Hepatobiliary system, spleen , pancreas
LiverUS :
Diagnosing focal & diffuse hepatic disease.Defining perihepatic fluid collection
Guidance liver biopsy procedure
Plain abdomen : Restricted uses in hepatic disease ( shows calcified foci in the liver & some time shows hepatic enlargement )
CT : is a superb investigation for most of liver pathology.
MRI; provide multidisplay information in great range of liver disease and may make successful diagnosis when other imaging modalities fail. It provides details of vessels and bile ducts with ever-increasing resolution. MRA being particularly helpful to a surgeon contemplating liver resection.
Radionuclide scanning:
Angiography : now more applicable to interventional technique and therapy ( e.g. embolization of vascular lesion & transhepatic portosystemic anastomosis-TIPS )
• Imaging techniques
Ultrasound of the liver :
Focal masses ( cysts , solid , mixed "complex ") masses
Cysts are echo free, have thin or invisible wall.
Solid or complex masses may be benign or malignant.
In practice its difficult to differentiate benign from malignant lesions unless the mass is clearly simple cyst.
When multiple solid or complex masses are seen within the liver , metastatic disease is likely diagnosis.
The prime differential diagnosis of multiple masses are multiple abscesses, regenerating nodules of cirrhosis of the liver and multiple haemangiomas.
Diffuse parenchymal diseases : such as diffuse chronic inflammation and diffuse neoplastic infiltration
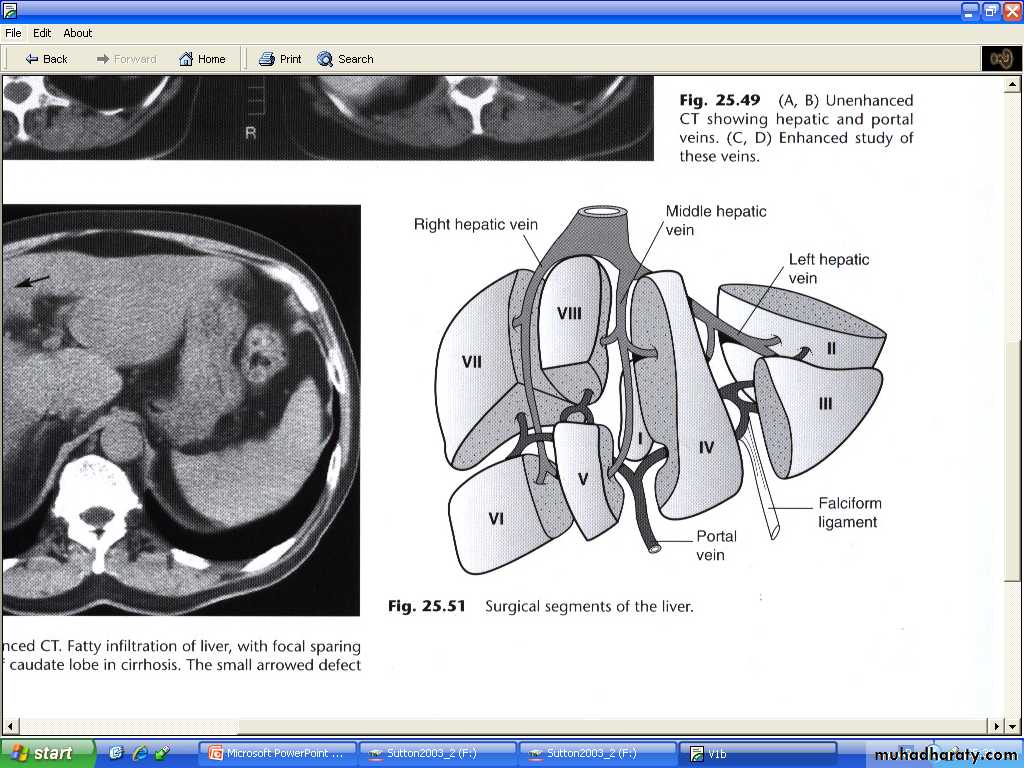
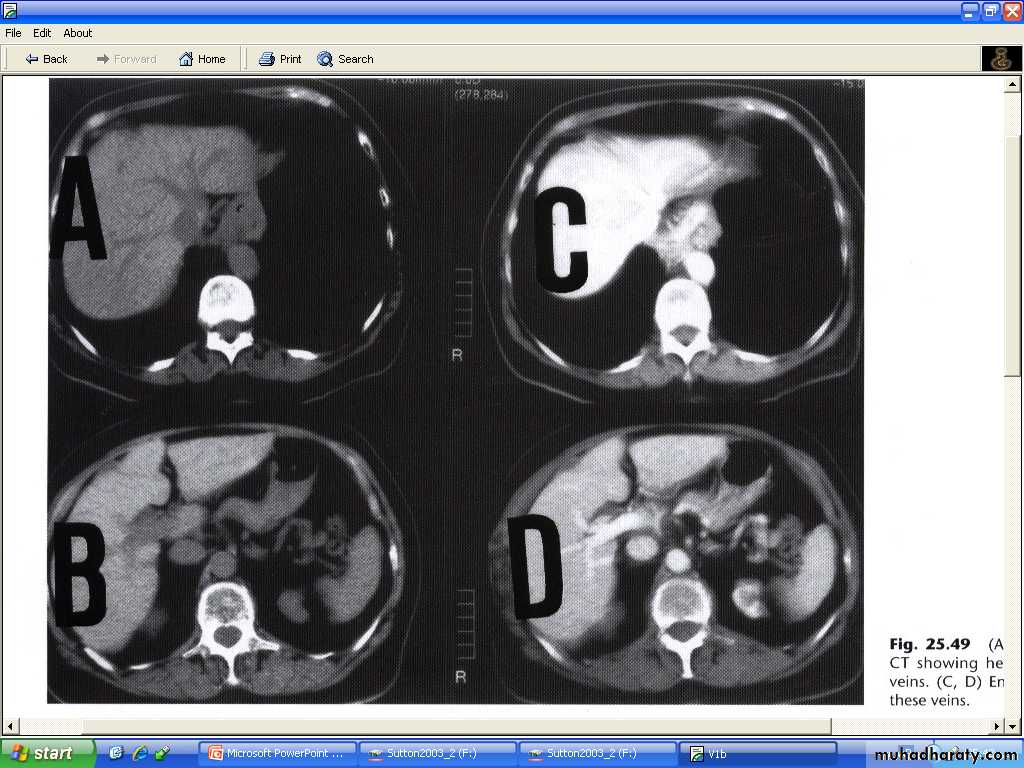
CT of the liver :
Native scan ( pre contrast scan )Post contrast scan –dynamic-triphasic liver scan (arterial phase "30 sec ", portal phase "60-70 sec " & delayed scan )
Most metastases are best demonstrated at portal phase as areas of low attenuation"hypodense" .
Scanning during arterial phase will shows lesions such as haemangiomas ( has typical enhancement pattern – discuss later ) and highly vascular metastases , as areas of grater enhancement than surrounding parenchyma
MRI of the liver:
Used as problem solving to give additional information to US and CT.Multiplanar imaging ( direct axial , coronal and sagittal views ).
IV contrast media ( gadolinium -) or new liver specific agent some are taken by hepatocytes and some taken by reticulo-endothelial cells .
Note : malignant tumors do not normally possesses hepatocytes or reticulo-endothilial cells , so there is heightened contrast between tumor and normal liver.
