Fifth Stage
Internal Medicine - Rheumatology
Dr. Fadhil – Lecture 4
1
Management of Rheumatoid Arthritis
Possible Causes of Premature Death in RA
Chronic inflammation results in accelerated atherosclerosis leading to stroke& myocardial
infarction
• Renal disease
• Respiratory disease
• Gastrointestinal disease
• Infection
Objectives of RA Treatment
• Relieve pain
• Decrease joint inflammation
• Prevent joint destruction
• Restore function of disabled joints
• Correct deformed joints
• Maintain quality of life
Drugs for RA
Nonsteroidal anti-inflammatory drugs (NSAIDs)
Disease-modifying anti-rheumatic drugs (DMARDs)
Synthetic
Biologic
Glucocorticoids
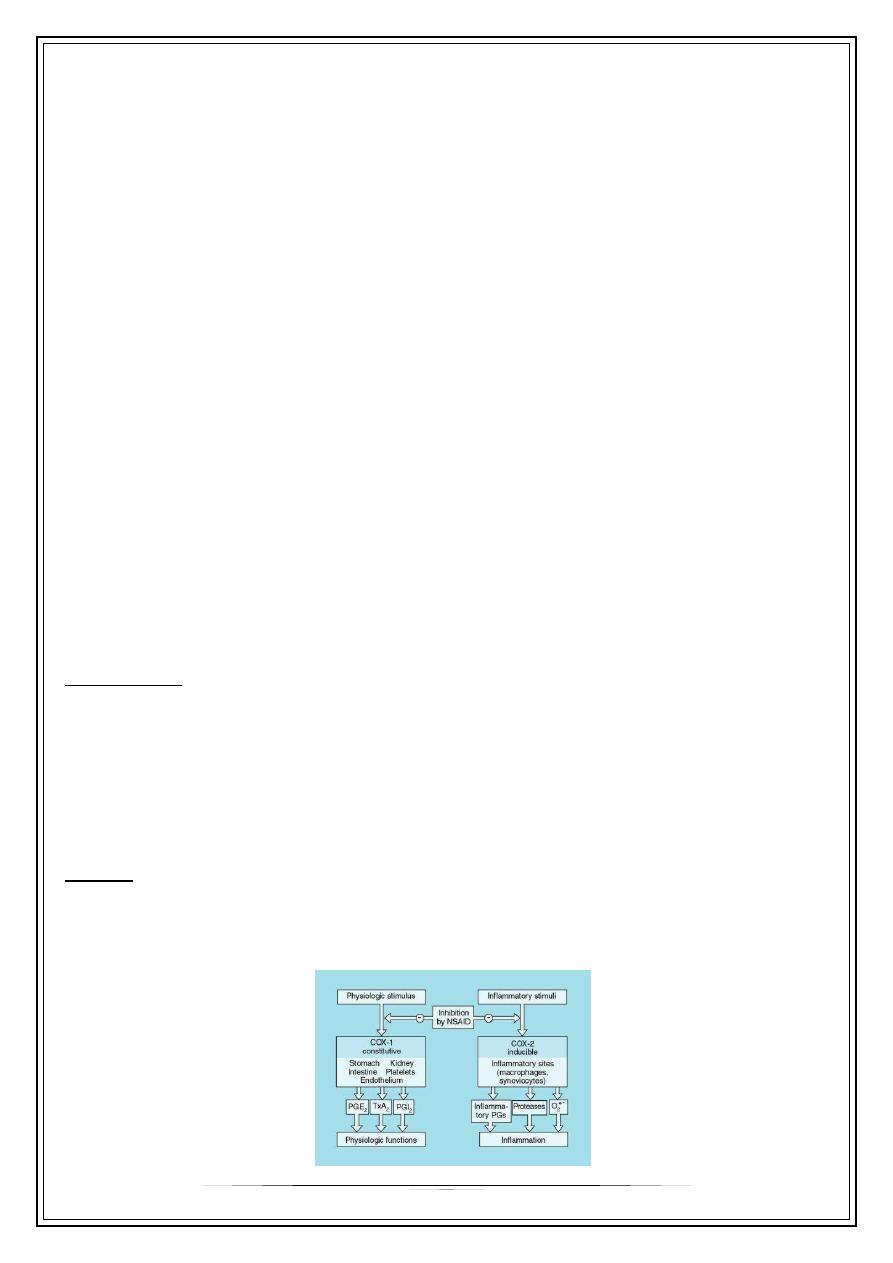
NSAIDs
Cyclo-oxygenase inhibitors
Do not slow the progression of the disease
Provide partial relief of pain and stiffness
2
Non-selective COX inhibitors
Ibuprofen
Diclofenac sodium
COX–2 inhibitors
celecoxib
COX-2 Inhibitors
COX-2 inhibitors appear to be as effective NSAIDs
Associated with less GI toxicity
However increased risk of CV events
DMARDs
Disease Modifying Anti-Rheumatic Drugs
• Reduce swelling & inflammation
• Improve pain
• Improve function
• Have been shown to reduce radiographic progression (erosions)
90% of the joints involved in RA are affected within the first year
SO TREAT IT EARLY
Some Disease-modifying Anti-rheumatic Drugs (DMARDS)
DMARD
Methotrexate
Hydroxychloroquine
Sulfasalazine
Leflunomide
Azathioprine
Cyclosporine
Gold
MONITORING
Hematologic, lung, liver (avoid alcohol)
Ophthalmologic
Hematologic, GI
Hematologic, liver
Hematologic, liver
Renal, blood pressure
Hematologic, renal
3
• DMARDs can substantially reduce the inflammation of RA, reduce or prevent joint damage,
preserve joint structure and function, and enable a person to continue his or her daily
activities. Although some DMARDs act slowly, they may allow to take a lower dose of
glucocorticoids to control pain and inflammation.
• An improvement in symptoms may require four to six weeks of treatment with
one to two months of treatment with
, and two to three months of treatment
. Even longer durations of treatment may be needed to derive the
full benefits of these drugs.
Combination therapy (using 2 to 3) DMARDs at a time works better than using a single DMARD
Synthetic DMARDs
• Methotrexate
• Sulphasalazine
• Chloroquine
• Hydroxychloroquine
• Leflunomide
Methotrexate (MTX)
Dihydrofolate reductase inhibitor
