1
L4. Acute Rheumatic Fever (RF)
It is a delayed sequela of group A beta-hemolytic streptococcal (GAS) pharyngitis as
immunological reaction to the infection.
It is rarely followed skin infection by GAS and it is commonly affect children between 6
and 15 years of age.
It is the most common acquired heart diseases in all age groups, accounting for about
50% of all cardiovascular diseases. Its commonly occurs in overcrowded and poor
communities and there might be genetic predisposition for rheumatic fever.
Clinical features:
Acute RF typically develops 2-4 wk after the acute GAS pharyngitis, and the disease
characterized by high rate of recurrence after the initial attack of acute RF.
The diagnosis of RF is done by revised Jones criteria which consist of 5 major and 4
minor criteria PLUS the evidence of recent GAS infection.
Major criteria:
1. Migratory polyarthritis:
Is the earliest manifestation of acute RF, occurs in about 75% of all patients. It typically
involve the large joints (knees, wrists, and elbows) while the involvement of spine, small
joints of hands and feet or hip is uncommon.
The affected joint is hot, red, swollen and extremely tender that the patient is not
tolerate even the friction of bed sheets. These manifestations may preceded by sever
joint pain (arthralgia).
The arthritis is non-deforming (completely resolve without residual joint destruction) and
have dramatic response to NSAID (salicylates).
The arthritis is characteristically migratory in nature, that mean the affected joint
become normal within 2-3 days without treatment, while one or more other large joints
become involved.
Monoarticular arthritis is unusual unless the salicylate is prematurely used during the
early course of acute RF which stop the progression of migratory arthritis.
2. Carditis:
It occurs in about 50% of all cases of acute RF. It’s either subclinical carditis
(echocardiac evidence of valvulitis but without murmur) or clinical carditis
(echocardiac evidence of valvulitis plus new cardiac murmur).
It is the most serious manifestation of acute RF and it characterized by pancarditis
(inflammation of pericardium, myocardium and endocardium “valvulitis”) and the
endocarditis (valvulitis) is universal finding in rheumatic carditis, whereas the presence
of pericarditis or myocarditis is variable.
Presence of myocarditis and\or pericarditis without clinical evidence of endocarditis
(Valvular disease) it is almost never rheumatic heart disease.
The most common rheumatic heart disease is isolated mitral regurgitation or combined
aortic and mitral regurgitations.
Clinical manifestations of carditis include tachycardia, new murmur (aortic or mitral
regurgitation), pericarditis, cardiomegaly and signs of congestive heart failure.
2
3. Chorea “Sydenham Chorea”:
Occurs in 10-15% of patients with acute RF and usually presents as isolated, subtle
movement disorders.
It characterized by emotional liability, incoordination, poor school performance,
uncontrollable movements and facial grimacing. These manifestations are exacerbated
by stress and disappearing with sleep.
The latent period between the acute GAS infection and chorea usually longer than that
for arthritis or carditis and it might be as long as months (so it usually presents as
isolated manifestation) and it rarely lead to permanent neurological sequelae.
Examination methods of chorea:
1.
Milkmaid’s grip: irregular contractions and relaxations of fingers muscle while
squeezing the examiner’s fingers.
2. Spooning and pronation of the hand while the arms extended.
3. Warmian darting movement of the tongue on protrusion.
4. Examination of hand writing for fine motor movements.
Diagnosis of chorea based on clinical examination and raised GAS antibody titers, but
because of the prolonged latent period between the GAS infection and onset of chorea,
the antibody titers may return to normal levels.
4. Erythema Marginatum:
It is rare manifestation of acute RF occurs in about 1% of all cases, consist of
nonpruritic erythematous macular rash with pale centers and serpiginous borders,
occurs on the trunk and extremities (but not on the face) and it accentuated by local
heat application.
5. Subcutaneous nodules:
It’s rare manifestation (<1%) seen predominantly with chronic or recurrent RF. They are
firm, painless, nonpruritic, mobile nodules found on the extensor surfaces of the large
and small joints, scalp and spine.
There’s a correlation between the presence of these nodules and significant rheumatic
heart disease.
Minor criteria:
1. Arthralgia ((joint pain without physical signs of arthritis)), it used as minor criteria
only if the arthritis is not used as major criteria.
