
Pelvic organ prolapse (POP)
The herniation of the pelvic organs to or beyond the vaginal walls is a
common condition. Many women with prolapse experience symptoms
that impact daily activities, sexual function, and exercise. The presence of
POP can have a detrimental impact on body image and sexuality. Its
caused by injury to the muscles or tissues that support the pelvic organs.
TERMINOLOGY
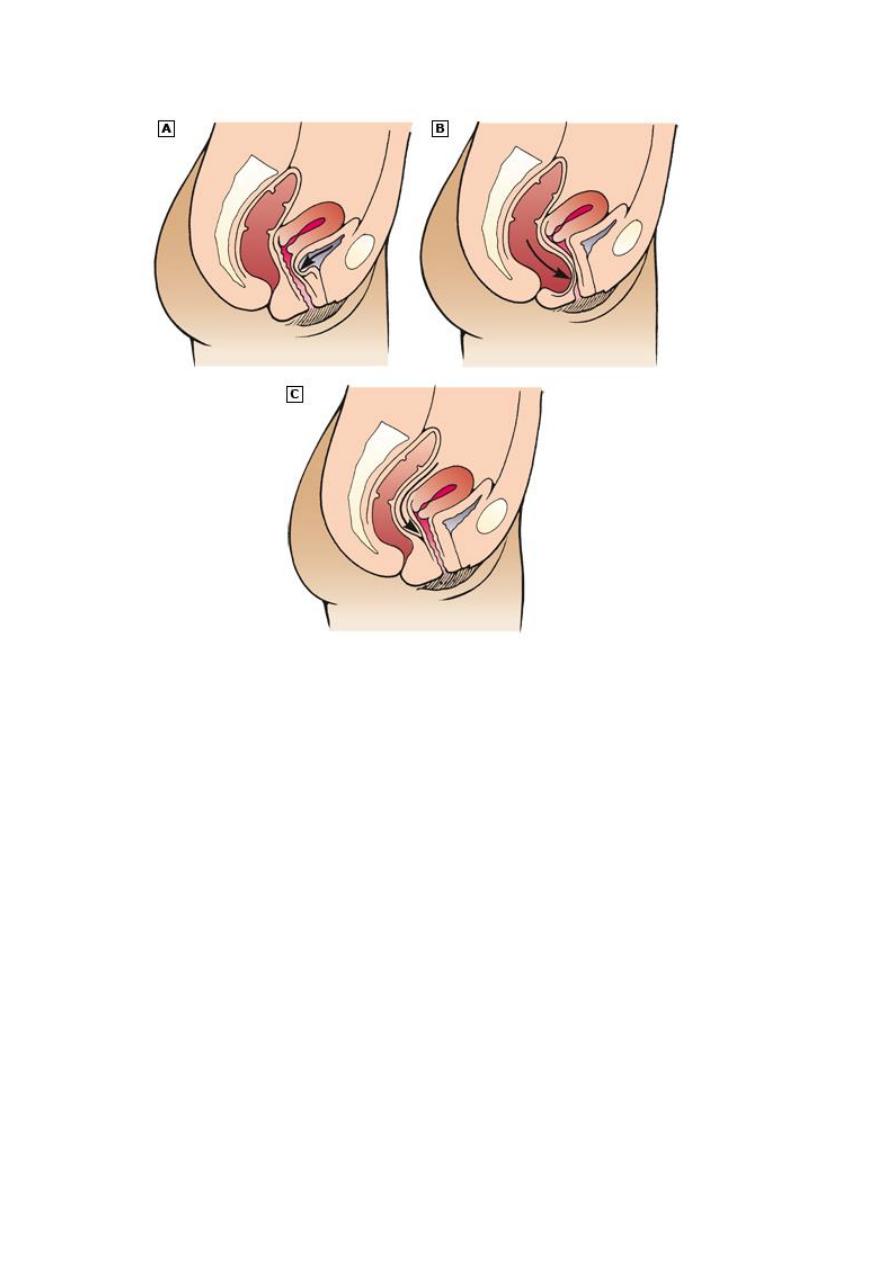
Pelvic organ prolapse (POP) – The herniation of the pelvic organs
to or beyond the vaginal walls.
Commonly used terms to describe specific sites of female genital
prolapse include:
Anterior compartment prolapse – Hernia of anterior vaginal wall
often associated with descent of the bladder (
cystocele
).