Liver masses :
1- Malignant liver neoplasm:Metastases are more common than primary tumors ( hepatoma and malignant lymphoma , both of which can be multifocal )
Metastases :
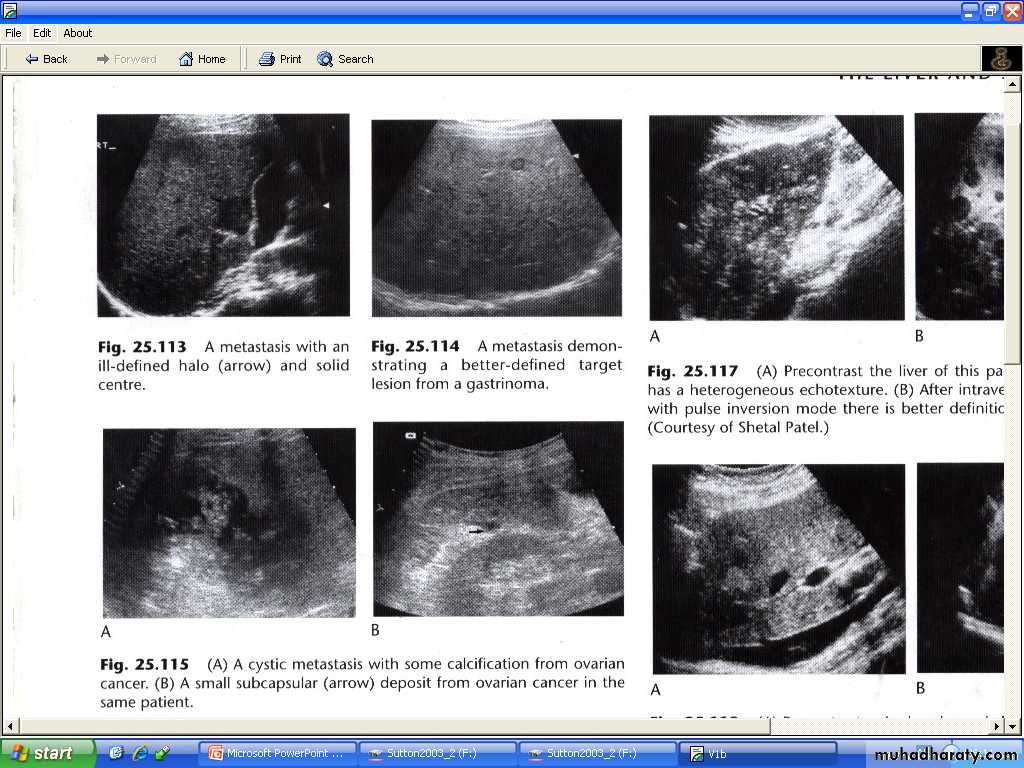
Often multiple , peripherally situated and variable sizes.
US
# may shows increase attenuation ( increase echogencity ) (echognic ) (hyperechoic ).
# more usually shows decrease echogencity ( hypoechoic ).
# At time , they show a complex echo pattern.
# When undergoes central necrosis they may even resemble cysts.
# may have an echogenic center giving an appearance described as a target lesion.
# some isoechoic to surrounding liver parenchyma ( i.e cannot be visualized sonographically )
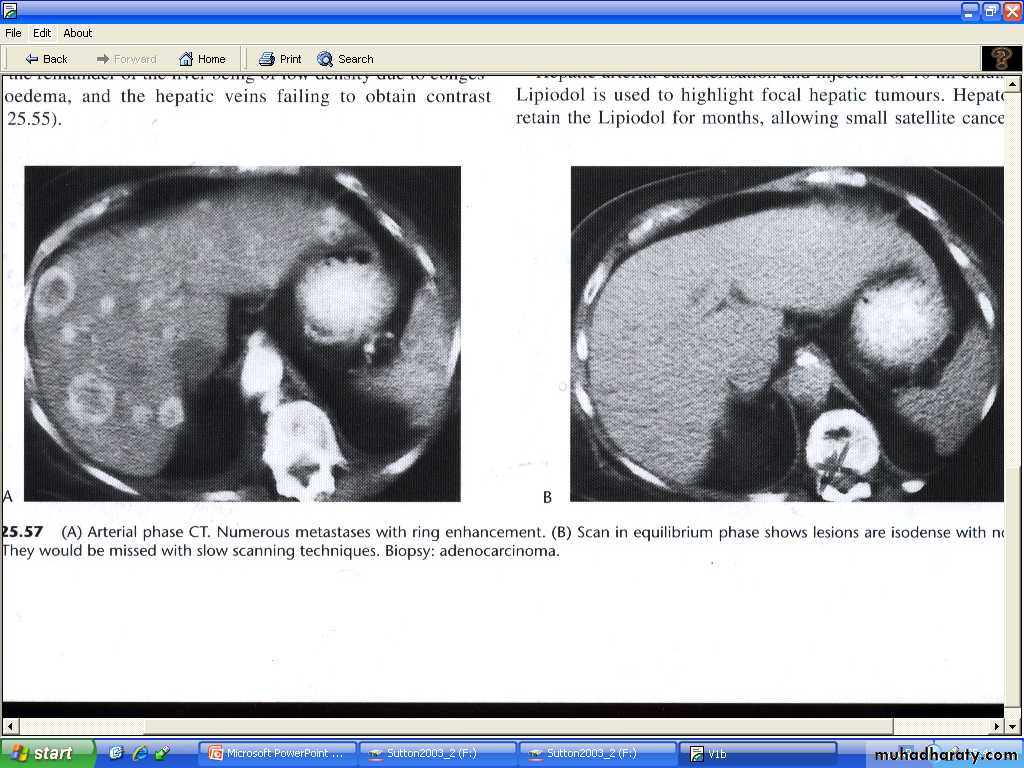
CT
# usually seen as lower density than the contrast enhanced surrounding liver parenchyma.
# intense contrast enhancement some time seen within the tumor or immediately surrounding them- a useful differentiating feature , which is not seen with cysts.
# some metastases ( e.g. carcinoid )are hypervascular and appear as high density areas.
MRI
# most shows lower signal than surrounding liver (hypointense) on T1-weighted scan and a high signal (hyperintense ) on a T2-weighted scan.
Primary carcinomas of the liver, which include hepatocellular carcinoma and cholangiocarcinoma are often large and usually solitary but they may be multifocal. CT, US and MRI features are similar to metastatic neoplasm
2- Benign liver masses :
- Most are cysts , some are haemangiomas . focal nodular hyperplasia are rare but can closely resemble malignant masses.- Liver cysts ;
Simple liver cysts :
# single or multiple , usually congenital , some due to infection.
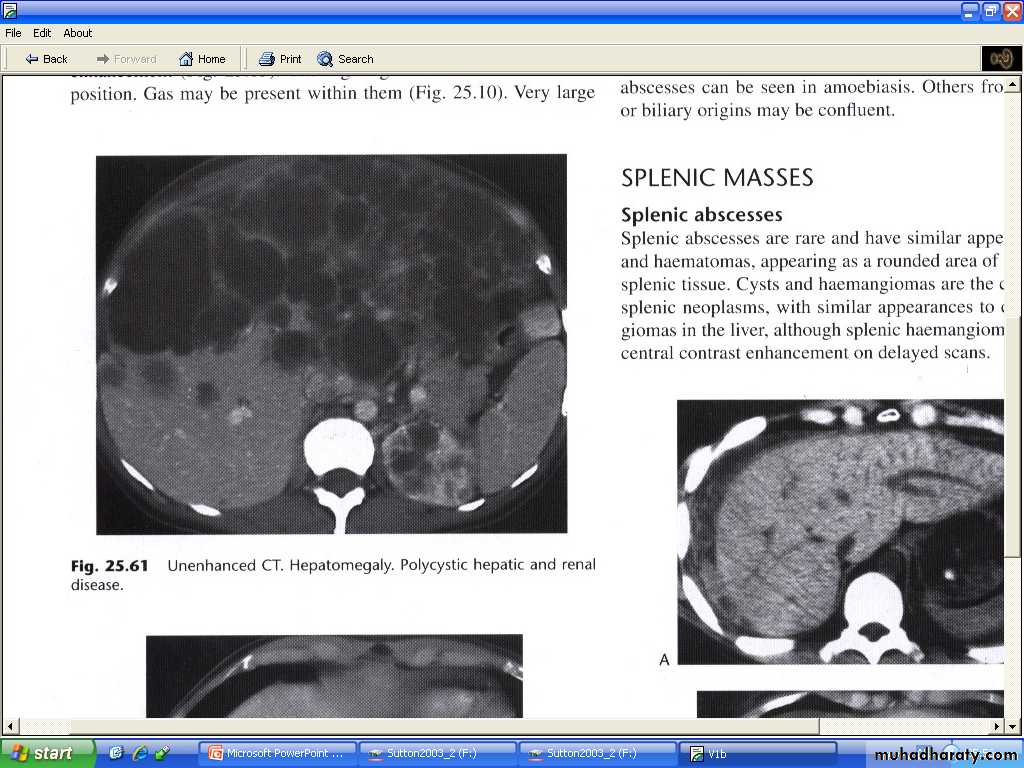
# multiple hepatic cysts occur in polycystic disease ( not only affect the kidney but may also affect the liver and other organs )
# at US : typical features of cysts elsewhere ( sharp margin , no echo within the lesion "anechoic", intense echo from the front and back walls with acoustic enhancement deep to the larger cysts.