2. Fever (38.2-38.9 C).
3. Elevated acute phase reactant (ESR, C-reactive protein or leukocytosis).
4. Prolonged PR-interval on ECG ( unless the carditis is a major criteria).
Evidence of recent group A streptococcal (GAS) infection:
1. Scarlet fever.
2. Positive throat swab culture for GAS ( rarely positive).
3. Raised ASO (antistreptolysin O) titer and other anti-streptococcal Abs e.g. anti
DNase B antibodies.
3
Diagnosis of Rheumatic fever:
The diagnosis of acute RF made if the patient have 2 major criteria or 1 major and 2
minor criteria PLUS the evidence of recent GAS infection.
Recurrent RF diagnosed by presence of 3 minor criteria plus evidence of recent GAS
infection.
There are THREE conditions in which the diagnosis of RF done without strict adherent
to Jones criteria, these are:
1. When the chorea is only the major manifestation of RF.
2. When the indolent carditis is the only manifestation.
3. In limited number of patients with recurrent RF in high risk population.
Treatment of RF:
1. General measures: bed rest and closed monitoring for evidence of carditis.
2. Antibiotics therapy: It should be started regardless to the throat swab culture results
by given 10 days course of oral penicillin or amoxicillin or single I.M. injection of
benzathin penicillin G to eradicate GAS from URT.
If the patient is allergic to penicillin give 10 days course of erythromycin or 5 days
course of azithromycin or clindamycin.
3. Anti-inflammatory therapy:
Anti-inflammatory drugs (aspirin or corticosteroid) should be delayed if arthralgia or
atypical arthritis is the only manifestation of RF because premature treatment with one
of these drugs may interfere with the development of characteristic migratory
polyarthritis and obscure the diagnosis of acute RF.
Acetaminophen (paracetamol) can be used for treatment of pain and fever while patient
observed for more definite signs of acute RF.
Oral salicylate (aspirin): indicated for patient with typical migratory arthritis or those
with carditis without cardiomegaly or congestive heart failure.
Dose: 50-70 mg\kg\day in 4 divided doses orally for 3-5 days followed by 50 mg\kg\day
in 4 divided doses orally for 3 wk then half of the dose for another 2-4 wk.
Corticosteroid (prednisone): indicated in patients with carditis associated with
cardiomegaly and\or congestive heart failure.
Dose: 2mg\kg\day in 4 divided doses orally for 2-3 wk followed by half of the dose for
another 2-3 wk and then gradual tapering of the dose by 5 mg\day every 2-3 days.
When prednisone is being tapered, the aspirin at dose of 50 mg\kg\day in 4 divided
doses orally should be given for 6 wk to prevent rebound of inflammation.
4. Treatment of congestive heart failure: by digoxin, fluid and salt restriction, diuretics
and oxygen.
5. Treatment of Sydenham chorea: Phenobarbital is the drug of choice. If it is
ineffective, then haloperidol or chlorpromazine should be used as alternative therapies.
Anti-inflammatory agents are not indicated in treatment of chorea because it often
occurs as isolated manifestation after resolution of acute phase of disease, but some
patients may get benefit from a few weeks course of corticosteroid if the other drugs are
ineffective in treatment of chorea.
4
Prevention of RF:
A. Primary prevention: Is prevention of first attack of acute RF by identification and
eradication of GAS pharyngitis (as in the treatment of RF).
B. Secondary prevention: Is prevention of recurrent attacks of RF in patients with
previous attack of acute RF by continuous prophylactic antibiotic therapy to prevent
any GAS infection of URT.
This secondary prevention should be started as soon as the diagnosis of acute RF
made and immediately after a full course of antibiotic therapy.
