3rd Stage
Brucellosis
Microbiology lecture
1
Brucellosis
History
Under the name "Malta fever", the disease now called brucellosis first came
to the attention of British medical officers in the 1850s in Malta during the
Crimean War. The causal relationship between organism and disease was first
established in 1887 by Dr. David Bruce.
Cause
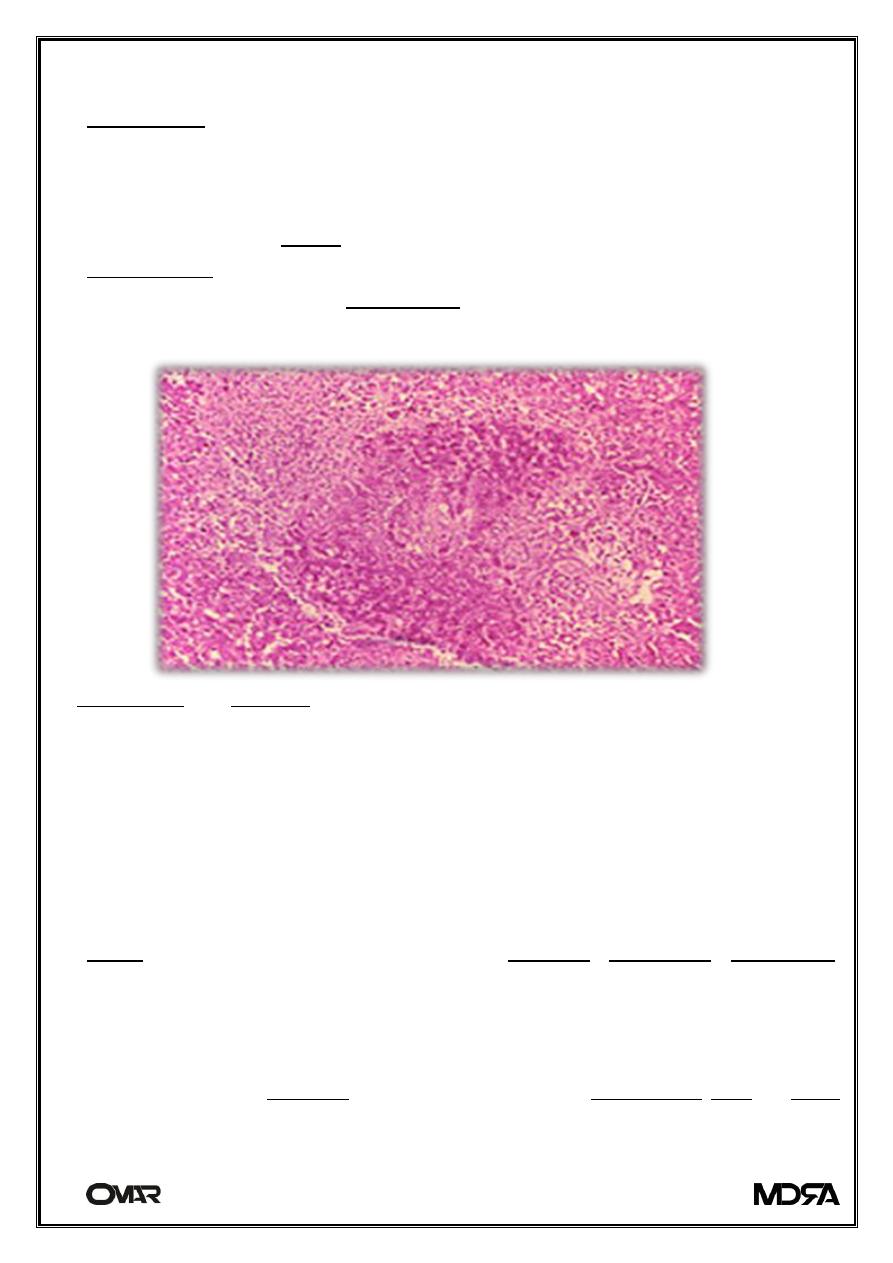
Granuloma and necrosis in the liver of a guinea pig infected with Brucella suis.
Brucellosis in humans is usually associated with the consumption of
unpasteurized milk and soft cheeses made from the milk of infected animals,
primarily goats, infected with Brucella melitensis and with occupational
exposure of laboratory workers, veterinarians, and slaughterhouse workers.
Some vaccines used in livestock, most notably B. abortus strain 19, also cause
disease in humans if accidentally injected. Brucellosis induces inconstant
fevers, miscarriage, sweating, weakness, anaemia, headaches, depression,
and muscular and bodily pain.
Brucellosis, also called Bang's disease, Crimean fever, Gibraltar fever, Malta
fever, Maltese fever, Mediterranean fever, rock fever, or undulant fever, is a
highly contagious zoonosis caused by ingestion of unsterilized milk or meat
from infected animals or close contact with their secretions. Transmission
3rd Stage
Brucellosis
Microbiology lecture
2
from human to human, through sexual contact or from mother to child, is rare
but possible.
Brucella are small, Gram-negative, non-motile, non-spore-forming, rod
shaped (coccobacilli) bacteria. They function as facultative intracellular
parasites causing chronic disease, which usually persists for life. Symptoms
include profuse sweating and joint and muscle pain. Brucellosis has been
recognized in animals.
Pathogenesis of Brucella spp.
infections are uncommon and usually mild. Most natural human infections
have been acquired through close contact with infected dogs or accidental
laboratory contamination .
In dogs, transmission of the disease usually occurs by breeding or ingestion of
contaminated placental tissues, aborted fetuses or vaginal secretions from
infected bitches.