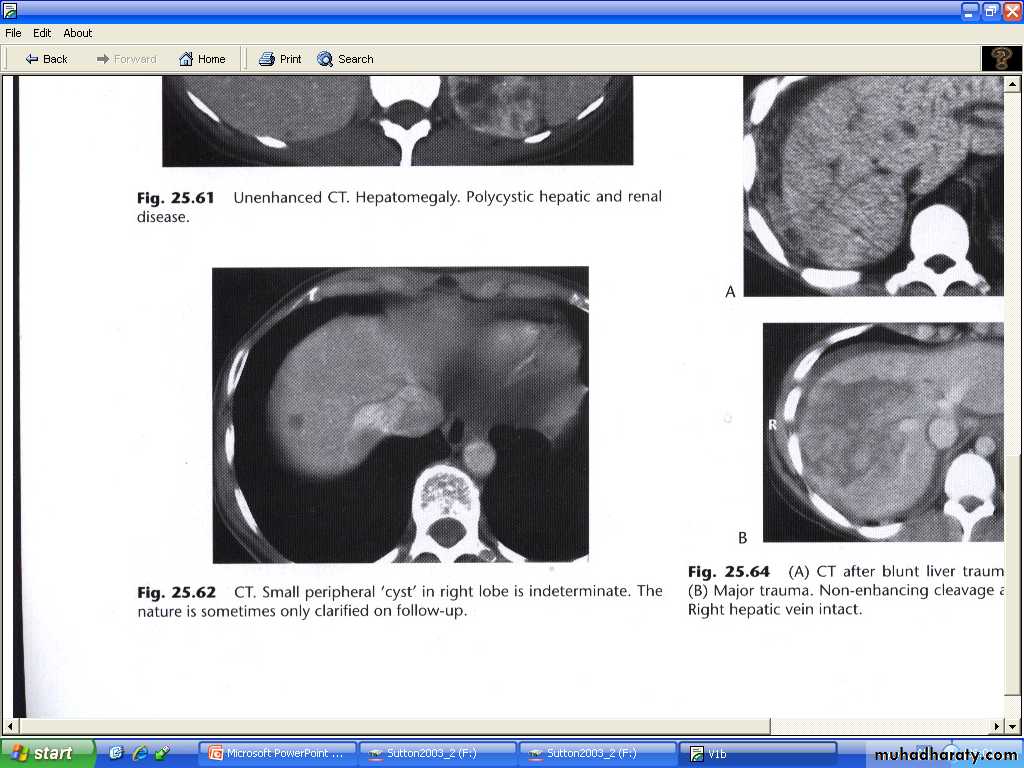
# at CT : very well defined margins , attenuation value similar to that of water (HU=0-15 ). Its often not possible to characterize small lesions and with lesions below 1 cm in diameter its almost never possible to distinguish cyst from neoplasm.
# at MRI : low signals on T1-W and high signal on T2-W
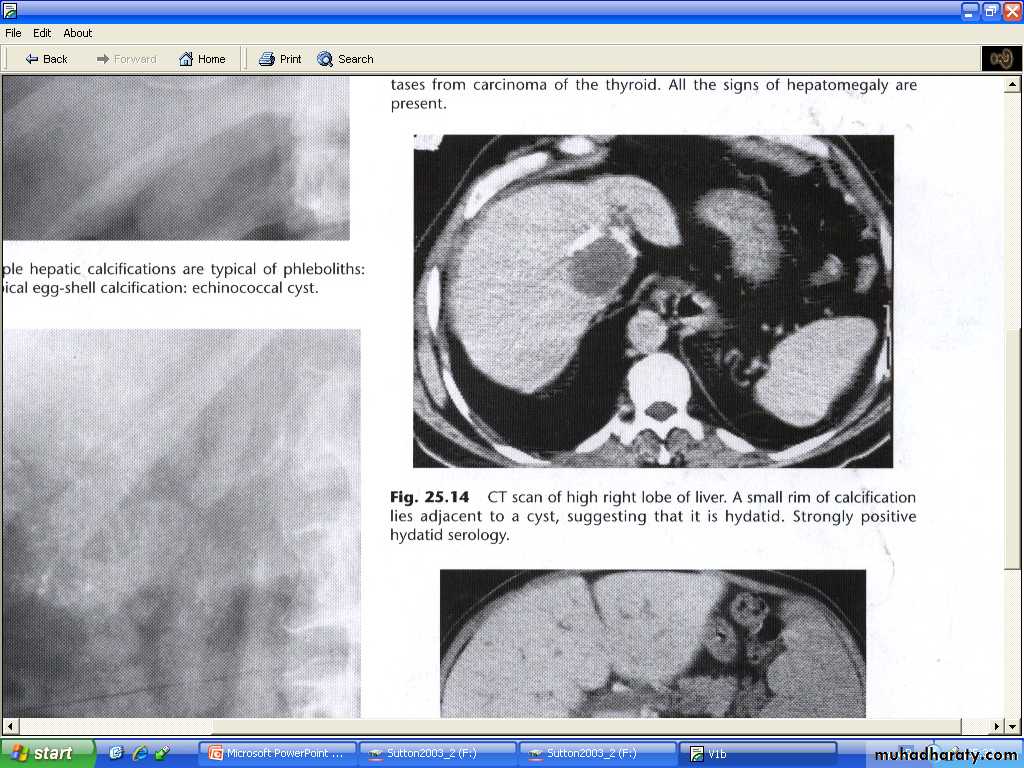
Hydatid cysts:
# may be single or multiple# some shows calcific wall, some shows daughter cysts and some shows internal undulating membrane (waterlily sign )
# unless these features are present ( some time H.cyst resemble simple cyst criteria), H cysts may prove indistinguishable from simple cysts at both US and CT
# Response to medical therapy include : reduction in size of cyst , membrane detachment , progressive increase in cyst reflectivity, and wall calcification.
Occasionally metastases can have a cystic appearance.
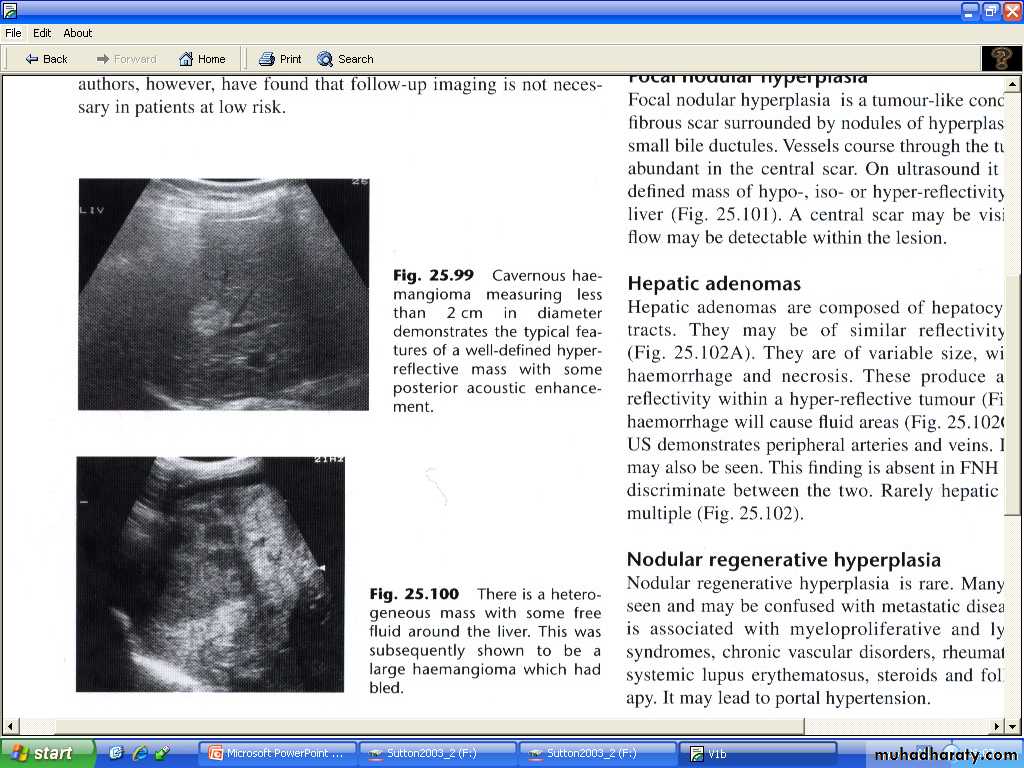
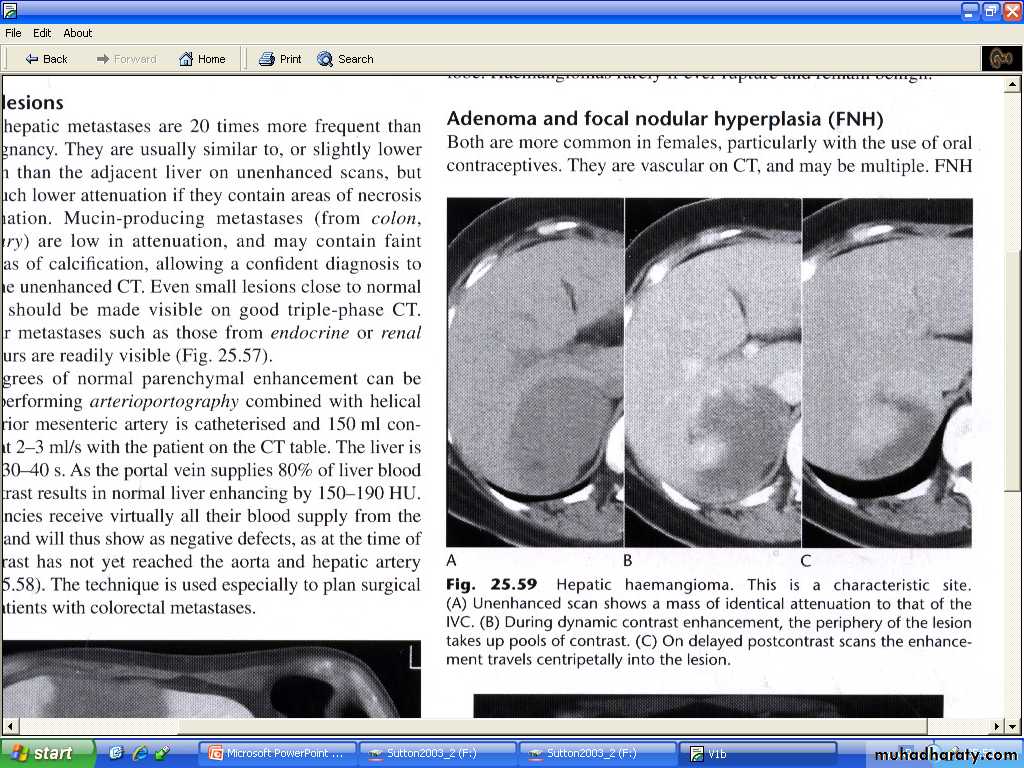
Haemangiomas of the liver
Often incidental finding, single or multiple , occasionally can cause significant hemorrhage , especially following trauma therefore percutanous biopsy should be avoided.Resemble neoplasm and other masses at US , usually hyperechoic and well defined .