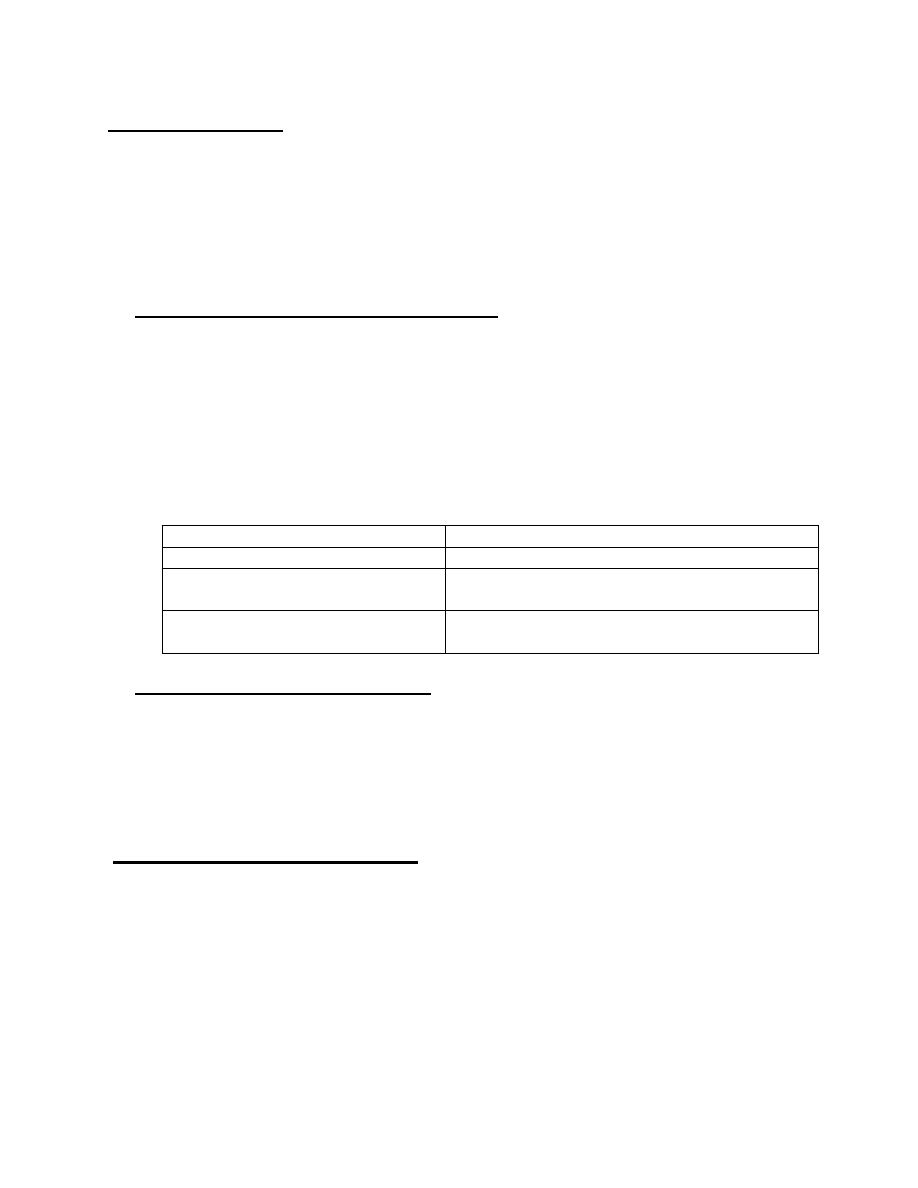
Duration of antibiotic prophylaxis therapy:
1. Patients who did not have carditis during the first attack have low risk of carditis
with recurrent RF so the prophylactic antibiotics should continue until the age of
21yr or until 5yr after the last attack of RF, whichever is longer.
2. Patients who have initial RF with carditis but without valvular heart disease
required prophylaxis for 10 years or until 21yr of age, whichever is longer.
3. Patients with carditis and Valvular heart disease in initial attack of acute RF
required continuous antibiotic prophylaxis into the adulthood (40yr) or for long
life because they are at high risk of having carditis with recurrent RF and for
additional cardiac damage.
CATEGORY
DURATION of prophylactic therapy
Rheumatic fever without carditis
5 yr or until 21 yr of age, whichever is longer
Rheumatic fever with carditis
but without valvular heart disease
10 yr or until 21 yr of age,
whichever is longer
Rheumatic fever with carditis and
persistent valvular heart disease
For adulthood (40yr), sometimes
lifelong prophylaxis
Regimen of secondary prevention:
1. Single I.M. injection of benzathin penicillin G every 4wk or every 3wk in
populations with high incidence of RF.
2. Oral penicillin V, 250 mg twice daily.
3. Sulfadiazine or sulfasoxazole once daily.
4. Macrolides (erythromycin or clarithromycin) or azithromycin are used for patients
who are allergic to penicillin and sulfonamide.
Prognosis of Rheumatic fever:
It depend on the degree of permanent cardiac damage. Cardiac involvement may
resolve completely especially in the first attack and followed by prophylactic therapy.
The severity of cardiac involvement worsens with each recurrent RF.
