Ovarian cancer
Dr .huda adnanc.a.b.o.g.
Epidemiology
Median age at diagnosis 63Life time risk 1/70.
Fourth commonest cause of cancer death in women in developed countries
>60% of women diagnosed with Stage III/IV
symptoms of abdo pain, bloating, distension, constipation, back pain usually happen in advanced stage
To date, no mortality benefit demonstrated with CA125 and TVUS screening.
Subtypes
Epithelial• High grade serous 75%,Mucinous 10%,Endometrioid 10%, Clear cell,Low grade serous.
Germ cell tumour
Dysgerminoma ,endodermal sinus tumour, embryonal cell carcinoma,choriocarcinoma.
Sex cord tumour
granulosa cell tumour, sertoli ledyg cell tumour, gynandroblastoma.
Metastasis from other site called krukenberg especially from stomach.
Epithelial ovarian cancer
Epithelial ov. Cancer is the leading cause of death from gynecological cancer. It derived from ceolomic epithelium of the ovary, fallopian tube, and peritoneum. It is hetrogenous group of neoplasm differ in histological and molecular feature and clinical behavior(low malignat potential, frankely invasive malignant neoplasm).
15-20% of all epithelial neoplasms are LMP, type I tumor low grade(serous, mucinous, endometriod,clear cell,and transitional Brenner tumor) compremise 25% of malignant ov. Cancer.
Type II include high grade serous, endometriod, malignant mixed mesodermal and undifferentiated carcinomas.
Serous tr. 1/2 of epith. tr. Have serous histology; psammoma bodies are pathognomonic of ov. Type serous carcinoma. Mostly present in advance disease, can be bilateral).
Endometroid tumor 2nd. Common is associated with endometriosis, endometrial cancer. It vary in size 12cm-25 cm fleshy ii k.k.
Mucinous tr. 15% of epith. Ovarian cancer.majority benign, 15% of LMP, only 3.5% malignant.it grow quite large reaching 30 cm and wt 40 kg. malignant mucinous bilateral in 10-20%, benign is unilateral.
pseudomyxoma peritonei is clinical term used to describe abundant of mucoid or gelatinous material in the pelvis or abdominal cavity surrounded by thin fibrous capsules, ov. Cancer +this cond. Is always metastases rather than 1ry.
Secondary tr. Malignant tr. That metast. To ovary are bilateral (krukenberg tr.refer to metst. Mucinous-signet ring cell adenocarcinoma originate from stomach.
Germ cell tumour
These tumors comprise approximately 20 to 25 percent of ovarian neoplasms overall, but account for only about 5 percent of all malignant ovarian neoplasms .Ovarian germ cell tumors arise primarily in young women between 10 and 30 years of age and represent 70 percent of ovarian tumors in this age group . Dysgerminoma is the most common type.DYSGERMINOMA — Although dysgerminomas are relatively uncommon among all ovarian tumors (accounting for only about 2 percent), they account for 32.8 percent of malignant OGCTs
The majority of cases (75 percent) arise in adolescents and young adults, in whom they account for about one-third of all ovarian malignancies .Because of their predilection for young women, they are one of the more common ovarian malignancies detected during pregnancy. Nevertheless, dysgerminoma can occur at any age.
Lymphocytic infilteration is charecteristic on histopathology.
Clinical manifestations
The growth of dysgerminomas is usually rapid; as a result, patients often present with abdominal enlargement and pain due to rupture with hemoperitoneum or torsion. Menstrual abnormalities may occur if the tumor is hormonally active.Seventy-five percent of women with dysgerminomas present with stage I disease the contralateral ovary is involved in 10 to 15 percent .Bilateral ovarian disease is more common with dysgerminoma than with any other malignant OGCT.
Surgery is performed for definitive diagnosis, staging, and initial treatment. For a unilateral tumor confined to the ovary without capsular involvement or rupture (stage IC), simple salpingo-oophorectomy is curative in over 95.
Granulosa cell tr.
They are solid, but as they grow larger they develop many small cystic spase, cut surface k.k yellow tinge bec, lipid content. Histology call-exner body, tr. Usually occur at late reproductive age or after menopause but can seen at any age. Both granulosa, thecoma produce estrogen.
If before puberty/ precocious puberty.
Reoroductve life/small amount of E cycle remain regular, discovered if complication occure like tortion.
If E is high ther will be menstrual irregularity, amenorrhea.
After menopause/ post menopausal bleeding, 4% endometrial ca., breast enlargement.