Posterior compartment prolapse – Hernia of the posterior vaginal
segment often associated with descent of the rectum (
rectocele
).
Enterocele
– Hernia of the intestines to or through the vaginal wall.
Apical
compartment prolapse (uterine prolapse, vaginal vault
prolapse) – Descent of the apex of the vagina into the lower vagina,
to the hymen, or beyond the vaginal introitus . The apex can be
either the uterus and cervix, cervix alone, or vaginal vault,
depending upon whether the woman has undergone hysterectomy.
Apical prolapse is often associated with enterocele.
Procidentia
— Hernia of all three compartments through the
vaginal introitus.
ANATOMY OF PELVIC SUPPORT
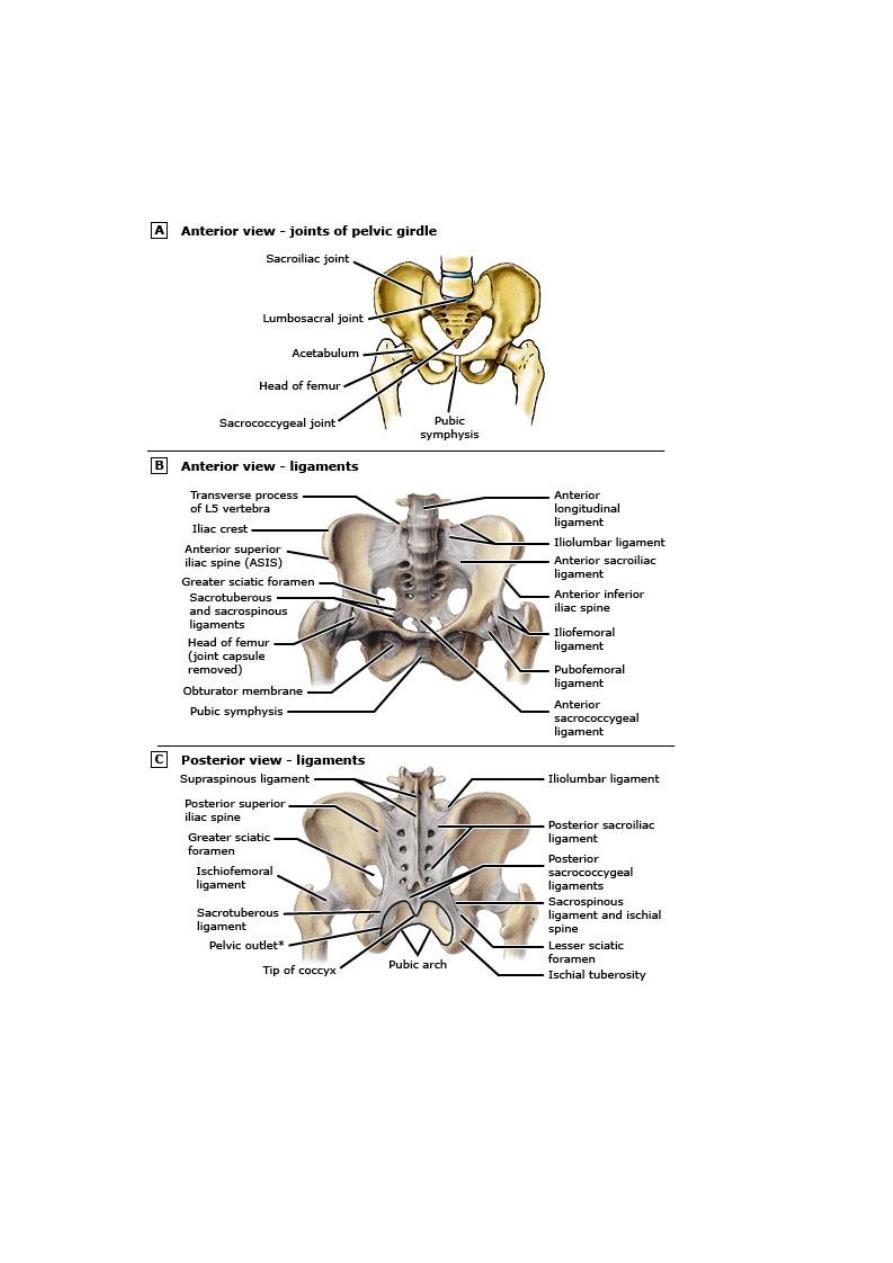
Anatomic support of the pelvic organs in women is provided by an
interaction between the muscles of the pelvic floor and connective tissue
attachments to the bony pelvis.
