Sporotrichosis
Sporotrichosis is a cutaneous infection caused by the saprophytic mold Sporothrix
schenckii. Pulmonary and hematogenous involvement is uncommon. Symptoms are
cutaneous nodules that spread via lymphatics and break down into abscesses and
ulcers. Diagnosis is by culture. Treatment is with itraconazole or amphotericin B.
(See also the Infectious Diseases Society of America’s
Sporothrix schenckii resides on rose or barberry bushes, in sphagnum moss, and in
other mulches. Horticulturists, gardeners, farm laborers, and timber workers are most
often infected, typically after minor trauma involving contaminated material. In
contrast to the other dimorphic fungi, S. schenckii is not usually inhaled but enters the
body through small cuts and abrasions in the skin.
Symptoms and Signs
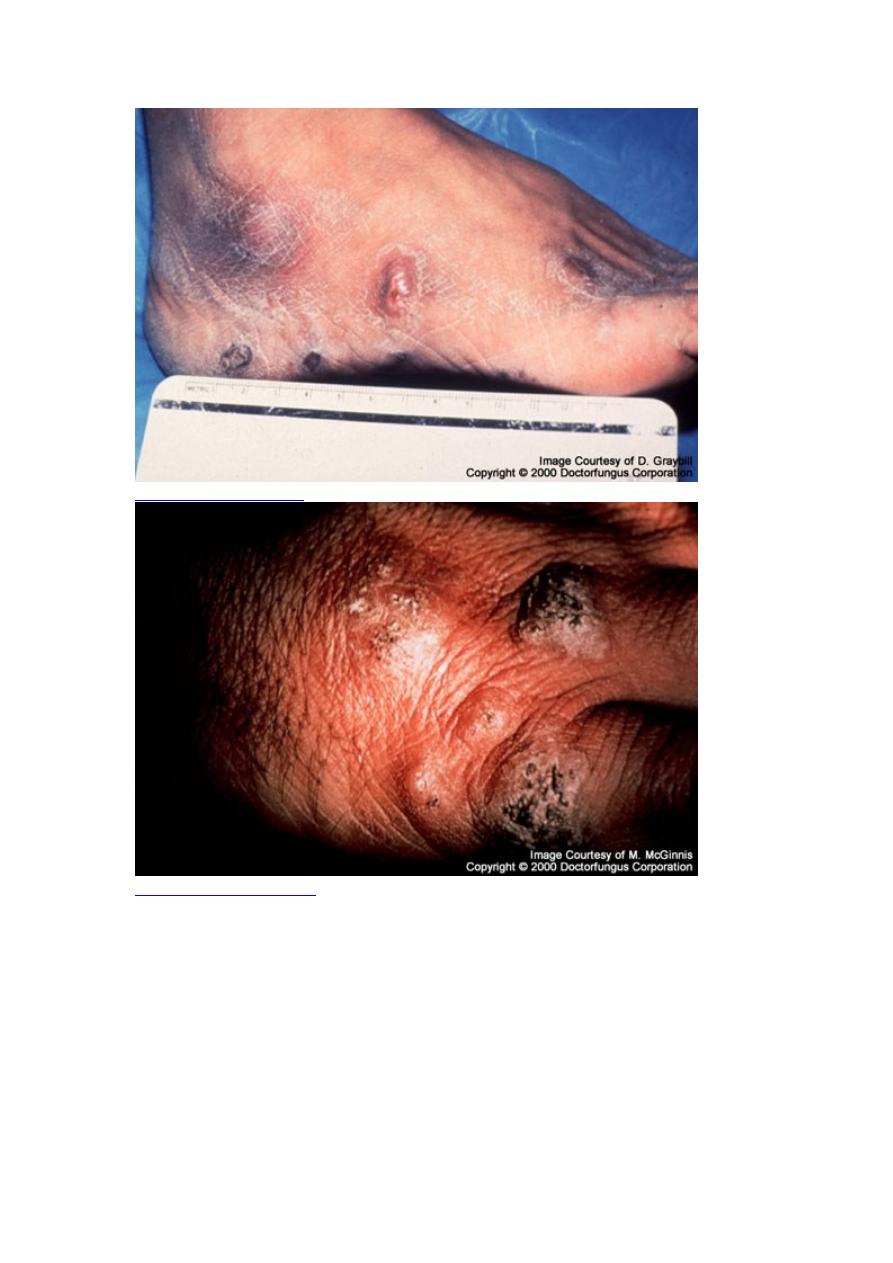
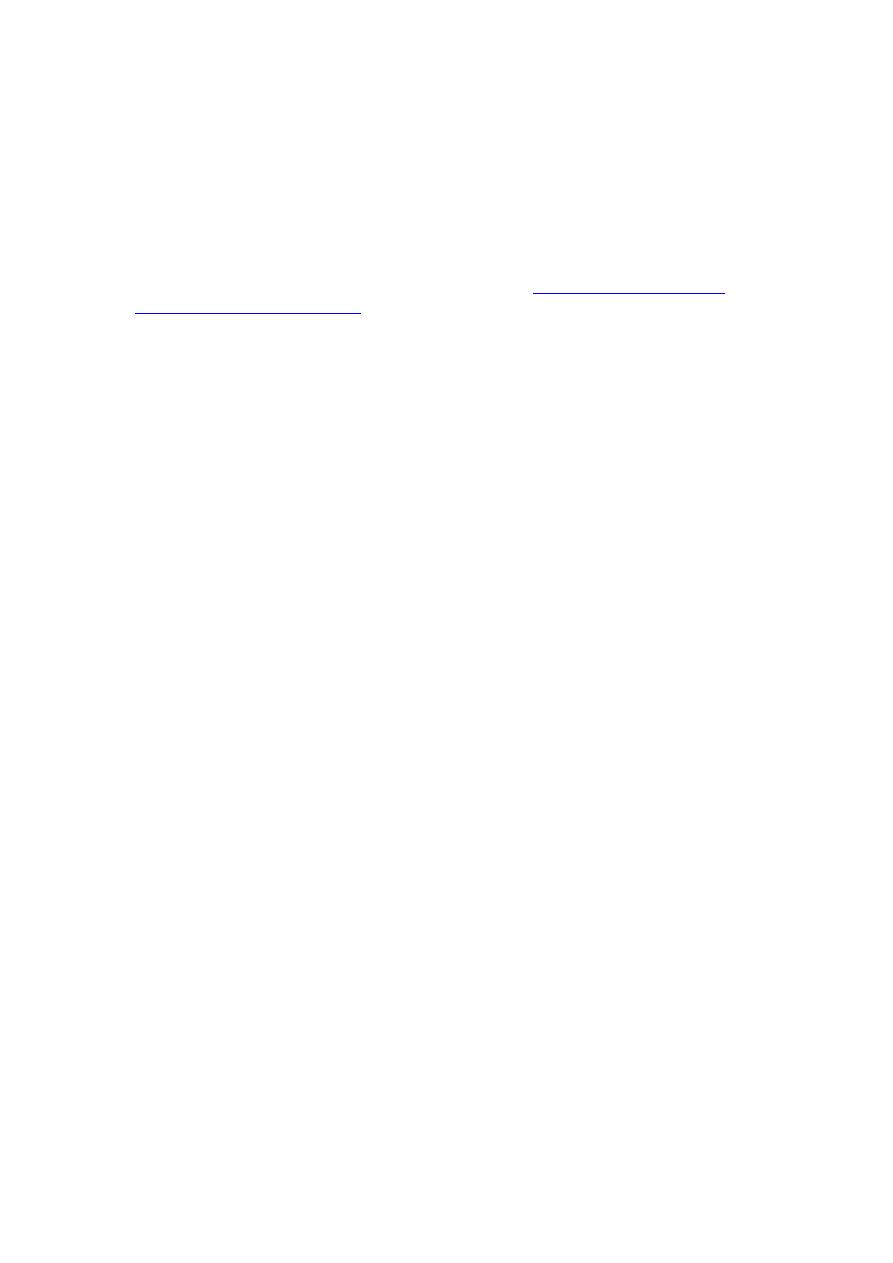
Lymphocutaneous infections are most common. They characteristically involve one
hand and arm, although they can occur anywhere on the body; primary lesions may
occur on exposed surfaces of the feet or face.
A primary lesion may appear as a small, nontender papule or, occasionally, as a
slowly expanding subcutaneous nodule that eventually becomes necrotic and
sometimes ulcerates. Typically, a few days or weeks later, a chain of lymph nodes
that drain the affected area begins to enlarge slowly but progressively, forming
movable subcutaneous nodules. Without treatment, overlying skin reddens and may
later necrose, sometimes causing an abscess, ulceration, and bacterial superinfection.