At native CT scan : appears rounded low density.
On dynamic Post contrast CT or MRI : early shows nodular peripheral nodular enhancement , slow centrepital filling on next few min scan then became similar to surrounding liver.
Giant haemangiomas : >6 cm shows central irregular necrotic non enhancing core.
Small haemangiomas : <1 cm may give similar post contrast features to other liver masses and cannot be differentiated.
On MRI shows uniform very high intensity on T2-W , a characteristic that is shared with benign cysts , but very unusual with malignant neoplastic lesions.
Adenoma and focal nodular hyperplasia
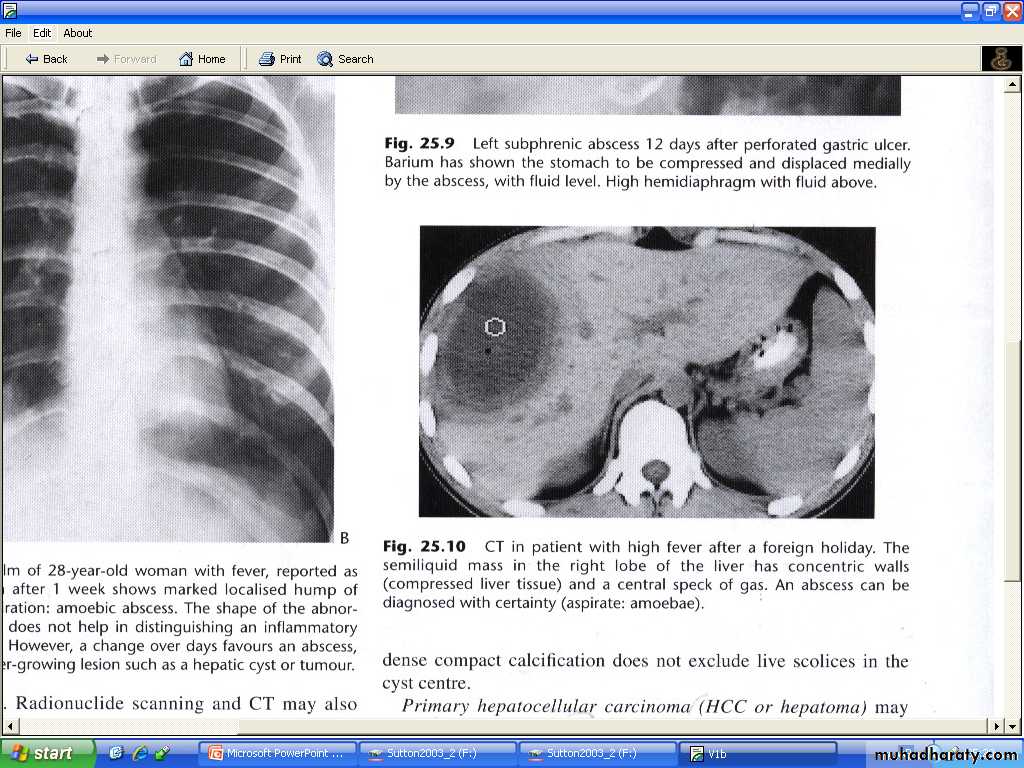
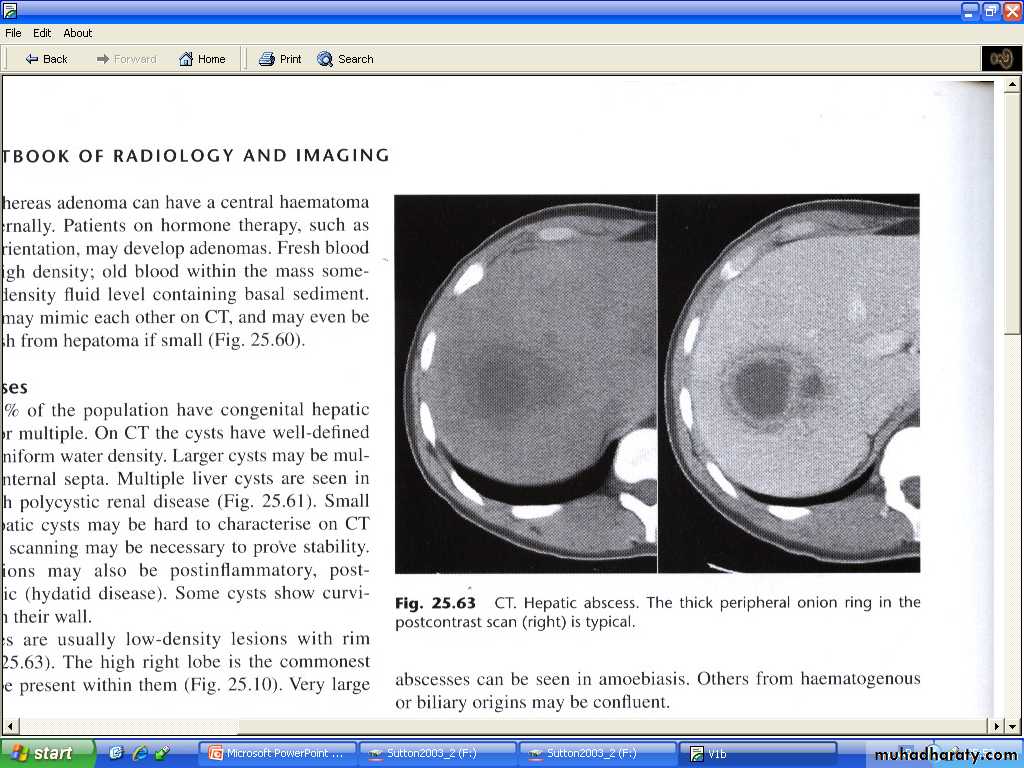
Both of these conditions appear as enhancing masses on CT.Liver abscess :
Hepatic abscess tend to have fluid centers , with walls that are thicker , more irregular and more obvious than those of simple cysts.At CT : the core fluid have attenuation values may be same as water , usually they are higher .
At US : necrotic debris may be seen within the abscess.
Occasionally chronic abscess calcify.
Abscess cannot usually be differentiated from necrotic tumor by US,CT or MRI, clinical situation should be aid in distinction.
