Coccidioidomycosis
(San Joaquin Fever; Valley Fever)
Coccidioidomycosis is a pulmonary or hematogenously spread disseminated disease
caused by the fungi Coccidioides immitis and C. posadasii; it usually occurs as an
acute benign asymptomatic or self-limited respiratory infection. The organism
occasionally disseminates to cause focal lesions in other tissues. Symptoms, if
present, are those of lower respiratory infection or low-grade nonspecific
disseminated disease. Diagnosis is suspected based on clinical and epidemiologic
characteristics and confirmed by chest x-ray, culture, and serologic testing. Treatment,
if needed, is usually with fluconazole, itraconazole, newer triazoles, or amphotericin
B.
(See also the Infectious Diseases Society of America’s
In North America, the endemic area for coccidioidomycosis includes
The southwestern US
Northern Mexico
The affected areas of the southwestern US include Arizona, the central valley of
California, parts of New Mexico, and Texas west of El Paso. The area extends into
northern Mexico, and foci occur in parts of Central America and Argentina. About 30
to 60% of people who live in an endemic region are exposed to the fungus at some
point during their life. In the US, about 150,000 infections develop annually; over half
of them are subclinical.
Pathophysiology
Infections are acquired by inhaling spore-laden dust. Thus, certain occupations (eg,
farming, construction) and outdoor recreational activities increase risk. Epidemics can
occur when heavy rains, which promote the growth of mycelia, are followed by
drought and winds. Because of travel and delayed onset of clinical manifestations,
infections can become evident outside endemic areas.
Once inhaled, C. immitis spores convert to large tissue-invasive spherules. As
spherules enlarge and then rupture, each releases thousands of small endospores,
which may form new spherules. Pulmonary disease is characterized by an acute,
subacute, or chronic granulomatous reaction with varying degrees of fibrosis. Lesions
may cavitate or form nodular-like coin lesions.
Sometimes disease progresses, with widespread lung involvement, systemic
dissemination, or both; focal lesions may form in almost any tissue, most commonly
in skin, subcutaneous tissues, bones (osteomyelitis), and meninges (meningitis).
Progressive coccidioidomycosis is uncommon in otherwise healthy people and more
likely to occur in the following contexts:

HIV infection
Use of immunosuppressants
Advanced age
2nd half of pregnancy or postpartum
Certain ethnic backgrounds (Filipino, African American, Native American,
Hispanic, and Asian, in decreasing order of relative risk)
Symptoms and Signs
Primary coccidioidomycosis
Most patients are asymptomatic, but nonspecific respiratory symptoms resembling
those of influenza, acute bronchitis, or, less often, acute pneumonia or pleural effusion
sometimes occur. Symptoms, in decreasing order of frequency, include fever, cough,
chest pain, chills, sputum production, sore throat, and hemoptysis.
Physical signs may be absent or limited to scattered rales with or without areas of
dullness to percussion over lung fields. Some patients develop hypersensitivity to the
localized respiratory infection, manifested by arthritis, conjunctivitis, erythema
nodosum, or erythema multiforme.
Primary pulmonary lesions sometimes leave nodular coin lesions that must be
distinguished from tumors, TB, and other granulomatous infections. Sometimes
residual cavitary lesions develop; they may vary in size over time and often appear
thin-walled. A small percentage of these cavities fail to close spontaneously.
Hemoptysis or the threat of rupture into the pleural space occasionally necessitates
surgery.

Progressive coccidioidomycosis
Nonspecific symptoms develop a few weeks, months, or occasionally years after
primary infection; they include low-grade fever, anorexia, weight loss, and weakness.
Extensive pulmonary involvement is uncommon in otherwise healthy people and
occurs mainly in those who are immunocompromised. It may cause progressive
cyanosis, dyspnea, and mucopurulent or bloody sputum.
