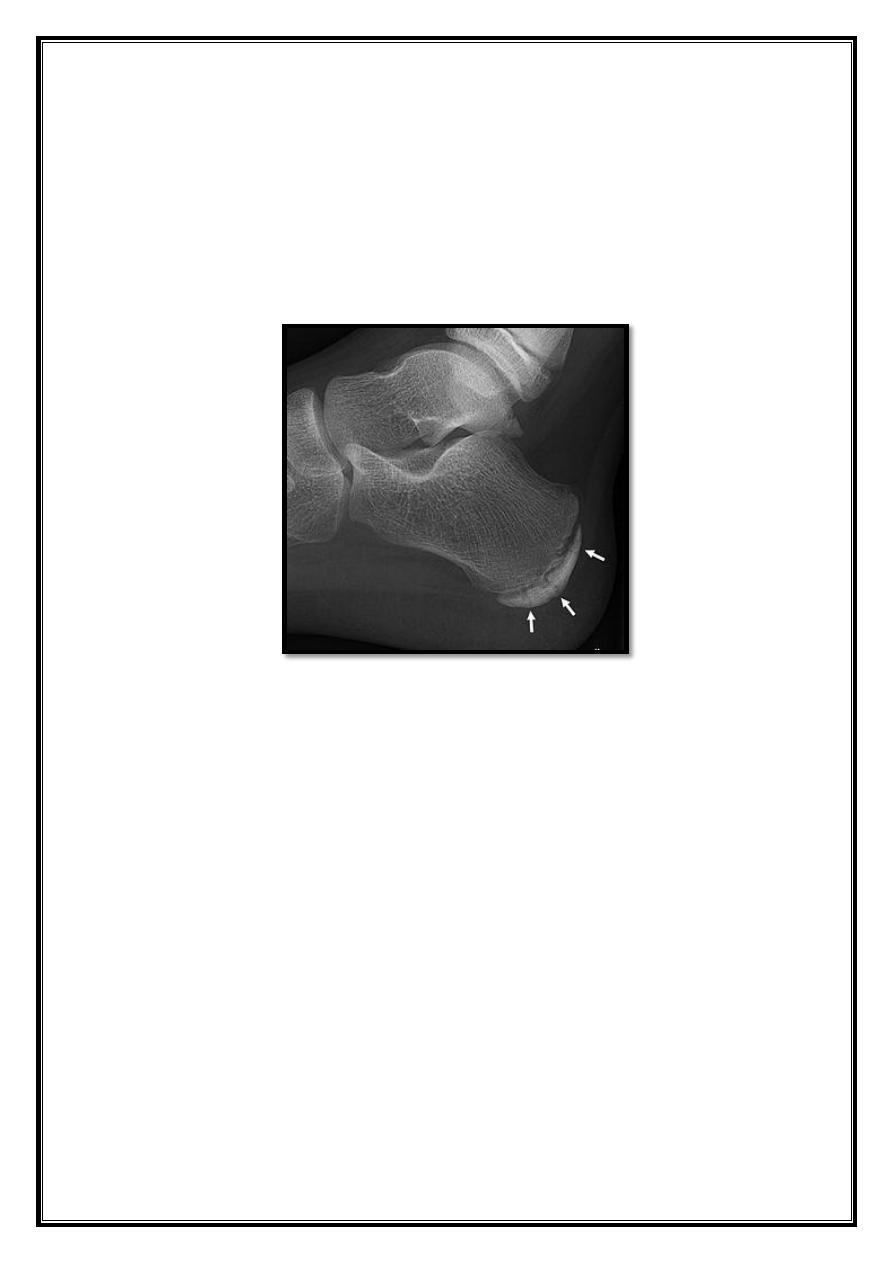
INFERIOR HEEL PAIN
Calcaneal bone lesion
- Stress fracture.
- Osteomyelitis
.
- Osteoid osteoma
.