The levator ani muscle complex, consisting of the pubococcygeus,
puborectalis and iliococcygeus muscles, provides primary support to the
pelvic organs, providing firm, yet elastic, based upon which the pelvic
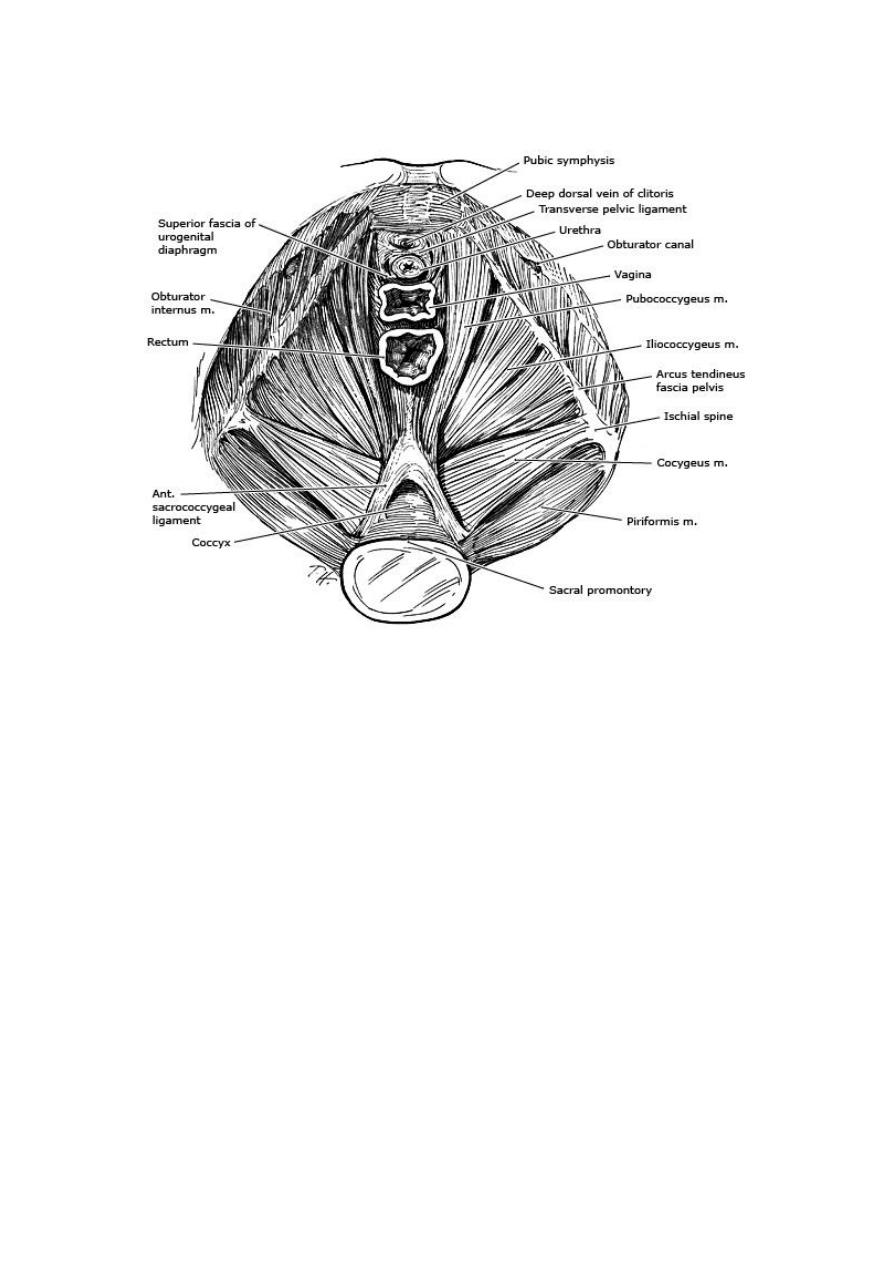
organs rest.