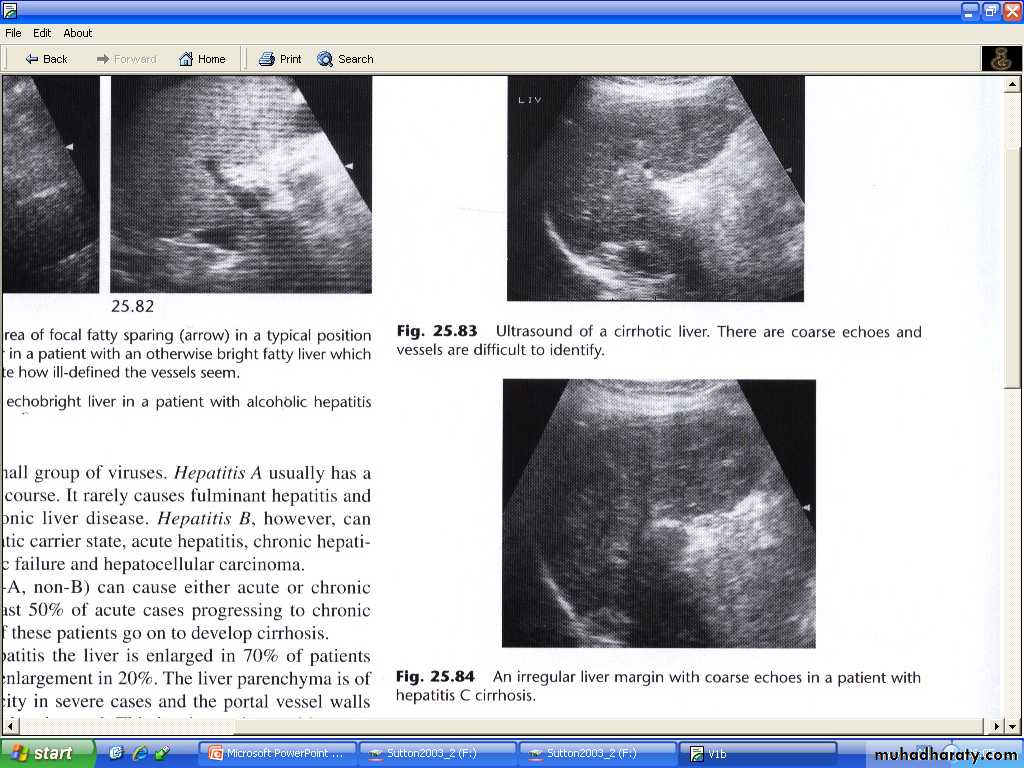
Cirrhosis of the liver and portal hypertension:
In portal HT the pressure of portal venous pressure is elevated due to obstruction to the flow of blood in the portal or hepatic venous systems.Cirrhosis of the liver is by far the commonest cause.
Other causes include occlusion of hepatic veins (Budd-Chiari syndrome ) and thrombosis of portal veins, particular following infection of the umbilical vein in neonatal period.
Portosystemic anastomosis collateral may follow to enter the vena cava by passing the liver , the most important of these are varices at lower esophagus. And these can be shown with color Doppler US.
The signs of cirrhosis of liver at CT and US are reduction in the size of Rt lobe of the liver and irregularity of liver surface , together with splenomegaly .
Ascites may be present.
Liver texture at US may be diffusely abnormal while on CT appears normal until late in the disease.
Patency of splenic , portal and hepatic veins can be assessed with Doppler US , CT or MRI.
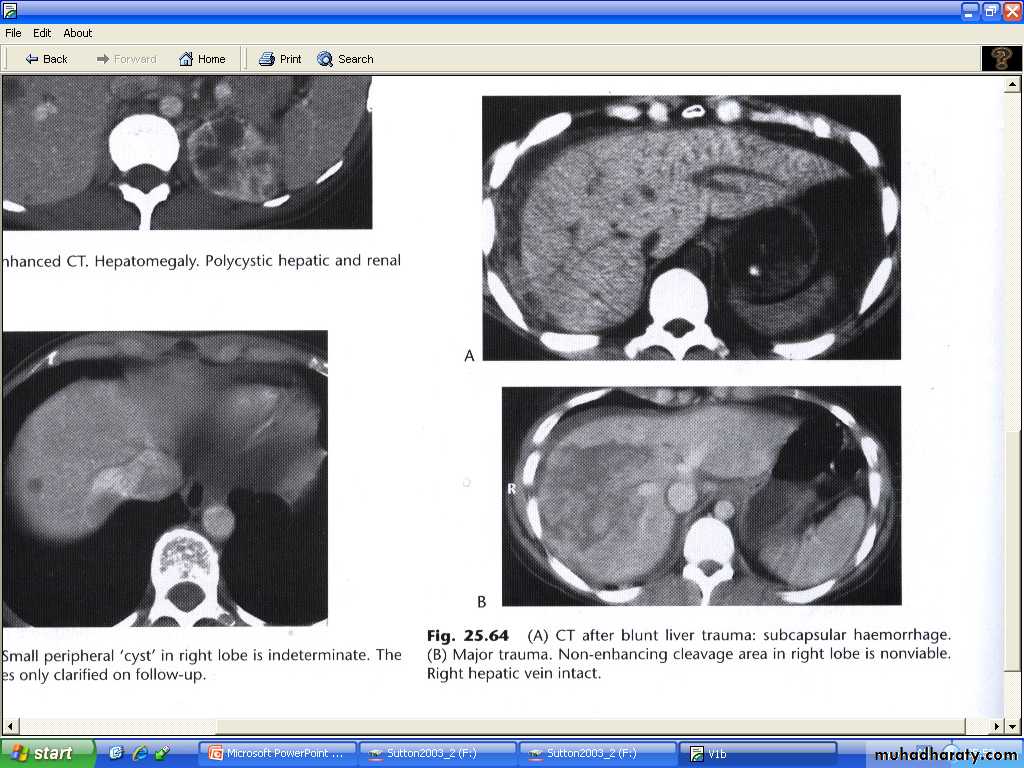
Liver trauma :
Is the commonest abdominal injury that leads to death.Features are : parenchymal lacerations , subcapsular and intrahepatic haematomas.
Lacerations and haematomas are recognized as low density areas relative to the contrast enhanced parenchyma , leakage of contrast indicate active bleeding .
Although US and MRI can demonstrate liver injury , CT is the best technique, which can survey other organs like spleen and kidneys. And identify any peritoneal fluid collection.
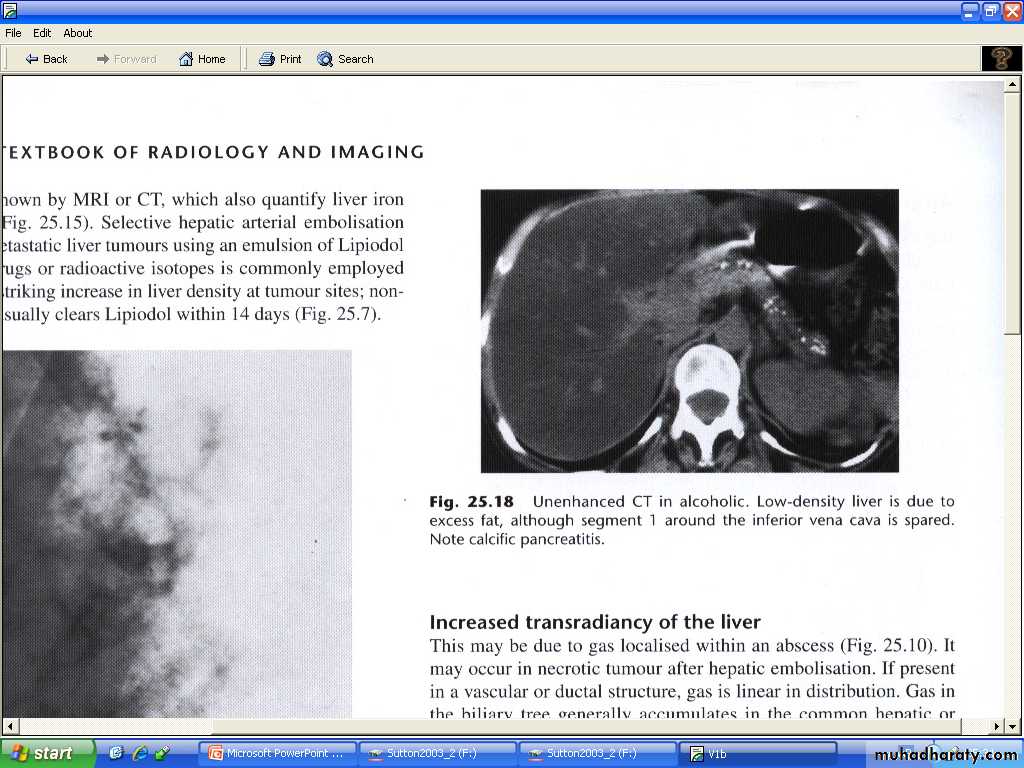
Fatty degeneration ( or infiltration ) of the liver :(steatosis )
Commonly seen in patient with diabetes mellitus and alcoholics. other include obesity, hyperlipedaemia , parentral nutrition, severe hepatitis and chemotherapy.On US :causing increase liver reflectivity (bright liver ), poor definition of posterior liver and hepatic veins . the liver will be enlarged in 75-80%.