Ovarian Cancer Risk Factors
50 years of age or olderFamilial factors
Family history of breast, ovarian, or colon cancer ?3x baseline risk
Personal history of breast or colon cancer
Familial cancer syndrome (10%)
BRCA (breast cancer) gene mutation
Hereditary nonpolyposis colon cancer (HNPCC)
Other potential risk factors
Early menarche (younger than 12 years of age)
Late menopause (older than 52 years of age)
Hormone replacement therapy
First pregnancy at older than 30 years of age
Infertility, endometriosis
(fertility Rx does not increase risk)
Certain factors may reduce a woman's risk of developing ovarian cancer :
Taking birth control pills for more than 5 years
Breastfeeding
Pregnancy
A hysterectomy or a tubal ligation
Prophylactic oophorectomy in case of BRCA mutation.
Lifetime Risk of Cancers Associated With Specific Genes
• Cancer, %• BRCA1
• BRCA2
• MMR*
• Breast
• 35-60
• 30-55
• 0
• Ovarian
• 35-45
• 15-25
• 6-20
• Endometrial
• 0
• 0
• 40-60
*MMR (mismatch repair) = HNPCC.
Chen S, et al. J Clin Oncol. 2007:25:1329-1333. Aarnio M, et al. Int J Cancer. 1999:81:214-218.
Red Flags for Cancer Susceptibility: BRCA1/BRCA2 screening indication:
Multiple family members with ovarian or breast cancer
Age of onset of breast cancer
Younger than 50 years of age (premenopausal)
Bilateral breast cancer
Both breast and ovarian cancer in same patient
Ashkenazi Jewish ancestry (2% chance of BRCA)
Male breast cancer
Ovarian Ca screening
Major organisations do not recommend ovarian cancer screening:Poor understanding of natural history
Poor performance of current test in detecting early stage disease
No survival benefit demonstrated even in ‘high risk grp”
Potential for harm
Genetic study remains the standard of care for BRCA carriers and reduces risk of OC by 75-96%.
Ovarian cancer screeningin high risk group by annual transvaginal ultrasound and serum CA125.
Sign and symptoms
Ovarian ca. previously called a silent killer without appreciable signs or symptom until advanced disease is obvious clinically.Commonly increase abdominal size, bloating,abdominal or pelvic pain. urinary urgency,frequency, fatigue,upset stomach, indigestion, inability to eat normally, constipation and back pain.pain during sex. Abnormal vaginal bleeding rarely occur menstrual changes, nausea, vomiting or intestinal obstruction, weight loss.
Urological symptom such as urgency, frequency.
Physical examination
A pelvic-abdominal mass is palpable in most patients with ovarian cancer, malignant tumor is tend to be solid, nodular, fixed, but no pathognomonic sign distinguish these growth from benign tumor. Rectovaginal exam should be performed.
The presence of fluid wave or flank bulging suggests the presence of ascites dx. of ovarian ca. until prove otherwise. In advance disease upper central abdominal mass signifying omental caking.
Auscultation of the chest (malignant pleural effusion).
Palpation of L.N supraclavicular, inguinal L.N.
Breast and rectum exam to assess tumor originated from these organs.
laboratory investigations
1-CBP thrombocytosis2- Electrolyte hyponatremia
3- Serum CA125 is glycoprotein not produce by normal epithelium but produced by benign and malignant tumor normal value less than 35 ml unit /ml.