Systemic symptoms and signs of infection are notably absent.

Lymphocutaneous sporotrichosis is chronic and indolent; it is potentially fatal only if
bacterial superinfections cause sepsis.
Rarely, in patients without primary lymphocutaneous lesions, hematogenous spread
leads to indolent infections of multiple peripheral joints, sometimes bones, and, less
often, genitals, liver, spleen, kidneys, or meninges. Equally rare is chronic pneumonia
caused by inhaling spores and manifested by localized infiltrates or cavities, most
often in patients with preexisting chronic lung disease.
Diagnosis
Culture
The illness must be differentiated from local infections caused by Mycobacterium
tuberculosis, atypical mycobacteria, Nocardia, or other organisms. During the early,
nondisseminated stage, the primary lesion is sometimes misdiagnosed as a spider bite.
Culture of tissue from the active infection site provides the definitive diagnosis. S.
schenckii yeasts can be seen only rarely in fixed-tissue specimens, even with special
staining. Serologic tests are not available.
Treatment

Itraconazole
Oral itraconazole 200 mg po once/day given until 2 to 4 wk after all lesions have
resolved (typically 3 to 6 mo) is the treatment of choice. Severe infection requires a
lipid formulation of amphotericin B (3 to 5 mg/kg IV once/day); after a favorable
response, treatment is switched to oral itraconazole for a total of 12 mo of treatment.
AIDS patients may require lifelong maintenance therapy with itraconazole for
meningeal and disseminated infection. Posaconazole may have a role.