On CT appear as reduction of attenuation (low density) , and vessel more prominent (due to reduction of back ground of parenchymal density )
MRI can be very helpful because fat gives characteristic set of signals.
Fatty infiltration may be diffuse , focal , or diffuse with focal sparing areas.
Viral hepatitis :
In acute viral hepatitis the liver is enlarged in 70%, splenic enlargement in 20% of cases.By US : liver parenchyma usually normal and decrease echogencity in severe cases and portal vessels more echogenic than normal. GB wall thickened may also be observed.
In Sever chronic hepatitis there is increase echogencity of the liver parenchyma undifferentiated from fatty infiltration ,
Biliary system :
Imaging investigations:
US : is the best and primary method of investigation ,because simplest and excellent method in showing gallstones and diseases of gallbladder also an excellent test for confirming or excluding bile duct dilatation. patient should be fasting 6—8 Hrs prior to procedure to fully distend the GB .
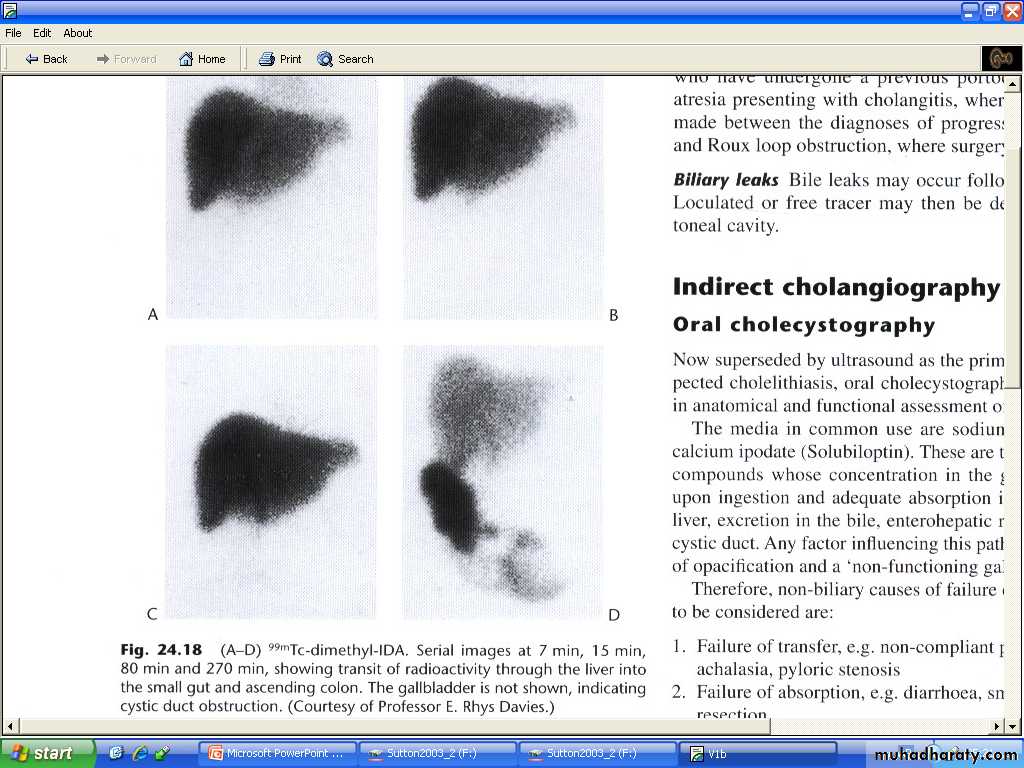
Radionuclide imaging using hepatobiliary agents ( e.g. 99m TC-HIDA ). Hepatic excretion occurs despite relatively high serum bilirubin levels, and, therefore, these agents can be used when the patient is jaundiced, even with serum bilirubin levels of up to 250 μmol/L (15 mg%). The main use of this technique is in patients with suspected biliary leak following biliarysurgery. The technique may also be used in acute cholecystitis (with nonfilling of the gall bladder in cases of an impacted stone in the cystic duct) or in children, when biliary atresia is suspected.
CT: GB wall thickening , gall stones and dilatation of common duct all can be recognized at CT , but US produced better information , because pure cholesterol stone density may approach that of fat and difficult to appreciated with CT.
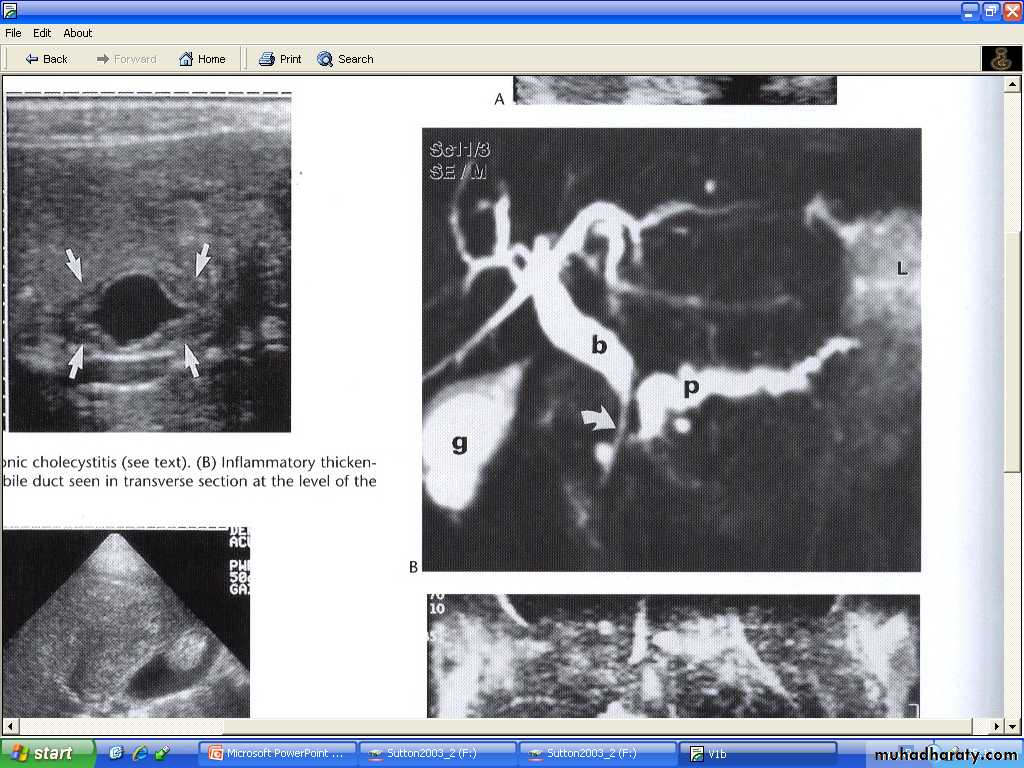
MRI and MRCP : excellent in visualization of biliary radicles , equivocal US and CT results and may be diagnostic in non dilating biliary disorders .the examination is non invasive and no contrast needed .
PTC ( percutanous cholangiography ): reduced now a day as a diagnostic method & mostly replaced by ERCP &MRCP is generally performed if an
- ERCP is unsuccessful in treating a distal common bile duct
(CBD) obstruction or
as the primary procedure in treating a more proximal hilar stricture.
Chiba needle under fluoroscopic or US guide. With local anesthesia
Haemorrhage is an occasional problem,as are septicaemia and biliary peritonitis.
ERCP : advantage is biliary & pancreatic ducts are studies , allow direct inspection and biopsy of papilla and duodenum & therapeutic procedure of sphencterectomy & stone extraction , endoscopic basket or balloon extraction & stint placement.
It is still occasionally used for more detailed imaging of the intrahepatic biliary ducts as resolution is better than with MRCP (e.g. in sclerozing cholangitis). Pancreatitis is an occasional complication of ERCP.
Operative cholangiography . & post-operative T-tube cholangiography.