The endopelvic fascial attachments, in particular condensations of the
endopelvic fascia referred to as the uterosacral and cardinal ligaments,
stabilize the pelvic organs correct position so that the pelvic muscles can
provide optimal support in t
he
PREVALENCE
—It about 12-30% in multiparous, and 2% in
nulliparous.
Grading
0-
No prolapse
1-
Leading edge of prolapse str. Descend halfway to vaginal
introitus
2-
Leading edge of prolapse structure descend to vaginal
introitus
3-
Leading edge of prolapse str. Protrude up to half way outside
the vagina
4-
Leading edge protrude up to halfway outside the vagina
RISK FACTORS
— Established risk factors for POP include
parity, advancing age, and obesity
Parity — The risk of POP increases with increasing parity
Obstetric factors in addition to parity can influence the risk of
prolapse. POP can develop during pregnancy prior to delivery.
Vaginal delivery is associated with a higher incidence of POP than
cesarean.
Advancing age — Older women are at an increased risk for POP
Obesity — Overweight and obese women (body mass index >25)
have a two-fold higher risk of having prolapse than other women.
While weight gain is a risk factor for developing prolapse, it is
controversial whether weight loss results in prolapse regression.
However, there are reports of POP regression in women after
bariatric surgery.
Hysterectomy — Hysterectomy is associated with an increased risk
of apical prolapse. Factors that may influence the risk of prolapse
after hysterectomy are age and the surgical route (abdominal or
vaginal).
Race and ethnicity — Data suggest that African-American women
have a lower prevalence of symptomatic POP than other racial or
ethnic groups in the US.
Other risk factor — chronic constipation is a risk factor for POP,
likely due to repetitive increases in intraabdominal pressure, the
risk of prolapse is increased in women with occupations that
involve heavy lifting.
Some connective tissue disorders (eg, Ehlers-Danlos syndrome) or
congenital abnormalities (eg, bladder exstrophy) contribute to POP.
Endocrine (menstrual cycle, pregnancy and menopause) are the
most significant endocrine event effect pelvic floor fascia, that is
why POP more evident in mense, pregnancy(effect of
progesterone)
PREVENTION
— Prolapse prevention strategies have not been
extensively studied. Although vaginal childbirth is associated with
an increased risk of prolapse, it is unclear that cesarean delivery
will prevent the occurrence of prolapse.
Prevention of progression of prolapse has not been well studied.
Some data suggest that women with prolapse who use a vaginal
pessary have a lower stage of prolapse on subsequent exams.
Interventions such as weight loss, treatment of chronic
constipation, and avoidance of jobs that require heavy lifting are
potential interventions to avoid the development or progression of
POP and deserve further investigation.
CLINICAL MANIFESTATIONS
Patients with POP may present with symptoms related specifically to the
prolapsed structures, such as a bulge or vaginal pressure or with
associated symptoms including urinary, defecatory or sexual dysfunction.
Symptoms such as low back or pelvic pain have often been attributed to
POP.
Severity of symptoms does not correlate well with the stage of
prolapse. Symptoms are often related to position; they are often
less noticeable in the morning or while supine and worsen as the
day progresses.
Many women with prolapse are asymptomatic; treatment is
generally not indicated in these women.
Bulge or pressure symptoms — Women with POP often present
with the complaint of vaginal or pelvic pressure and/or the
sensation of a vaginal bulge or something falling out of the vagina.
Some women are able to see a protrusion of the prolapse beyond
the introitus (procidentia).
Protrusion of the vagina may result in chronic discharge and/or
bleeding from ulceration.

Urinary symptoms — Loss of support of the anterior vaginal wall
or vaginal apex may affect bladder and/or urethral function.
Symptoms of stress urinary incontinence (SUI) often coexist with
stage I or II prolapse, obstructive symptoms, incomplete bladder
empyting , urinary retention.
Women with POP have a two- to five-fold risk of overactive
bladder symptoms (urgency, urge urinary incontinence, frequency)
compared with the general population.
In addition, some women with POP experience enuresis or
incontinence with sexual intercourse.
Defecatory symptoms — the most common bowel symptom
associated with prolapse is constipation. Other defecatory
symptoms include fecal urgency and fecal incontinence and
obstructive symptoms, eg, incomplete emptying, straining, or the
need to apply digital pressure to the vagina or perineum (splint) to
completely evacuate; some women report fecal incontinence during
sexual intercourse.