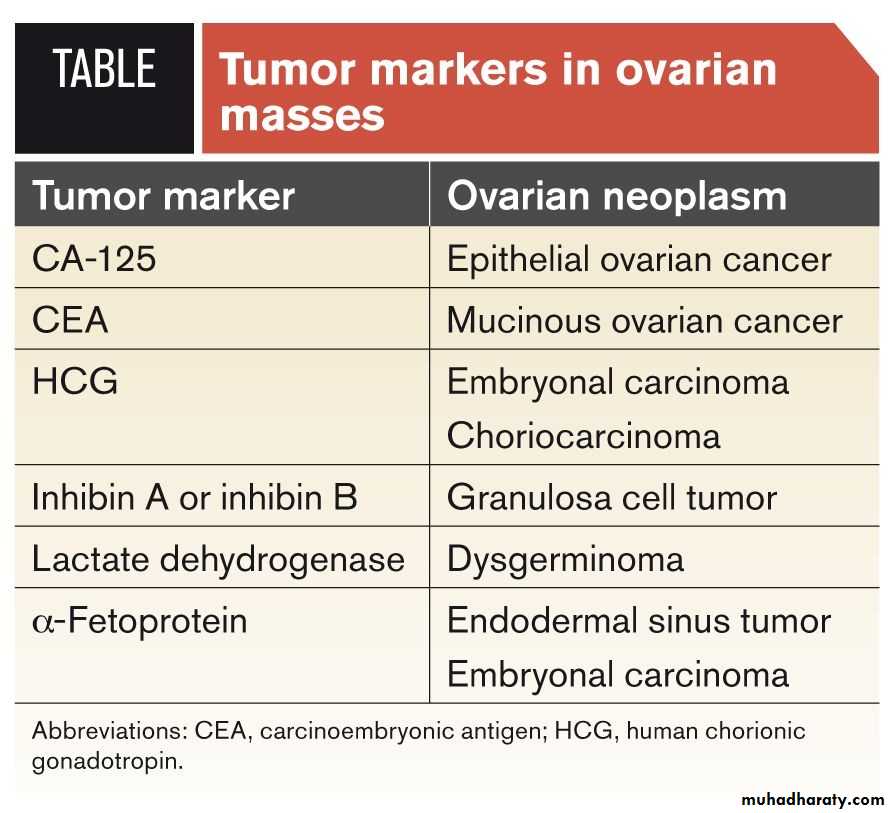
Half of stage 1 ovarian ca. normal value (false negative), false positive in PID, endometriosis, fibroid, pregnancy, menstruation. Antigen 19-9 in mucinous tr. And CEA, AFP,LDH, HCG, inhibin , estrogen and testosterone .
Imaging
A-sonography TVS, malignant multiloculated, solid, or echogenic, large than 5cm. thick septa, area of nodularity, papillary projection, neovascularity by Doppler flow. Ascites is easily detected.B- Radiography CXR (pleural effusion, lung metastases).
C- CT scan do not detect small ovarian tumors see larger tumor and may able to see if tumor is gowing into near by structures, and enlarge L.N. In advance disease (detect tr. In liver, retroperitoneal, omentum, abdomen--) and guide surgical cytoreduction.
D- MRI, PET, bone scan of little benefit.
E- Barium enema X-ray to see if the cancer invaded colon or rectum, rarely used now colonoscopy instead can be used.
Risk of malignancy indexfor any ovarian mass we can calculate the risk of malignancy index byca125 *menopausal status * ultrasonic featurespremenopause give 1, post menopause give 3ultrasonic features give one for each multilocular,solid component, ascites, metastasis, bilateral. If no any sign give 0, if 1 give 1, if 2-5 give 3.low risk (3%) if RMI < 25mod. Risk (20%) if RMI 25-250High risk (>75%) if RMI >250
Stage at diagnosis and 5-yr survival
• Stage I Confined to the Ovary 20% 85%
• IA Growth limited to one ovary, no ascites, capsule intact, no surface tumor extension
• IB Same as IA but involves both ovaries
• IC IA or IB but with positive washings or ruptured capsule
• Stage II Extends to True Pelvis 5% 60%
• IIA Involves fallopian tube or uterus
• IIB Extension to other pelvic tissues
• IIC Either IIA or IIB but with positive washings or ruptured capsule
• Stage III Extends Beyond the True Pelvis 58% 26%
• IIIA Tumor limited to true pelvis but microscopic positive biopsy outside the pelvis
• IIIB Abdominal implants up to 2 cm
• IIIC Positive lymph nodes or abdominal implants > 2 cm
• Stage IV Distant Disease 17% 12%
Stage at diagnosis 5-yr OS
Treatement
After the diagnostic tests are done, your cancer care team will recommend 1 or both treatment options.Surgery
Chemotherapy
Early stage disease (stage 1a, stage 1b )grade 1 managed by debulking suregery include bilateral salpingoophorectomy plus total abdominal hysterectomy plus infracolic omentectomy plus systemic pelvic lymphadenectomy , ascitic fluid for cytology and removal of any visible deposits , no need for chemotherapy.
advanced stage disease 1a and 1b high grade and stage 1c- stage 4 managed by debulking sugery plus chemotherapy in form of 6 cycles carboplatin and paclitaxil.
No role for 2nd look surgery.
In case of recurrent disease treatement by additive chemotherapy.
Surveillance
After treatment early stage ov. Ca. followed every 2-4 m. for 1st, 2 Y. then twice/Y. for 3 Y. and then annually, by complete physical and pelvic exam, serum CA. 125, imaging.
Prognosis depends on
1-stage of disease
2- Histo. mucinous, clear cell type poor prognosis
3- Smaller disease volume prior to surgical debulking
4- Smaller residual disease following cytoreductive surgery.
5- Age at presentation.
FIGO 5 Survival
I 85
II 60
III 26
IV 10-20