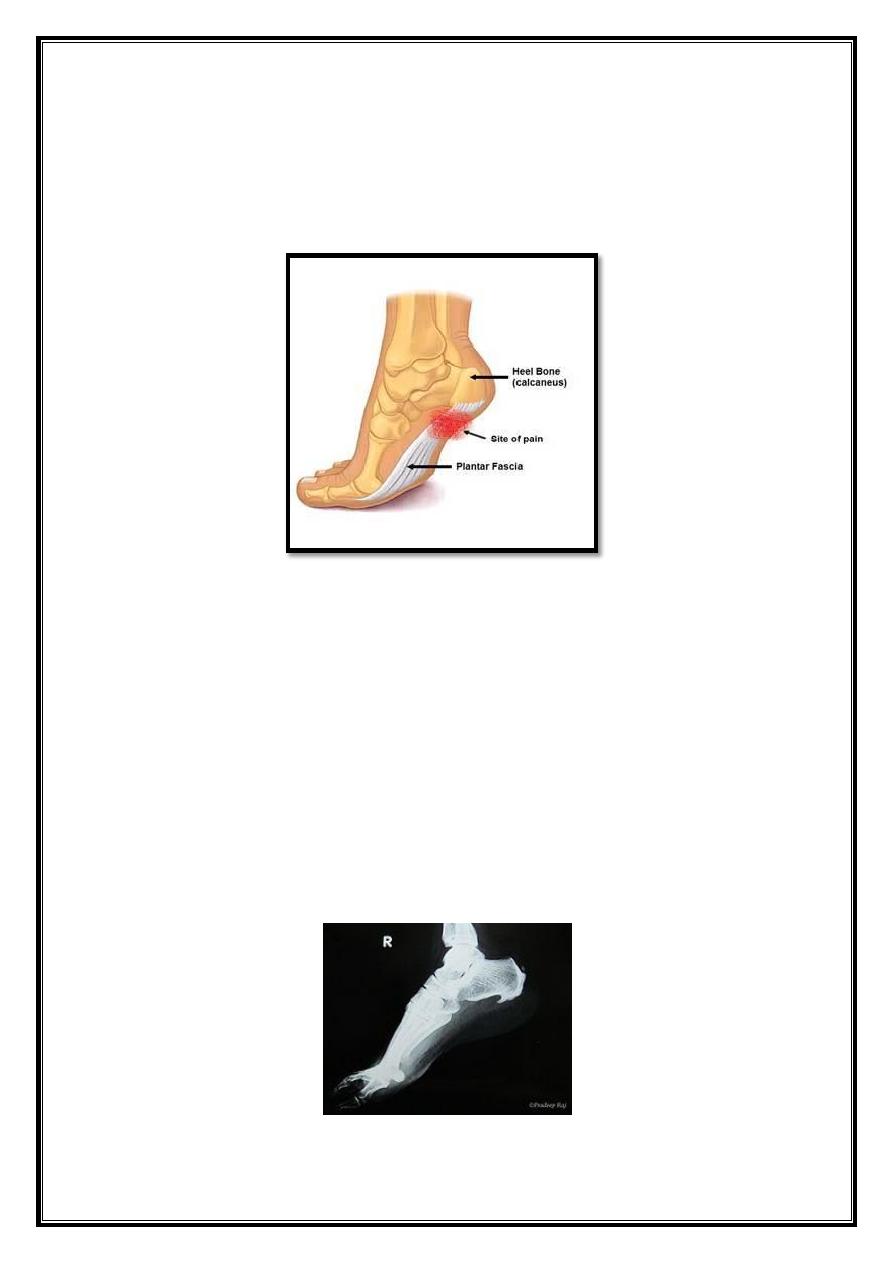
Planter fasciitis
.
32
Planter fascitis
Pain &tenderness in the sole of the foot mostly under the heel. The pain is
often worse when first getting up in the morning or when first getting up
from a period of sitting (startup pain &stiffness).
Sometimes associated with:
- Gout
.
- Ankylosing spondylitis
.
- Reiters disease
.
X-ray
- often show what looks like a bony spur undersurface of the
calcaneum.
- It is an associated not a causative.
- The condition can take 18-36 months or longer to resolve, but is
generally selflimiting.
33
Treatment
- Relative rest
& NSAIDs.
- An analysis of causative factors (footwear, sports and exercise).
Painful tarsus
Children:
- Kholer disease (osteochondritis of the navicular bone).
- The bony nucleus of the navicular becomes dense & fragmanted.
- Child under 5, painful limp, tender, worm and thickening over the
navicular.