↓ thymidine & purine nucleotide synthesis
“Gold standard” for DMARD therapy
7.5 – 30 mg weekly
Absorption variable
Elimination mainly renal
Biologics
Monoclonal Antibodies to TNF
Infliximab
Adalimumab
Soluble Receptor Decoy for TNF
Etanercept
Receptor Antagonist to IL-1
Anakinra
Monoclonal Antibody to CD-20
Rituximab
Prompt introduction of DMARD therapy plays a central role.
4
The patient should be advised that this will not improve symptoms immediately, but in the
longer term there is a good chance that symptoms will come under control and joint damage
will be prevented.
If the first-choice drug fails to control disease activity, other DMARDs can be added
If adverse effects occur, the patient should be switched to another DMARD.
If disease activity persists despite an adequate trial of two DMARDs including methotrexate, anti-
TNF therapy should be considered.
Most patients also require NSAID and other analgesics.
Because of the delayed onset of action, corticosteroids are often given when DMARDs are
commenced to give symptomatic relief.
Tumor Necrosis Factor (TNF)
TNF is a potent inflammatory cytokine
TNF is produced mainly by macrophages and monocytes
TNF is a major contributor to the inflammatory and destructive changes that occur in RA
Blockade of TNF results in a reduction in a number of other pro-inflammatory cytokines (IL-1, IL-6,
& IL-8)
Side Effects
Infection
• Common (Bacterial)
• Opportunistic (Tb)
Demyelinating Disorders
Malignancy
Worsening CHF
Glucocorticoids
Potent anti-inflammatory drugs
Serious adverse effects with long-term use
To control the disease
Indications
• As a bridge to effective DMARD therapy
• Systemic complications (e.g. vasculitis)
Surgery in RA
Synovectomy of the wrist or finger tendon sheaths of the hands may be required for pain
relief or to prevent tendon rupture when medical interventions have failed.
In later stages when joint damage has occurred, osteotomy, arthrodesis or arthroplasty may
be required.
5
PROGNOSIS
average life span is reduced by 8-15 years & 5- years survival for patients with sever RA is only 50%.
40% will be disabled within 4 years……..
Factors associated with poor prognosis:
1-systemic features(wt. loss, extra-articular manifestations)
2-insidious onset
3- female gender
4-higher base line disability
5-rheumatoid nodules
6- involvement of MCP joints
7- positive rheumatoid factor
8- disease duration over 3 months
9- early bone erosions
Thank you,,,