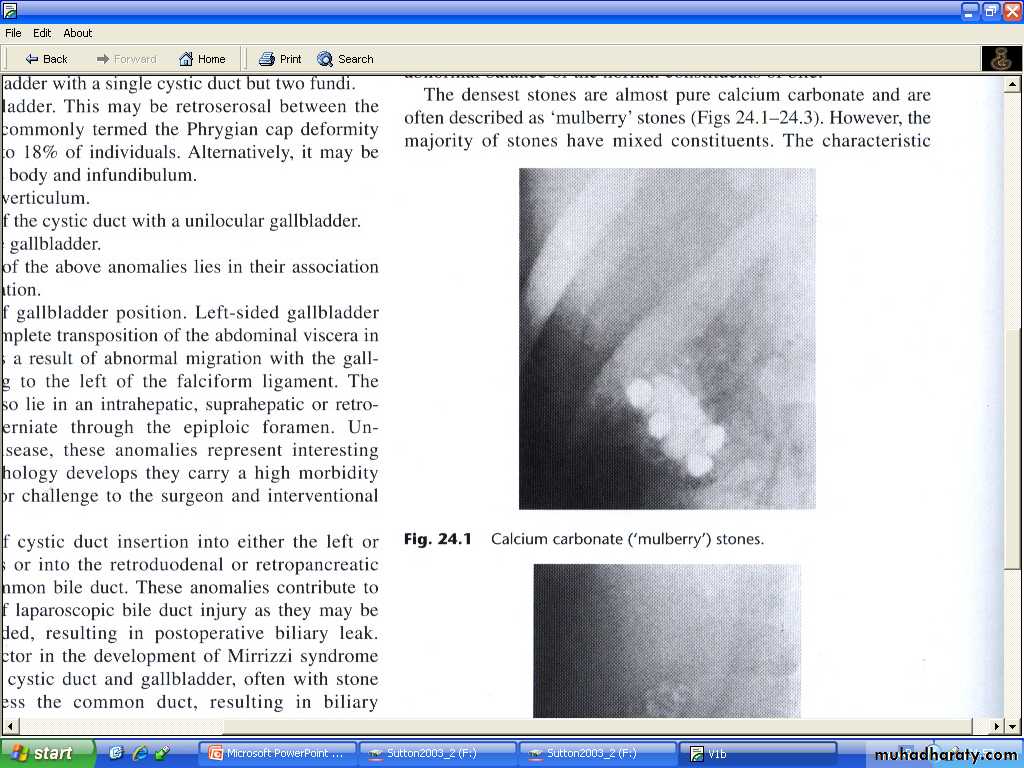
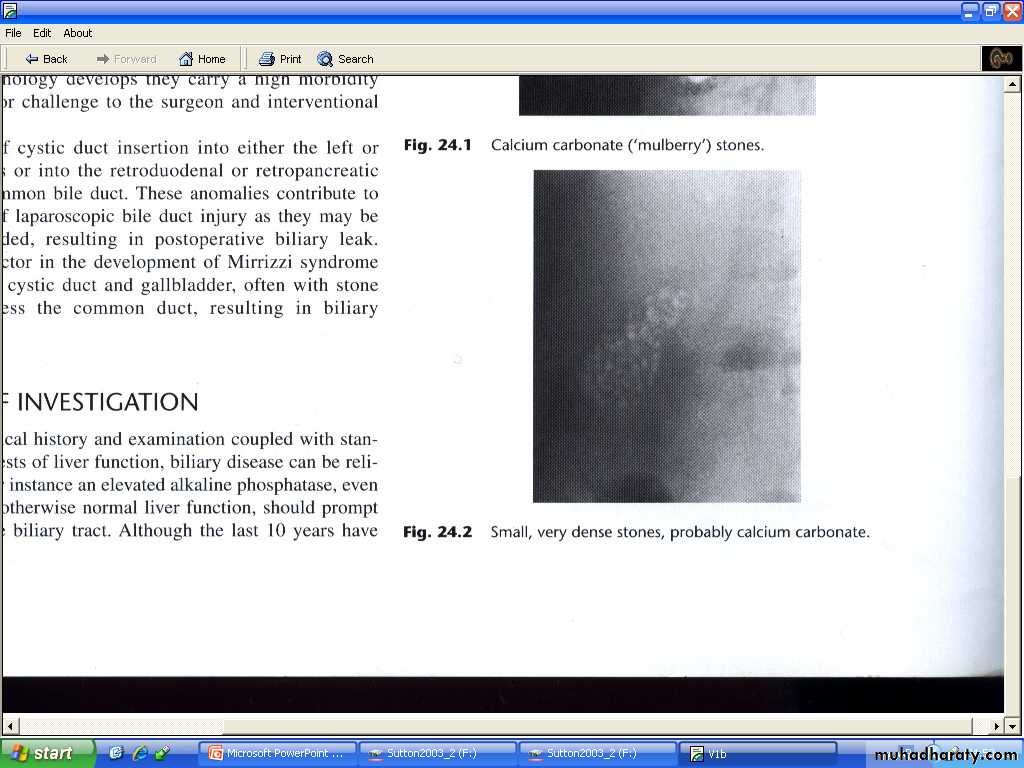
Gall stones and cholycystitis :
Gall stones are frequent finding in adults , particularly in middle age female. Together with accompanying chronic cholecystitis they are a major cause of recurrent upper abdominal pain .20% of gall stones contain sufficient calcium to be visualized by plain film.
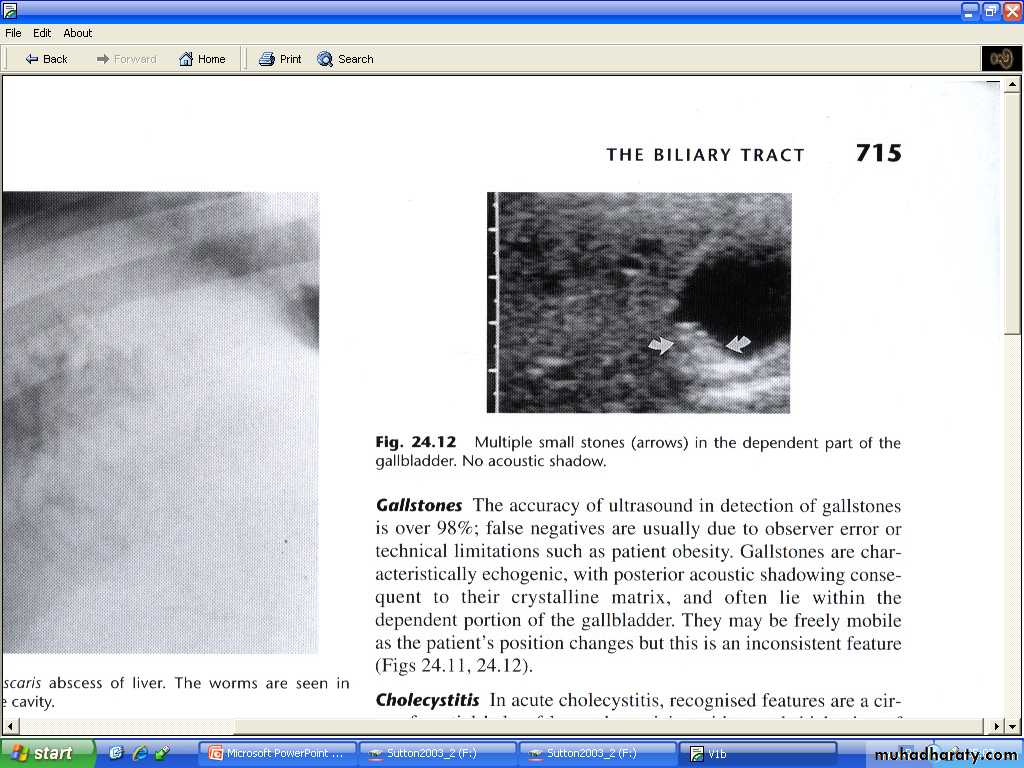
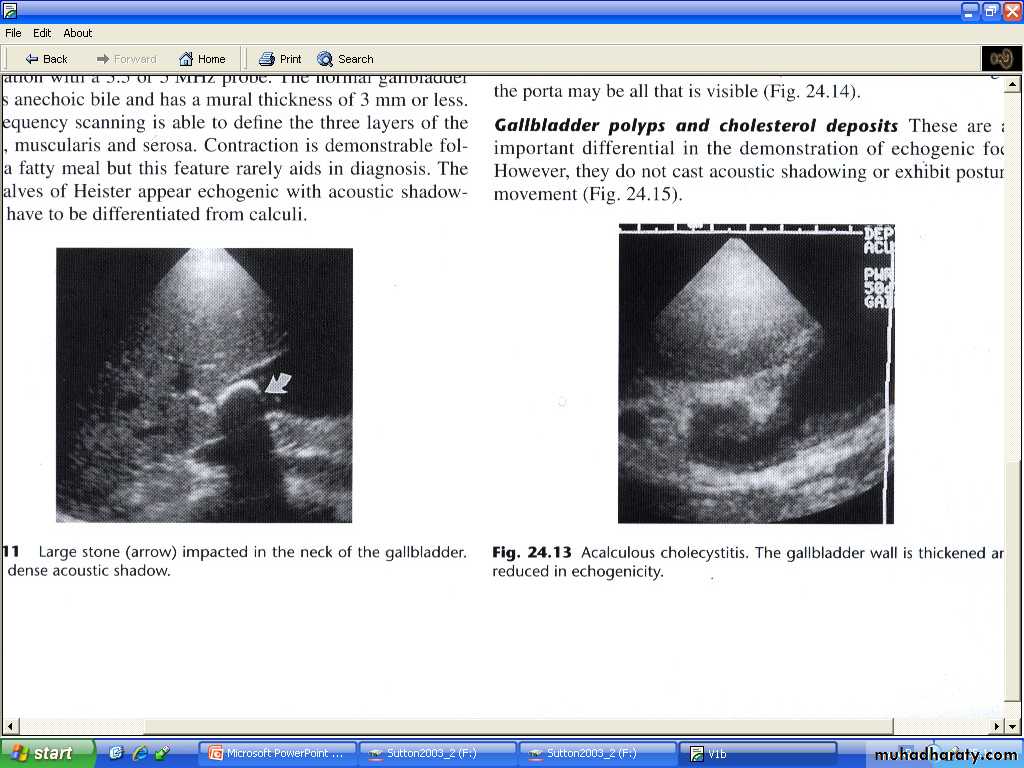
At ultrasound , gallstones are seen as a strongly echogenic foci within the dependant portion of gall bladder . acoustic shadow usually seen behind stones..