Adults:
- High arched foot bony ridge at dorsum of medial cuneiform & 1st.
metatarsal.
Painful (Forefoot, metatarsalgia)
Generalized pain
Foot strain due to
- Faulty weight distribution
.
- Prolonged or unaccustomed walking.
Pain in MTPs
.
Localized pain
Sesamoiditis.
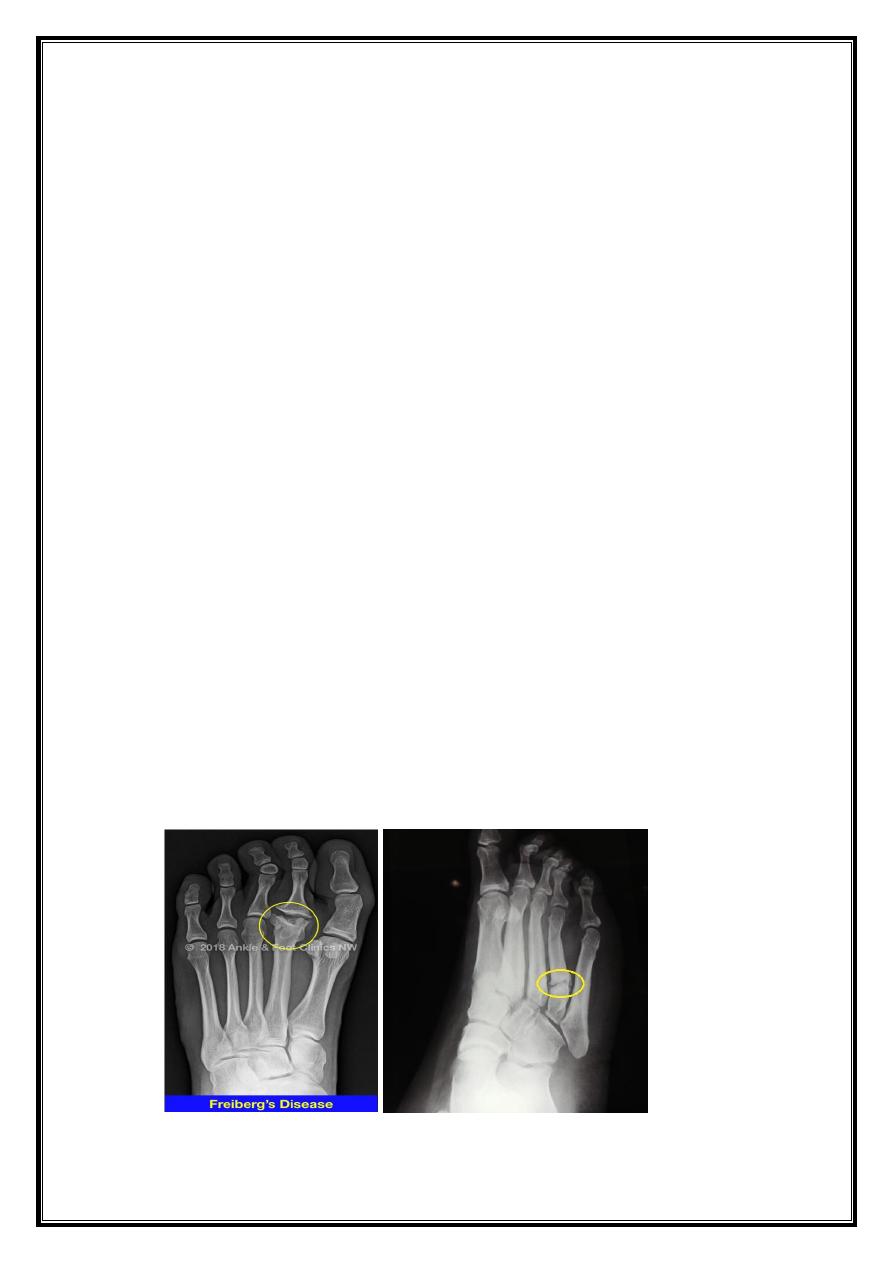
Freibergs disease
.
Stress fracture
.
Interdigital nerve compression (Mortons metatarsalgia)
.
Tarsal tunnel syndrome (compression of the posterior tibial nerve)
.
