Cryptococcosis
(European Blastomycosis; Torulosis)
Cryptococcosis is a pulmonary or disseminated infection acquired by inhalation of
soil contaminated with the encapsulated yeast Cryptococcus neoformans or C. gattii.
Symptoms are those of pneumonia, meningitis, or involvement of skin, bones, or
viscera. Diagnosis is clinical and microscopic, confirmed by culture or fixed-tissue
staining. Treatment, when necessary, is with azoles or amphotericin B, with or
without flucytosine.
(See also the Infectious Diseases Society of America’s
Management of Cryptococcal Disease
Distribution of C. neoformans is worldwide; it is present in soil contaminated with
bird droppings, particularly those of pigeons. Cryptococcosis is a defining
opportunistic infection for AIDS (typically associated with CD4 counts < 100/µL),
although patients with Hodgkin lymphoma, other lymphomas, or sarcoidosis and
those taking long-term corticosteroid therapy are also at increased risk, as are
recipients of a solid organ transplant.
C. gattii is primarily associated with trees, especially the eucalyptus and, unlike C.
neoformans, is not associated with birds and is more likely to cause disease in
immunocompetent hosts. Outbreaks have occurred in the Pacific Northwest and in
Papua New Guinea and northern Australia.
Pathophysiology
Cryptococcosis is acquired by inhalation and thus typically affects the lungs. Many
patients present with asymptomatic, self-limited primary lung lesions. In
immunocompetent patients, the isolated pulmonary lesions usually heal spontaneously
without disseminating, even without antifungal therapy.
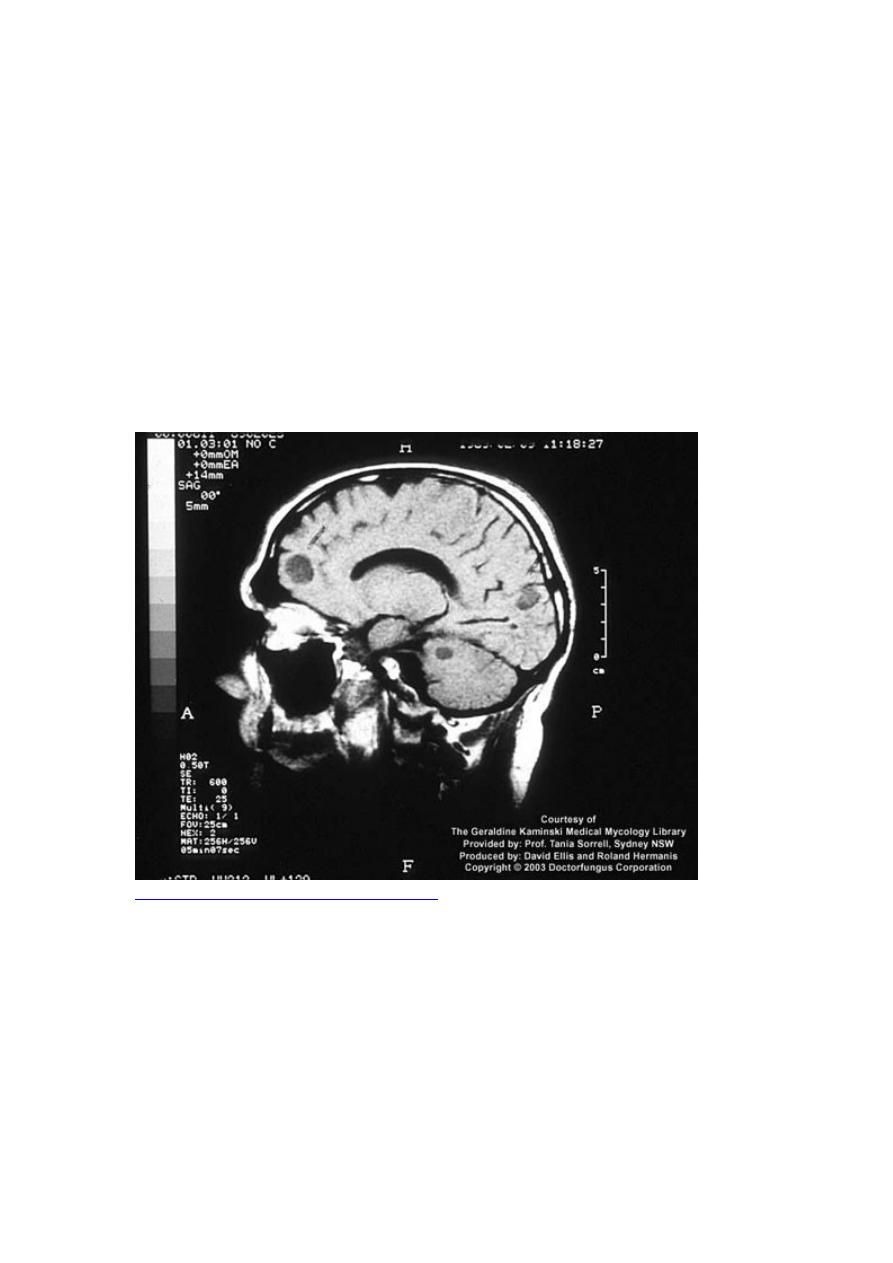
After inhalation, Cryptococcus may disseminate, frequently to the brain and
meninges, typically manifesting as microscopic multifocal intracerebral lesions.
Meningeal granulomas and larger focal brain lesions may be evident. Although
pulmonary involvement is rarely dangerous, meningitis is life threatening and requires
aggressive therapy.
Focal sites of dissemination may also occur in skin, the ends of long bones, joints,
liver, spleen, kidneys, prostate, and other tissues. Except for those in the skin, these
lesions usually cause few or no symptoms. Rarely, pyelonephritis occurs with renal
papillary necrosis.
Involved tissues typically contain cystic masses of yeasts that appear gelatinous
because of accumulated cryptococcal capsular polysaccharide, but acute inflammatory
changes are minimal or absent.
Symptoms and Signs
Manifestations depend on the affected area.
CNS
Because inflammation is not extensive, fever is usually low grade or absent, and
meningismus is uncommon. In patients with AIDS, cryptococcal meningitis may
cause minimal or no symptoms, but headache frequently occurs and sometimes slowly
progressive altered mental status. Because most symptoms of cryptococcal meningitis
result from cerebral edema, they are usually nonspecific (eg, headache, blurred vision,
confusion, depression, agitation, other behavioral changes). Except for ocular or facial
palsies, focal signs are rare until relatively late in the course. Blindness may develop
because of cerebral edema or direct involvement of the optic tracts.