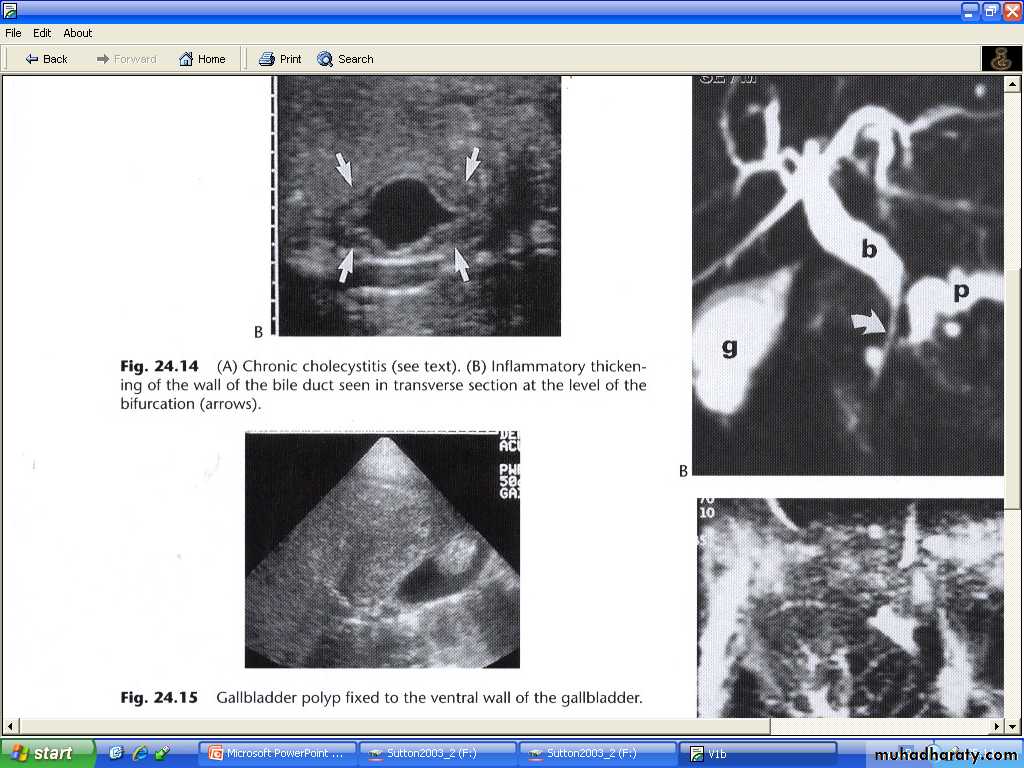
Acoustic shadows is an important sign, not seen with polyp. Most polyps are small measuring only few millimeters and are not neoplasms but aggregation of cholesterol.
US very accurate in detecting gall stones but less reliable for detecting stones in the common bile duct.
Calculus cholecystitis :
In acute cholecystitis , sonography will usually detect gall stones , inflammatory debris "biliary sludge" and gall bladder wall thickening .Unless there is visible edema adjacent , ultrasound cannot distinguish acute from chronic cholecystitis. In acute cholecystitis pain is often localized to gallbladder (ultrasonic Murphy sign). Also in chronic cholecystitis the GB is contracted.
No available test to be very good in diagnosing gallbladder inflammation , but since the cystic duct is always obstructed in acute cholecystitis , a normal hepatobiliary radionuclide scanning exclude the diagnosis.
An empyemia or mucocoele may results if there is continuing cystic duct dilatation.
Perforation may results give rise to localized abscess or biliary peritonitis.
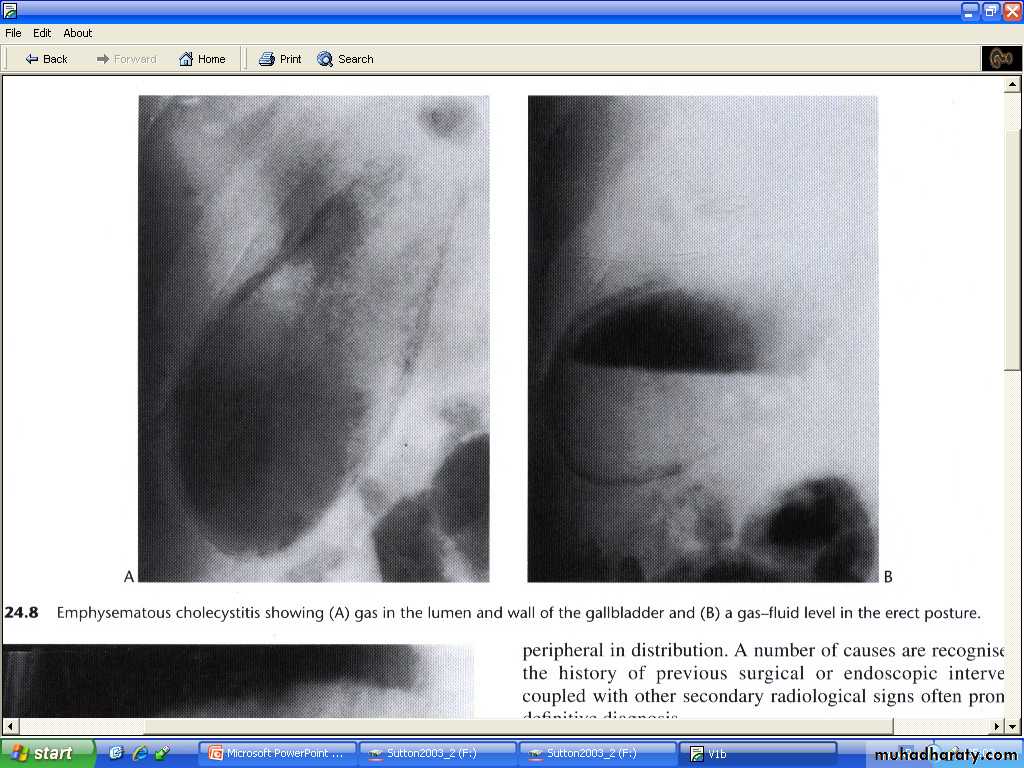
Infection with specific coliform organism or clostridium welchii may resuls in emphysematous cholecystitis , particularly in patient with DM and immunocompramized with mural air seen on plain abdomen or CT.
Fistulation may occur to small or large bowel with associated enteric obstruction termed gallstone ileus.
Jaundice:
Imaging test may be required when there is doubt as the nature of jaundice.The basis of this distinction is that dilated biliary ducts are a feature of jaundice from biliary obstruction.
Most often the imaging is used to determined the site and possible cause of such obstruction.
The causes of large duct obstruction :
- Impacted stone in the common bile duct.
- Carcinoma of the head of pancreas.
- Carcinoma of ampulla of vater
Dilatation of the intra- and extra-hepatic biliary system can be identified at both US and CT. US is more sensitive test and is usually the 1st test to be performed.
The CBD located just infront of portal vein and is dilated when more than 7 mm in diameter ( some books 8 mm , and range of 6—8 mm is equivocal , vey rarely normal ducts seen up to 12 mm , especially in post cholectectomy , elderly )
More often the cause of obstruction cannot be seen because of overlying gas in duodenum especially in distal portions.
CT may be helpful in such cases but MRCP is exceedingly better.
Substantial dilatation of common hepatic and CBD may be present with only minimal dilatation of intrahepatic biliary ducts & also the intrahepatic biliary tree may not dilate at all within the 1st 48 Hrs following obstruction.
ERCP provide excellent diagnostic & interventional procedure in obstructive jaundice.
MRCP- stricture cholangiocarcinoma