Symptoms of extrapulmonary lesions depend on the site. Draining sinus tracts
sometimes connect deeper lesions to the skin. Localized extrapulmonary lesions often
become chronic and recur frequently, sometimes long after completion of seemingly
successful antifungal therapy.
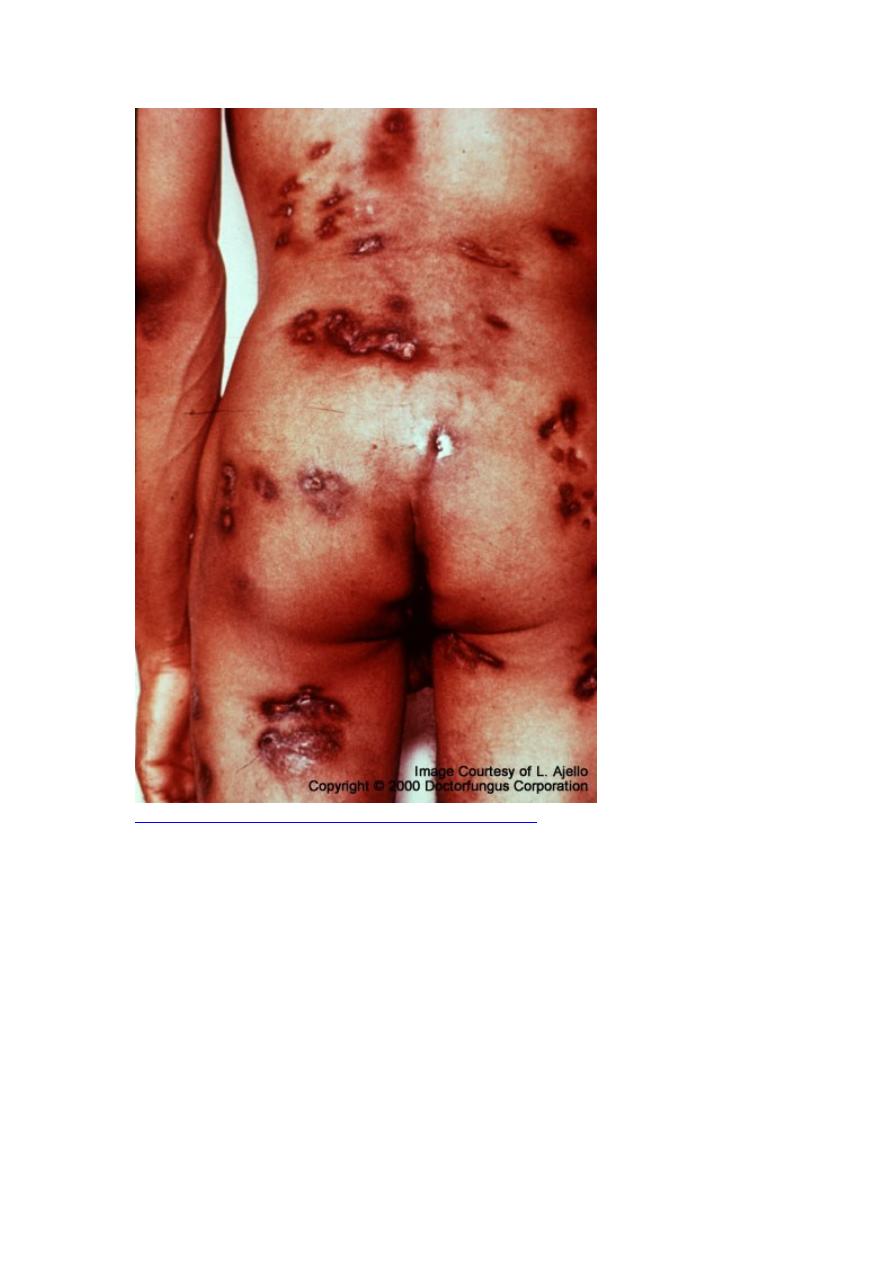
Coccidioidomycosis—Disseminated (Multiple Lesions)
Untreated disseminated coccidioidomycosis is usually fatal and, if meningitis is
present, is uniformly fatal without prolonged and possibly lifelong treatment.