Lungs
Many patients are asymptomatic. Those with pneumonia usually have cough and
other nonspecific respiratory symptoms. However, AIDS-associated cryptococcal
pulmonary infection may manifest as severe, progressive pneumonia with acute
dyspnea and an x-ray pattern suggesting Pneumocystis infection.

Skin
Dermatologic spread can manifest as pustular, papular, nodular, or ulcerated lesions,
which sometimes resemble acne, molluscum contagiosum, or basal cell carcinoma.
Diagnosis
Culture of CSF, sputum, urine, and blood
Fixed-tissue specimen staining
Serum and CSF testing for cryptococcal antigen
Clinical diagnosis is suggested by symptoms of an indolent infection in
immunocompetent patients and a more severe, progressive infection in
immunocompromised patients. Chest x-ray, urine collection, and lumbar puncture are
done first.
Culture of C. neoformans is definitive. CSF, sputum, and urine yield organisms most
often, and blood cultures may be positive, particularly in patients with AIDS. In
disseminated cryptococcosis with meningitis, C. neoformans is frequently cultured
from urine (prostatic foci of infection sometimes persist despite successful clearance
of organisms from the CNS). Diagnosis is strongly suggested if experienced observers
identify encapsulated budding yeasts in smears of body fluids, secretions, exudates, or
other specimens. In fixed tissue specimens, encapsulated yeasts may also be identified
and confirmed as C. neoformans by positive mucicarmine or Masson-Fontana
staining.
Elevated CSF protein and a mononuclear cell pleocytosis are usual in cryptococcal
meningitis. Glucose is frequently low, and encapsulated yeasts forming narrow-based
buds can be seen on India ink smears in most patients, especially in those who have
AIDS (who typically have a higher fungal burden than those without HIV infection).
In some patients with AIDS, CSF parameters are normal, except for the presence of
numerous yeasts on India ink preparation. The latex test for cryptococcal capsular
antigen is positive in CSF or blood specimens or both in > 90% of patients with
meningitis and is generally specific, although false-positive results may occur, usually
with titers ≤ 1:8, especially if rheumatoid factor is also present.
Treatment
For meningitis, amphotericin B with or without flucytosine, followed by
fluconazole
For nonmeningeal disease, fluconazole (which is usually effective)
Patients without AIDS
Patients may need no treatment for localized, asymptomatic pulmonary involvement,
confirmed by normal CSF parameters, negative cultures of CSF and urine, and no
evidence of cutaneous, bone, or other extrapulmonary lesions. Some experts give a

course of fluconazole to prevent hematogenous dissemination and to shorten the
course of the illness. Patients with pulmonary symptoms should be treated with
fluconazole 200 to 400 mg po once/day for 6 to 12 mo.
In patients without meningitis, localized lesions in skin, bone, or other sites require
systemic antifungal therapy, typically fluconazole 400 mg po once/day for 6 to 12 mo.
For more severe disease, amphotericin B 0.5 to 1.0 mg/kg IV once/day with
flucytosine 25 mg/kg po q 6 h is given for several weeks.
For meningitis, the standard regimen is induction with amphotericin B 0.7 mg/kg IV
once/day plus flucytosine 25 mg/kg po q 6 h for 2 to 4 wk, followed by consolidation
therapy with fluconazole 400 mg po once/day for 8 wk, then maintenance therapy
with fluconazole 200 mg po once/day for 6 to 12 mo. Repeated lumbar puncture is
important to manage elevated opening pressures.
Patients with AIDS
All patients require treatment. For meningitis or severe pulmonary disease, the
standard regimen is amphotericin B 0.7 mg/kg IV once/day plus flucytosine 25 mg po
q 6 h for the first 2 wk of treatment (longer induction therapy may be needed if
clinical response is slow or cultures remain positive), followed by fluconazole 400 mg
po once/day for 10 wk total. Once induction therapy is completed, long-term
suppressive (maintenance) therapy is required. Repeated lumbar puncture is important
to manage elevated opening pressures. Patients with mild to moderate symptoms of
localized pulmonary involvement (confirmed by normal CSF parameters, negative
cultures of CSF and urine, and no evidence of cutaneous, bone, or other
extrapulmonary lesions) may be treated with fluconazole 400 mg po once/day for 6 to
12 mo.
Nearly all AIDS patients need maintenance therapy until CD4 cell counts are > 150.
Fluconazole 200 mg po once/day is preferred, but itraconazole at the same dose is
acceptable; however, itraconazole serum levels should be measured to make sure that
patients are absorbing the drug.