Effects on sexual function — Prolapse does not appear to be
associated with decreased sexual desire or with dyspareunia,
DIAGNOSIS AND CLASSIFICATION
POP is diagnosed using pelvic examination. A medical history is
also important to elicit prolapse-associated symptoms, since
treatment is generally indicated only for symptomatic prolapse, the
Pelvic Organ Prolapse Quantitation (POPQ) system has become
the most commonly used prolapse staging system.
NATURAL HISTORY — Prolapse has traditionally been regarded
as a progressive disease, with mild prolapse leading to more
advanced disease. However, data suggest that the course is
progressive until menopause, after which the degree of prolapse
may follow a course of alternating progression and regression.
Examination
Pelvic examination by sims speculum for assesment of pop
grading.
APPROACH TO MANAGEMENT

Indications for treatment — Treatment is indicated for women with
symptoms of prolapse or associated conditions (urinary, bowel, or
sexual dysfunction). Obstructed urination or defecation or
hydronephrosis from chronic ureteral kinking are all indications for
treatment, regardless of degree of prolapse.
Treatment is generally not indicated for women with asymptomatic
prolapse.
Establishing patient goals — Treatment is individualized
according to each patient’s symptoms and their impact on her
quality of life.
Management options — Women with symptomatic prolapse can be
managed expectantly, or treated with conservative or surgical
therapy
The choice of therapy depends upon the patient’s preferences, as
well as the ability to comply with conservative therapy or tolerate
surgery. Some data suggest that age, the degree of POP as
measured by descent of leading edge of prolapse, preoperative
pelvic pain scores, and prior prolapse surgery are independently
associated with treatment choices.
Expectant management — Expectant management is a viable
option for women who can tolerate their symptoms and prefer to
avoid treatment.
Women with symptomatic or asymptomatic prolapse who decline
treatment, particularly stage III or IV, should be evaluated on a
regular basis to assess for the development or worsening of urinary
or defecatory symptoms.
Conservative management — Conservative therapy is the first line
option for all women with POP, since surgical treatment incurs the
risk of complications and recurrence. However, prolapse is
typically a chronic problem, and many women ultimately prefer
surgery to conservative therapy since successful surgery does not
require ongoing maintenance.
Vaginal pessary — the mainstay of non-surgical treatment for POP
is the vaginal pessary. Pessaries are silicone devices in a variety of
shapes and sizes, which support the pelvic organs. Approximately
half of the women who use a pessary continue to do so in the
intermediate term of one to two years. Pessaries must be removed
and cleaned on a regular basis.

Need replacement every 6 months, shelf pessary used in
hysterectomised patient, pt. do not desired sexual function and
incase of vaginal ulceration and infection.
Indication for pessary: pt. wish, as therapeutic test, child bearing
not completed, medically unfit, during and after pregnancy, while
waiting for surgery.
Pelvic floor muscle exercises — pelvic floor muscle exercises
(PFME) appear to result in improvements in POP stage and POP-
associated symptoms.
Estrogen therapy — There are few data about the use of estrogen
therapy for treatment of symptomatic POP. Use of estrogenic
agents (raloxifene) appears to be associated with a decrease in
undergoing surgery for POP.
Surgical treatment — Surgical candidates include women with
symptomatic prolapse who have failed or declined conservative
management of their prolapse. There are numerous surgeries for
prolapse including vaginal and abdominal approaches with and
without graft materials.
Surgical prognosis depends upon the severity of symptoms, extent
of the prolapse, physician experience, and patient expectations.
Surgery has traditionally been associated with a
recurrence/reoperation rate of up to 30%.
Utero vaginal prolapse
If the woman not wish to conserve her uterus: vaginal hysterectomy
with adequate support of the vault to the uterosacral ligament is
sufficient.
If wish to conserve uterus 1- Manchester op.
2- Sacrohysteropexy
Vault prolapse
sacrocolpopexy, sacrospinous ligment fixation
Cystourethroceole
(anterior colporphy) done if no concurrent stress
incontinence.
Rectocele
(posterior colporaphy)
Enterocele
the peritoneal sac contain small bowel should be excised,
POD closed by approximating the peritoneum and utero sacral
ligament.

Colpocleisis
closure of vagina