Importantly, B. canis may be shed for long periods in semen or vaginal
secretion after occurrence of abortion . In bitches, the predominant clinical
sign is abortion after 45-55 days of gestation. Occasionally, early embryonic
death and reabsorption, or abortion 10-20 days after mating, may occur .
Infected males have unilateral or bilateral epididymitis and orchitis as the
most important clinical signs, often leading to infertility.
Semen from infected dogs usually contains large numbers of abnormal sperm
and inflammatory cells, especially during the first three months after
infection.
Chronically infected males may have azospermia, or reduced numbers of
immature sperm . In contrast to other Brucella infections, B. canis infection of
dogs results in prolonged bacteremia. Therefore, blood culture is a valuable
diagnostic approach in canine brucellosis, as opposed to other Brucella/host
combinations .
3rd Stage
Brucellosis
Microbiology lecture
3
TARGET CELLS
Brucella spp. is capable of invading and surviving in both phagocytic and non-
phagocytic host cells . Macrophages, dendritic cells (DCs), and trophoblasts
represent the major target cells for Brucella, according to clinical
manifestation of brucellosis in experimental and natural hosts, characterized
by persistent infectious in lymphoid tissues and inflammatory lesions in the
reproductive tract of pregnant females.
Bacterial entrance, survival and replication have been intensively investigated
in phagocytes, but these mechanisms are poorly characterized in
trophoblasts, which represents an important gap in our understanding of the
disease and transmission in the natural host species.
Signs and symptoms
The symptoms are like those associated with many other febrile diseases, but
with emphasis on muscular pain and sweating. The duration of the disease
can vary from a few weeks to many months or even years. In the first stage of
the disease, septicaemia occurs and leads to the classic triad of undulant
fevers, sweating (often with characteristic smell, likened to wet hay), and
migratory arthralgia and myalgia (joint and muscle pain).
Blood tests characteristically reveal leukopenia and anemia, show some
elevation of AST and ALT, and demonstrate positive Bengal Rose .
This complex is, at least in Portugal, known as Malta fever. During episodes of
Malta fever, melitococcemia (presence of brucellae in blood) can usually be
demonstrated by means of blood culture in tryptose medium or Albini
medium. If untreated, the disease can give origin to focalizations or become
chronic. The focalizations of brucellosis occur usually in bones and joints and
spondylodiscitis of the lumbar spine accompanied by sacroiliitis is very
characteristic of this disease. Orchitis is also common in men.
Diagnosis of brucellosis
· Demonstration of the agent: blood cultures in tryptose broth, bone marrow
cultures. The growth of brucellae is extremely slow (they can take up to two
3rd Stage
Brucellosis
Microbiology lecture
4
months to grow) and the culture poses a risk to laboratory personnel due to
high infectivity of brucellae.
Demonstration of antibodies against the agent either with the classic
Huddleson, Wright and/or Bengal Rose reactions, either with ELISA or the 2-
mercaptoethanol assay for IgM antibodies associated with chronic disease
· Histologic evidence of granulomatous hepatitis on hepatic biopsy
· Radiologic alterations in infected vertebrae.
Treatment and prevention
Antibiotics like tetracyclines, rifampicin, and the aminoglycosides
streptomycin and gentamicin are effective against Brucella bacteria. However,
the use of more than one antibiotic is needed for several weeks, because the
bacteria incubate within cells.
The gold standard treatment for adults is daily intramuscular injections of
streptomycin 1 g for 14 days and oral doxycycline 100 mg twice daily for
45 days (concurrently). Gentamicin 5 mg/kg by intramuscular injection once
daily for seven days is an acceptable substitute when streptomycin is not
available or contraindicated. Another widely used regimen is doxycycline plus
rifampin twice daily for at least six weeks. This regimen has the advantage of
oral administration. A triple therapy of doxycycline, with rifampin and co-
trimoxazole, has been used successfully to treat neurobrucellosis.
Doxycycline is able to cross the blood–brain barrier, but requires the addition
of two other drugs to prevent relapse. Ciprofloxacin and co-trimoxazole
therapy is associated with an unacceptably high rate of relapse. In brucellic
endocarditis, surgery is required for an optimal outcome. Even with optimal
antibrucellic therapy, relapses still occur in 5–10 percent of patients with
Malta fever.
The main way of preventing brucellosis is by using fastidious hygiene in
producing raw milk products, or by pasteurizing all milk that is to be ingested
by human beings, either in its unaltered form or as a derivate, such as cheese.
3rd Stage
Brucellosis
Microbiology lecture
5
Experiments have shown that co-trimoxazole and rifampin are both safe drugs
to use in treatment of pregnant women who have brucellosis
Prognosis
With combination drug therapy, most individuals recover in 2 to 3 weeks. Even
widespread infections may be cured. Untreated, however, the infection may
progress and increase in severity and also affect new tissues. Although
brucellosis can take a chronic form, with periods of illness alternating with
periods of no symptoms, persistent illness lasting longer than 2 months may
be due to a previously unsuspected underlying disease or a complication of
the brucellosis.
Approximately 10% of individuals may have a relapse, even after treatment is
completed. In these cases, treatment should be repeated.
This disease has a low mortality rate (lower than 2%); the most likely cause of
death is endocarditis caused by Brucella melitensis.
Biological warfare
In 1954, B. suis became the first agent weaponized by the United States at its
Pine Bluff Arsenal near Pine Bluff, Arkansas. Brucella species survive well in
aerosols and resist drying. Brucella and all other remaining biological weapons
in the U.S. arsenal were destroyed in 1971–72 when the American offensive
biological warfare (BW) program was discontinued by order of President
Richard Nixon.