Mortality rates in patients with advanced HIV infection exceed 70% within 1 mo of
diagnosis; whether treatment can alter mortality rates is unclear.
Diagnosis
Cultures (routine or fungal)
Microscopic examination of specimens to check for C. immitis spherules
Serologic testing

Eosinophilia may be an important clue in identifying coccidioidomycosis. The
diagnosis is suspected based on history and typical physical findings, when apparent;
chest x-ray findings can help confirm the diagnosis, which can be established by
fungal culture or by visualization of C. immitis spherules in sputum, pleural fluid,
CSF, exudate from draining lesions, or biopsy specimens. Intact spherules are usually
20 to 80 μm in diameter, thick-walled, and filled with small (2 to 4 μm) endospores.
Endospores released into tissues from ruptured spherules may be mistaken for
nonbudding yeasts. Because culturing Coccidioides can pose a severe biohazard to
laboratory personnel, the laboratory should be notified of the suspected diagnosis.
Serologic testing for anticoccidioidal antibodies using an immunodiffusion kit (for
IgG and IgM antibodies) and complement fixation (for IgG antibodies) are the most
useful tests. Titers ≥ 1:4 in serum are consistent with current or recent infection, and
high titers (≥ 1:32) signify an increased likelihood of extrapulmonary dissemination.
However, immunocompromised patients may have low titers. Titers should decline
during successful therapy. The presence of complement-fixing antibodies in CSF is
diagnostic of coccidioidal meningitis and is important because CSF cultures are rarely
positive. A urine antigen test that may be useful in cases of pneumonia and
disseminated infection has been developed.
Delayed cutaneous hypersensitivity to coccidioidin or spherulin usually develops
within 10 to 21 days after acute infections in immunocompetent patients but is
characteristically absent in progressive disease. Because this test is positive in most
people in endemic areas, its primary value is for epidemiologic studies rather than for
diagnosis.
Treatment
For mild to moderate disease, fluconazole or itraconazole
For severe disease, amphotericin B
Patients with primary coccidioidomycosis and risk factors for severe or progressive
disease should be treated. Treatment for primary coccidioidomycosis is controversial
in low-risk patients. Some experts give fluconazole because its toxicity is low and
because even in low-risk patients, there is a small risk of hematogenous seeding,
especially to bone or brain. In addition, symptoms resolve more quickly in treated
patients than in those who are not treated with an antifungal. Others think that
fluconazole may blunt the immune response and that risk of hematogenous seeding in
primary infection is too low to warrant use of fluconazole. High complement fixation
titers indicate spread and the need for treatment.
Mild to moderate nonmeningeal extrapulmonary involvement should be treated with
fluconazole ≥ 400 mg po once/day or itraconazole 200 mg po bid. Voriconazole 200
mg po or IV bid or posaconazole 400 mg po bid are alternatives but have not been
well-studied. For severe illness, amphotericin B 0.5 to 1.0 mg/kg IV over 2 to 6 h
once/day is given for 4 to 12 wk until total dose reaches 1 to 3 g, depending on degree
of infection. Lipid formulations of amphotericin B are preferred over conventional
amphotericin B. Patients can usually be switched to an oral azole once they have been
stabilized, usually within several weeks.
Patients with HIV- or AIDS-associated coccidioidomycosis require maintenance
therapy to prevent relapse; fluconazole 200 mg po once/day or itraconazole 200 mg
po bid usually is sufficient, given until the CD4 cell count is > 250/μL.
For meningeal coccidioidomycosis, fluconazole is used. The optimal dose is unclear;
oral doses of 800 to 1200 mg once/day may be more effective than 400 mg once/day.
Treatment for meningeal coccidioidomycosis should be given lifelong. Surgical
removal of involved bone may be necessary to cure osteomyelitis.
